1. Introduction
hild Welfare South Africa, a Non-Governmental Organisation (NGO), has reported an increase in child abuse over the years in South Africa. [1] Research has shown that the country has one of the largest numbers of orphans and neglected children in the world as a result of the high prevalence of HIV AIDS. It is against this background that children who are abused end up at emergency rooms with nonaccidental injuries.
The Red Cross War Memorial Children's Hospital in Cape Town was established in 1956 and is the only paediatric hospital in Africa with a dedicated trauma unit for children under the age of 13. It is an academic children's healthcare facility offering comprehensive specialist paediatric services.The hospital is a referral centre for other hospitals in South Africa, and occasionally for hospitals in other parts of Africa. Since the establishment of a Child Abuse Management Service at the centre in the early 1980s, there has been a steady increase in patient numbers. In any given year, over a quarter of a million patients receive treatment and the trauma unit attends to about 10 000 children a year. [2]Many of these seriously injured children have come to the trauma unit for initial care. The initial recognition or suspicion of nonaccidental injury (NAI) in children is the most important step in the child protection process.
It is important that the attending physician is able to recognise the differences between accidental and non-accidental injuries. [3] Detection and diagnosis of a child's non-accidental injury depends on the clinician's ability to recognise suspicious injuries. There is a need to conduct a careful and thorough physical examination with shrewd use of essential tests. The caregiver's testimony should not conflict with the physical evidence, i.e. the characteristics of the injuries and the child's developmental capabilities. a) Background of the study During a study covering the years 1999 -2005 at the Red Cross War Memorial Children's Hospital, 99586 trauma patients were treated, of which 1037 (1.04%) were diagnosed with non-accidental injuries.The majority were male (64%) with an average age of 44.8 months. [4] According to van as: "Of the 1037 patients diagnosed with NAI, 121 (11.7%) sustained a total of 149 fractures; 21 (17.3%) with multiple fractures (16 had 2 fractures, 3 had 3 fractures and 2 had 4 fractures)." [4] He notes that the head and neck were the most frequently fractured anatomical areas (53%), followed by the upper limbs (24%) and lower limbs (18%). Only 7 fractures of the trunk were seen. Furthermore, children sustaining fractures of the head and neck were significantly younger than those sustaining fractures to other areas.
2. b) Literature Review
According to the Forensic Psychology Practice Ltd.'s Non Accidental Injury (NAI) Practitioners Portfolio, NAI is a common problem and a major cause of morbidity and mortality in children. [5] Non-accidental injury is defined as "active physical violence occurring usually within the family towards a baby or a child". [5] As such, it should be viewed as one aspect of child abuse that may occur in isolation or in combination with other forms of child abuse, including neglect, emotional abuse and sexual abuse. [6] Child physical abuse affects children of all ages, sexes, ethnicities, and socioeconomic classes. It usually takes the form of bruising (particularly on the face), bite marks, burns or scalds (particularly cigarette burns), or bone injuries (especially spiral fractures of the long bones in the limbs and skull fractures). Internal injuries may be fatal. [7] Jayakumar et al note that fractures with soft tissue injuries constitute the majority of manifestations of physical abuse in children. [8] Fracture and injury patterns vary with age and development, and NAI is intrinsically related to the mobility of the child. Furthermore, fractures and injuries to the brain and abdominal parenchyma are serious manifestations of NAI in children. [8] Considerable force is needed to cause such injuries. Careful examination often reveals several injuries of different ages, indicating long-term abuse. NAI usually has serious consequences for the child, including behavioural problems and failure to thrive.
Van As et al [4] note that although the established consensus on fracture patterns in NAI is that long bone fractures are the most frequently experienced in clinical practice, the principal finding of their study was that skull fractures were considerably more common; making up nearly 40% of all fractures. Moreover, approximately one third were reported to have been inflicted with an implement or weapon, and one-quarter of these children had multiple fractures at the time of presentation.
3. c) Motivation for the study
The Emergency Physician is often the first point of contact within the health system. [9] Failure by attending physicians to identify NAI may lead to continued infliction of the same or worse injuries to the children, resulting in death. According to Barnes et al, while it can be difficult to identify some injuries as NAI, some are obvious to detect, even without knowing the history of the patient. [10] This study will assist Emergency Physicians in the easy detection of suspicious non-accidental injuries. Quantifying the burden of non-accidental injuries also enables policymakers to make decisions about child abuse issues with supporting evidence. The study will thereby assist in policymaking and preventative programs to combat child abuse in South Africa.
4. d) Research Questions
This study seeks to answer the following questions:
? What are the patterns of injury in non-accidental injury (NAI) in children at the Red Cross War Memorial Children's Hospital? ? What are the most common types of NAI, and how are they dealt with?
e) Aims of the study
The aim of this study is to describe the pattern of injuries of children presenting to the Red Cross Children's Hospital after a non-accidental injury.
5. f) Objectives of the study
The study aims to describe the patterns of injury seen in non-accidental injury and to create and raise awareness in the general medical community, in order to ensure that the non-accidental injuries are recognised in a timely manner.
6. II.
Research Methodology a) Introduction to the research methodology Creswell (1998:17) reiterated that the nature of the research questions determine the kind of the research methodology to be used. In lieu of Creswell's dictum, this study will examine the patterns of injury in non-accidental injury (NAI) in children at the Red Cross War Memorial Children's Hospital, and it will also illuminates the most common types of NAI, and how are they dealt with in that hospital.
7. b) Study Design
This will be a retrospective descriptive study involving folder review of all the patients attended to at the Red Cross Trauma Centre, for the period 01 st January 2008 to 31 st December 2010 -covering a three year time frame to be examined.
8. c) Data collection method
Quantitative and qualitative data collection methods will be used. This will be undertaken by reviewing the Emergency Centre register and the social worker registry book to help identify patients and their folders. Furthermore, the collections of all NAI cases happened between years: 2008 -2010. Conclusions will be drawn from the information in the folders, by analysing the number of children presenting with different types of injuries, as well as the number of occurrences and the management methods used by the physician. There will be follow-up with social workers to see which cases were referred to the police. A single researcher will collect data.
9. d) Study Population
The files of children aged between 0 and 13 years and present with NAI at the Red Cross Trauma Centre are to be used in the study. Children outside this age range are not to be included in the study.
10. e) Sampling Size
All children who were present with suspected NAI during the period 01 st January 2008 to 31 st December 2010.
11. f) Inclusion Criteria
Patients between the ages of 0 and 13 years presenting to the Red Cross Children's Hospital emergency centre with a diagnosis of non-accidental injury will be included in the sample. This diagnosis must be documented in the Trauma register and the Ward registers.
12. g) Exclusion Criteria
? No definitive diagnosis of NAI.
? Any disease process other than one that can explain NAI or findings.
III.
13. Logistics
The study is estimated to cost South African Rand 4,480.00, as outlined in the budget section. The results are expected to be available for reporting within four months after the start of data collection, as outlined in the time schedule.
14. Global Journal of
15. Medical Research
Volume XIV Issue IV Version I
U TRANSPORTU U BROUGHT IN BYU U MECHANISM OF INJURY U U TRAGE PRIORITY Ambulance ? Mother ? Burn ? Red ? Private ? Father ? Assault ? Police ? Other?????????? Blunt ? Yellow ? School ? Sharp ? Other????? Other???? Green ? Not Done ? U BURN U %........ U PLACE OF OCCURRENCE Degree 1 ? 2 ?3 ? Flame ? At home ? Adm it ? Fluid ? Other home ? Dis cha rge ? Heat contact ? Public Place ? Plac e of s a fe ty ? Electrical ? School/Crèche ? Police case ? Chemical ? Sport ? Follow up b y s ocia l worker ? Explosion ? Other ? Unknown ? SEVERITYU U INVESTIGATIONSU U MANAGEMENT Mild ? CT ? Rape Kit ? Othe r??????? Moderate ? X-Ray ? EUA ? Severe ? Bloods ? POP ? Dressings ? Other?????????..Other?????????. Sutures ? U HEAD U U EYES U U BODYU Bruising to head?Peri-ocular ? Neck ? Shoulder ? Hip ? Soft tissue injury?Intra-ocular ? Chest ? Arm ? Thigh? (Retinal16. Introduction
Non-Accidental Injury (NAI) is defined as active physical violence occurring usually within the family towards a baby or a child. [1] Physical injury may be caused by burning, kicking, hitting with any object, punching or choking. [1] According to the NAI Practitioners Portfolio, NAI is common in childhood and is a major cause of morbidity and mortality. [1] NAI can occur in isolation or in combination with neglect, emotional and sexual abuse. [1]Children with NAI may present with injuries to the skeleton, soft tissues or organs. [2]They may present with clusters of injuries such as battered child syndrome, shaken infant and shaken brain syndrome (SBS) or whiplash. [3] NAI can result in behavioural problems and failure to thrive [4]. Typically, children of caregivers with mental and physical illness, alcohol and drug abuse, housing or financial problems are at higher risk of NAI. [5] NAI may be either clear cut or suspected. In clear cut cases a perpetrator is identified, or medical evidence shows ill-treatment has taken place. In these cases, a paediatrician or attending physician should conduct a medical exam and document findings. [4] In suspected NAI cases there is either no indication that an injury or other condition (e.g. unexplained failure to thrive) is caused by the ill-treatment or neglect, no perpetrator is noted, or there is no clear medical evidence. Additionally the degree or type of injury may be contradictory to the explanation given. [4] Medical tests supportive of the diagnosis of NAI have been pushed by many advocates as being proof of NAI in general, and SBS in particular; however, clear evidence for the value of this is not available. [8] The diagnosis of NAI and SBS should not rest upon a few isolated investigation results alone, but rather encompass medical examination, medical and social history, family circumstances, and interviews by experienced multidisciplinary teams. [8] Child physical abuse affects children of all demographic and socioeconomic classes. The most common types take the form of bruising, bite marks, burns or scalds, and bone injuries. [9] Instruments of abuse include blunt or sharp objects such as belts and wooden sticks, or the use of hot water or fire to inflict burns. The literature suggests that the key symptoms of NAI include bruising, bites, torn frenulum, frozen watchful eyes, altered states of consciousness, and fractures. [4] II.
17. Epidemiology
The prevalence of child sexual abuse in developing countries such as South Africa (SA) seems to be lower than that in Western countries. [8] However, this may be due to lower reporting rather than a true reflection of prevalence. In a study in 2007, NAI at the Red Cross War Memorial Trauma Unit in Cape Town was approximately 1 per 100 attendances, which is similar to studies among Western populations. [11] Incidence studies conducted with respect to cases of child maltreatment reported to official agencies in different countries proved that there were five times as many cases reported in Australia, Canada and the USA, as were finally substantiated. [10] Even though the rate per thousand children was much higher in these 3 countries than in England, there were huge similarities in the breakdown by different types of abuse. [10] A study in the USA suggested that 80% of the deaths from traumatic brain injury in children under the age of two years are due to NAI. [5] According to a 2009 study published in Clinical Psychology Review, the global prevalence of child sexual abuse is an estimated 19.7% for females and 7.9% for males. [54] The report examined 65 studies from 22 countries and it was noted that Africa had the highest prevalence of sexual abuse (34.4 %); with South Africa being the highest. America, Asia and Europe had 10.1%-23.9% while Europe had the lowest, at 9.2%. [9] In approximately 30% of the cases, the perpetrators were relatives of the child' 60% were friends of the family, babysitters, or neighbours and in 10% of cases the perpetratorswere strangers.
18. III.
19. History
Features in the history that may raise suspicion of NAI include delayed presentation of the child to the emergency centre, inconsistencies in the history; a changing explanatory story; a history of poor child supervision; poor health care history, including no or intoxication of guardian or parent on presentation; a lack of remorse on the part of the guardian towards the child's injury, and/or indifference to treatment.
20. IV.
21. Injury Patterns
Jayakumar noted that fractures with soft-tissue injuries constitute the majority of manifestations of physical abuse in children. [10] Fracture and injury patterns vary with age and development, and NAI is intrinsically related to the child's mobility. Furthermore, fractures and injuries to the brain and abdominal parenchyma are manifestations of NAI in children. [12] Considerable force is needed to cause such injuries. Careful examination often reveals several injuries of different ages, indicating long-term abuse.
A study conducted at the Red Cross War Memorial Children's Hospital, from 1999-2005, described 99 586 trauma patients treated, of which 1037 (1.04%) were diagnosed with NAI. The majority were male (64%) with an average age of 44.8 months. [11] According to van as, 11.7% of the 1037 patients sampled had a combined 149 fractures while17.3% of these had multiple fractures. [11] The head and neck area was the most frequently fractured anatomical area (53%), followed by the upper limbs (24%) and the lower limbs (18%). Torso injuries were relatively uncommon; only 7 fractures of the trunk were observed. Furthermore, children sustaining fractures of the head and neck were significantly younger than those sustaining fractures to other areas. Long bone fractures were the most frequent presentation of NAI and skull fractures were more common, representing nearly 40% of all fractures. Approximately 33% of NAI were inflicted with an object and 25% of these children had multiple fractures. This appears to be consistent with some NAI injury patterns internationally. [53] V.
22. Shaken Baby Syndrome
Shaken brain syndrome (SBS) is common in NAI cases. Infants who crawl or walk do not produce enough force in their own movements to cause fractures. [2] Typical signs and symptoms associated with SBS include: subdural haemorrhage (SDH), retinal haemorrhage (RH), and encephalopathy occurring in the context of inappropriate or inconsistent history and commonly accompanied by other apparently inflicted injuries (e.g. skeletal) [5, 12---25]. Although the literature is inconclusive, SDH is generally not expected to occur in a normal healthy infant. [6] Clinical findings not expected in a normal healthy child could be attributed to NAI, despite the absence of evidence to support that conclusion. When it comes to SBS, it is assumed that the shaking is intentional and violent, and the injury that the infant suffers is likely to be serious. Instances of retinal bleeding are assumed to be indicative of criminal abuse, unless there is evidence that suggests a medical cause. [25] VI.
23. Thermal Injuries
More than 1300 children die annually from burns in SA. [26] In SA, burns are the leading cause of non-natural death in infants and children under the age of 5. Burns are also the fourth major cause of accidental death in children in the 5 -9 year old age group, according to the National Injury Mortality Surveillance System. [26]In suspected NAI cases, physicians should look out for burn injuries inconsistent with history. Further signs to look out for in suspected NAI cases include: an unsatisfactory explanation for an injury; lack of independent mobility of the child; well-shaped injuries such as cigarette and iron burns; soft tissue injuries in areas not normally associated with accidental burns e.g. back, buttocks, back of hands and soles of feet. [27---30] Forced immersion injuries present as scalds to the lower limbs, buttocks and perineum; limbs in gloves or stockings or symmetrical distribution of injuries with sharply delineated borders. [27---30] The absence of splash marks in scald injuries (which occur when falling into the bath tub) and signs of the upper limbs restraining [27---30] may be indicative of NAI. Unexplained cold injuries, such as swollen (red) hands or feet and hypothermia are other signs to look out for in NAI [33] a) Ocular Injuries Eye injuries are common in NAI cases. [34] Due to the complexity in diagnosing these injuries, it is always helpful to have input from a specialist ophthalmologist when assessing such injuries. The commonest types of ocular injuries are retinal detachment and haemorrhage, vitreous haemorrhage and dislocation of the lens. [34] b) Abdominal Injuries In most cases, liver rupture occurs due to direct impact injury to the abdomen. This is one of the most frequent reasons for the death of children with NAI in SA. [32] Children are particularly vulnerable to such injuries due to their fragile abdominal wall muscles. In addition, it is generally easy to compress the abdominal tissues and organs against the spinal column, which leads to a variety of further injuries that also affect the small intestine. [32] It is also important to note that late clinical presentation of this type of injury is a diagnostic problem in many instances, with delays of several days being common before apparent, often severe, signs manifest themselves.
24. c) Bite Injuries
NAI in children may also be caused by human bites. [2,32] Human bites, in most cases, leave distinctive tooth marks on the victim. Correct
25. d) NAI Mimics
Identifying NAI cases is complicated by diseases, which can mimic or simulate NAI. This is most common in the case of skin lesions.
A number of physiological conditions may mimic NAI. Barnes et al note that the "growing fracture" (leptomeningeal cyst resulting from a dural tear) is not specific to NAI and may follow any diastatic fracture in a young infant [25,[33][34][35]. In some instances, subdural hematoma (SDH) may occur in normal, healthy neonates as a result of birth trauma, and even in cases of normal, uncomplicated vaginal delivery. [8, 27, 33---38]Donohoe notes that there is clear evidence that SDH can be caused by anatomical, infectious and biochemical disorders, which cause no obvious symptoms prior to intracranial bleeding, giving the appearance and impression of a normal and healthy (although not robustly healthy) infant, in spite of underlying predisposing pathology. However, these conclusions have been challenged. [6,8] Some head injuries that appear to indicate Shaken Baby Syndrome (SBS) may occur during birth and be subsequently mistaken for NAI. Intracranial haemorrhages, including SDH and retinal haemorrhages (RH), have been reported in a number of CT and MRI series of "normal" neonates. In one series this was as high as 50%. [6,[37][38][39][40][41][42] However, failure to detect scalp or skull abnormalities in imaging tests should not be interpreted as the absence of impact injury.
Medical conditions that may cause injuries that mimic NAI or cause failure to thrive include: epilepsy, thrombocytopenia and leukaemia, which may result in increased bruising, conditions predisposing fractures, e.g. osteogenesis imperfecta, metabolic bone disease in neonates, rickets, osteoporosis, copper deficiency, osteomyelitis, leukaemia and disseminated neuroblastoma. [43] It was also noted that in rare cases, subdural haematoma may be caused by Glutaricaciduria. [44] e) Sexual Abuse Sexual abuse is one of the most prominent forms of NAI. It is experienced by both sexes, though it is more common in females, and entails forced sexual acts. [33] In cases of physical abuse, specific attention should be paid to the genital areas to exclude possible associated sexual abuse. [32] It is important to note that the majority of sexual assault cases result in, among other things, sexually transmitted diseases as well as psychological trauma. [45] Feeny suggests that the examiner should especially focus on the nature of the injuries sustained, particularly in areas such as the vagina, rectum and mouth; as well as any signs of abrasions or bleeding on the part of the victim or perpetrator, because this assists in assessing the level of risk in terms of the potential transmission of HIV and hepatitis. It is also important to establish the nature of the attack, such as whether there was condom use or if ejaculation took place. Moreover, it is essential to establish whether the perpetrator used threats, violence or weapons during the attack and to get a description of the perpetrator. [45] Most physical injuries associated with sexual abuse are relatively minor, but some upper vaginal lacerations may be severe. [44 -45] Psychological symptoms are prominent in sexual assault victims. These include feelings of anger, fear, shame, embarrassment and guilt; as well as nightmares and sleep problems. [44 -45] Following an assault, patients may react by crying, becoming tense or even smiling inappropriately.
These behaviours may be manifestations of tiredness or frustration, or they may be coping mechanisms. Secondary enuresis, encopresis (defecation in inappropriate places), deliberate wetting and body-rocking are concerning behaviours suggestive of abuse in children. [31] f) Diagnostic strategies for NAI There is an on-going debate concerning which investigations provide the best result in detecting NAI in SBS. Sato et al demonstrated that there was a 50% greater rate of detection of subdural hematomas using MRI, compared with CT. [54] Although CT scan did not miss any surgically treatable injuries, the MRI scan improved the ability to detect and define intraparenchymal lesions of the brain. The two types of scan should therefore complement each other in evaluating brain injuries in infants. Given the relative insensitivity to subarachnoid blood and fractures, the MRI should be obtained 2 to 3 days after a CT scan if possible. [2] Lack of access to technology and the physical limitations of access to MRI when life support is required for critically ill infants or children may limit the usage of the MRI in practice. The radiologist therefore plays an important role in accurately identifying nonaccidental intracranial trauma.
It is important to be familiar with the spectrum of the(sometimes subtle) imaging findings one may encounter. A radiological skeletal survey of a child suspected to have NAI should include the following areas: hands, feet, long bones, skull, spine, and ribs; and these should be obtained as soon as the infant's medical condition permits. [2] Skull x-rays complement CT bone windows in the detection of skull fractures. [2] Old nall found that in studies of abused children, skull xrays were more sensitive and improved the confidence of correct diagnosis when compared with CT. [2] Multiple, bilateral and diastatic skull fractures are more likely to be non-accidental.
In shaken babies there are commonly associated patterns of skeletal injury. These include dislocations, avulsion fractures, bucket-handle and corner fractures, clavicular and humerus fractures, skull fractures as well as spinal and rib fractures. [2, 47 -48] Avulsion fractures are most common inthe spinal cord and mostly occur in other areas as a result of pulling, twisting and intense shaking. Bucket-handle fractures are mostly recognis able on a radiograph due to their bucket-handle appearance, appearing on the edge of the bone between the metaphysis and epiphysis. Lesions are suggestive of abuse. Corner fractures are avulsion fractures on the corner of the bone due to shearing of the growth plate. Depending on the angle of the X -ray, corner fractures may be confused with bucket-handle fractures.
Clavicular fractures are likely to occur if the perpetrator's thumbs press on the victim's shoulder bones during shaking. The clavicle is likely to break at mid-shaft level. Dislocations appear to be more traumatic in NAI cases. Similarly, impact fractures are equally traumatic; occurring when the infant is slammed onto hard surfaces, driving one end of the fractured bone into another.
Rib fractures are rarely seen in children because infant ribs are flexible and tend to compress with elasticity.
If there is no history of motor vehicle accidents or bone related diseases, there is reason to suspect NAI. Ribs more commonly fracture at the posterior, structurally their weakest area, during a shaking period. They may also fracture at the lateral (side) areas of the ribs. Cardiopulmonary resuscitation may also cause rib fractures. Van Rijn et al, in a 115,756 live birth study of birth trauma, showed no cases of rib fractures resulting from birth trauma, hence posterior rib fractures in young children have a high positive predictive value for NAI . [47] g) Identifying children at risk In suspected NAI cases, it is important to identify the degree of risk to the child and to take any steps necessary to protect the child. [4] NAI is an emotive issue; however, the physical and emotional safety of the child is paramount. To ensure the child is not put further at risk, documenting of the patient's history should be factual; any suggestion of abuse may result in refusal to allow the child to get treatment. [5] The available evidence will have a bearing on the course the law will take in abuse cases where NAI is identified. Parents or guardians may risk losing custody of the child, hence the need to be thorough in assessing suspected NAI victims. The evidence should be accepted in the relevant scientific community, though this can vary depending on jurisdiction. [14,13,17]Medical professionals may be acting in the interests of the child by assuming NAI, even where it has not occurred. However, there is a need to recognise the potential harm to the family and child where such assumptions prove to be incorrect. It is important to identify the perpetrator; however, this is not the task of the physician treating the child but rather the task of the social services and/or police services. Doctors treating NAI cases should also be fully aware of the legal rights of the child as well as the parents. [6] It is important that the legal procedures establish whether NAI has actually taken place and who should be held accountable. The evidence in such cases should be clear, so that the resulting judgements are also clear and based on the rule of law. Many cases of confirmed abuse, some without clear injury, may not have been investigated had it not been prompted by suspicions of medical practitioners. [6] h) Child Abuse Legislation and Support Organisations in the Western Cape
The Western Cape Province, in accordance with national priorities, has set up protocols and services to protect children against NAI. As of 2009, there were 132 Child Protection Organisations and 16 district offices in the Western Cape providing statutory social work services. [50] These include Child Welfare, Etafeni Day Care Centre Trust, Child Justice Alliance, Child Line, SOS Children's Village and Beautiful Gates, amongst others. Their duties include foster care, adoption, advocacy against commercial exploitation of children, and child labour. The Western Cape has made it a priority to train and educate social workers, child and youth care workers and NGOs to understand the contents of the Children's Act. In 2011, the Early Childhood Development (ECD) policy was amended to ensure all requirements of ECD were met; i.e. adequate nutrition, physical and health care, socio-emotional and intellectual development. [51] The new Children's Act stipulates that NGOs dealing with children should demonstrate certain levels of competency. As of August 2009, there were 35 registered children's homes, 8 shelters, 10 drop-in centres, call centres, and 30 000 children in foster care. [50] However, most NGOs operate in urban centres, neglecting the rural areas. [50] More resources are being allocated to rural areas to ensure no child is left behind. The South African's Children's Act, chapter 7 section 110, makes it mandatory for any professional dealing with children to report suspected NAI. [55] VII.
26. Conclusion
In conclusion, NAI cases are rarely clear cut and need proper investigation to warrant prosecution of the perpetrator and to determine how to treat the affected child. NAI can take many forms and qualified persons in the medical or social work fields are needed to carefully attend to each case. Methods: This is a retrospective case review study evaluating the period from 1 st of January 2008 to the 31 st of December 2010. The age group sampled was 0 -13 years. Gender, perpetrator, injury type, race, investigations, severity, place of occurrence and transportation of the patients were analysed. More detail regarding the data collection methods can be found in Appendix B.
Results: 623 folders were collected with initial diagnosis of NAI. Of these, only 522 cases of NAI were identified. The largest racial group of children in the sample was black, at 45.86%; followed by coloured (33.72%), and white (18.11%). Indian children and those whose ethnicity was not specified only made up 2.31% of the sample.
A sample of 522 was attributed to have NAI. It was noted that in 2008 there was a total of 174 NAI cases, compared to 170 in2009 and 178 in 2010. Females accounted for 61.69% (322 cases) and males for 38.31% (200 cases). Among the female cases, 60.5% were physical assaults, followed by 35% sexual abuse, 2% for genital assault, 0.5% for dog bites and 2% of unspecified cases. The highest number of NAI cases was recorded among the 5 -9 age group,comprising235 children or 45.02%; followed by the 0 -4 age group with 28.93%, and finally the 10 -13 group with 26.05%. Sexual abuse cases were prevalent in the 5 -9 group (48%), the 0-4 year old group (37.33% recorded) and the 10 -13 group, with 14.97%. Moderate cases accounted for 71.26%, mild for 21.07%, 6.32% not specified severe cases accounted for1.34% of the total. In essence, ambulances transported approximately 31% of total NAI cases, while police and schools each transported 1% respectively. 67% of cases were privately transported.
Keywords/MeSH terms: non-accidental injury, child abuse, injury mechanism, perpetrator, sexual abuse.
27. Section 1
28. What is already known on this subject?
The Emergency Physician is often the first point of contact within the health system. Failure by attending physicians to identify non-accidental injuries may lead to continued infliction of the same or worse injuries to children, resulting in death. According to Barnes et al, it can be difficult to ascertain some injuries as NAI, though some are obvious to detect even without knowing the history of the patient.
29. Section 2
30. What this study adds
The study will help Emergency Physicians in the easy detection of suspicious non-accidental injuries. Quantifying the burden of non-accidental injuries also allows for policymakers to decide on child abuse issues with supporting evidence. The study will thereby assist in policymaking and preventive programmes to combat child abuse in South Africa.
31. I.
32. Introduction
Child Welfare South Africa has reported an increase in child abuse over the years in South Africa, with most abused children being orphaned and neglected due to high HIV/Aids prevalence. [4] Many abused children end up at emergency centres with NAI.
The Red Cross War Memorial Children's Hospital in Cape Town, South Africa was established in 1956 as a highly specialised healthcare facility offering comprehensive specialist paediatric services. The hospital is predominantly a referral centre for children from the Cape Metropole region, other hospitals in South Africa and occasionally for hospitals outside South Africa. In any given year, over a quarter of a million patients receive treatment at the hospital. [5]Over the years, there has been a steady increase in referral numbers.
It is important that the attending physician be able to recognise NAI in children, [6] recognise patterns of injury and clues in history; and have knowledge of diagnostic strategies and patient management in suspected abuse cases.
33. II.
34. Aim
The aim of this study is to describe the population of children presenting to the Red Cross War Memorial Children's Hospital Trauma unit with NAI. Data analysis was used to identify the patterns and causes of injury in NAI at the Red Cross Children's Hospital. This may increase the suspicions of healthcare providers concerning these types of injuries. Non-accidental injury (NAI) is defined as active physical violence occurring usually within the family towards a baby or a child. [1] It should be viewed as one form of child abuse that may occur in isolation or in combination with other forms of child abuse, including neglect, emotional abuse and sexual abuse. [1,2] Physical injury is the most frequent consequence of abuse. Injury is commonly inflicted by burning, kicking, hitting with objects, punching or choking. [3] access to patient records was granted by the Human IV.
35. Data Analysis
Data was analysed to identify prominent types of NAI, the causes, place of occurrence, and time of presentation of the child to hospital after injury infliction. The data was cleaned in Excel and analysed in STATA, and the tables were exported to Microsoft Excel 2010 for analysis.
V.
36. Statistical Analyses
Average values and percentages were calculated for the different categories, and cross tabulations were used to compare the variables. The variables were tested for relationship significance using the Pearson Chi2 and Fischer's test. A P-Value less than 0.05 implies the variable is significant. The two are the same except that the Fischer's test applies when there are small cells (bivariate/cross tables with less than 5 in the cells). They all test for independence between two variables, with the null hypothesis stating that there is no association between the two variables, or that they are independent. Cramer V was used to test for strength of association. Cramer values range from 0 to 1, with a strong association if the value is close to 1 and a weak association if close to 0.
37. VI.
38. Results
Of the sample of 522 taken, it was noted that in 2008 there were a total of 174 (76 males) NAI cases, 170 in 2009 (120 males) and 178 in 2010 (126 males).
Overall, females accounted for 61.69% and males for 38.31%.
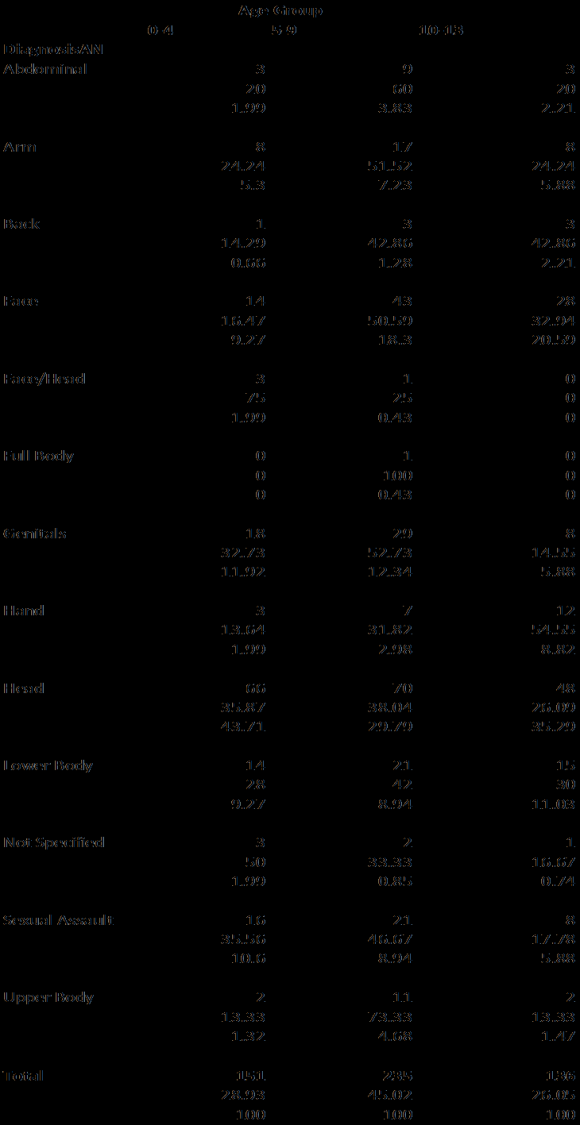
It was noted that the injuries inflicted on children occurred in several parts of the body. These were noted on the admissions forms as a primary diagnosis. Table 1 depicts the pattern of NAI. Head injuries were the most prevalent injury type, present in 35.4% of cases at the trauma centre. Head injuries included head lacerations, bruises and soft tissue damage. The most commonly documented injury (85.3 %) was bruising to the head followed by facial injuries (16.3%) and genital injuries (10.5%). In cases such as genitals being stated as a primary diagnosis, the cause was either genital assault or sexual abuse. This is clearly defined in the causes.
During primary diagnosis, it was noted that of the head injuries, 67.4% were male and32.6% female. Of the sexual assaults, 95.6% of cases were female and4.4% male. Of the genital injury cases, 56.36% were female and 43.64% male. Facial injuries were recorded in 75% of males and 25%of female cases.
In the 0 -4 age group, head injuries were more prevalent at 43.7%, followed by genitals (11.92%), sexual assault (10.6%), facial (9.27%), arms and hands (7.1%), and lower body (9.7%). For the 5 -9 year olds, the top cases were head injuries (29.8%), facial injuries (18.3%), genitals (12.3%) and sexual assault (8.94%).High numbers of head injuries were also recordedamong10 -13 year olds; at 35.3%, followed by facial injuries (20.6%), lower body (11%), sexual assault and genitals (5.9% respectively). Refer to Appendix A for more information. Because of the broad categories of primary diagnosis, we decided to use cause for most of the comparisons (cross tabulations), which had fewer categories and was likely to present the data well in addition to making it plausible for significance testing. Causes were divided into the following categories: physical assault, dog bites, genital assault, sexual abuse, neglect and not specified.
39. a) Differences in presentation between males and females
Table 2 shows that of the female cases, 60.5% were physical assaults, followed by 35% sexual abuse, 2% each for genital assault and not specified respectively, and 0.5% for dog bites. However, among the causes of NAI in males, 89.8% were for physical assault, followed by 5.3% for genital assault, while sexual abuse cases were very minimal at 1.6% compared with35% for females. Of all the causes, males surpassed females in occurrence, except for sexual abuse where 93.3% were female and 6.7% male. Fisher's test and P-value (Pr =0.00) suggests there is a high likelihood that cause and gender are associated. Cramer's V test of 0.5 suggests good strength in association between the two variables. Table 2 gives an outline of gender versus cause. The highest number of NAI cases was recorded among the 5 -9 age group, with 235 children (45.0%), followed by the 0 -4 age group with 28.9%, and finally the 10 -13 group with 26.1%. In terms of the causes of the injuries, sexual abuse cases were prevalent in the 5-9 group (48% recorded), the 0 -4 year old group (37.33%) and the 10 -13 group with 14.67%. The Fisher's test of 0.31 implies no association between cause and age, showing insignificance. Table 3 gives an outline of the results of age versus cause. Most of the physical assault cases occurred at home (49.14%) followed by school/crèche (26%), public spaces (15.6%) and unknown/other places (8.89%). Sexual assault was also most prevalent at home (61.33%), followed by other/unknown (26.67%), public space (6.67%), and (5.33%) at school. For more information see Appendix A.
40. d) Modes of transport for NIA cases
In essence, approximately 31% of the total NAI cases were transported by ambulance, while the police and schools each transported 1% respectively and 67% of cases were privately transported. The highest number of ambulance transportation cases were linked to physical assault (90.2 %), followed by sexual abuse cases at 7.8%, genital assault cases at 1.3% and0.7% for causes not specified. With the null hypothesis of no association between mode of transport and cause, the Fischer's test of 0.001 suggests we should reject the null hypothesis and assume association between the two variables. Cramer's V value of 0.1579 suggests a weak association between the cause and transport variables. Refer to Appendix A for more information.
41. e) Severity of NAI cases
With regard to the children present at the emergency rooms, severity was coded according to the categories Mild, Moderate, and Severe. The trauma unit classified patients based on the South African Triage score, and the clinical findings of the patient. In some instances it was not specified (6.32%). Moderate cases accounted for 71.3%, mild for 21.07% and the least common were severe cases, at 1.34%. The Fischer's test of 0.02 suggests an association between cause and severity coding. Table 4 gives an outline of cause versus severity. f) Decisions taken and management of cases Of all the NIA cases, a decision to admit was made in 28.74% of the total cases, 60.3% of cases were discharged, and 0.96% of cases were sent to a place of safety while for 9.96% of the cases, the decision was not specified. One can only assume they may have been discharged. With the null hypothesis of no association between decision and severity, the Fisher's test of 0.00 suggests we should reject the null hypothesis and assume significant association between the two variables. Cramer's V test notes the association to be of 21.4% strength. It would make sense that the severe cases were admitted into hospital. Of the moderate cases (71.26% of total cases), 34.68% were admitted, 55.38% discharged, 0.54% sent to a place of safety whilst 9.40% of the moderate cases' decision was not specified. For more information see Appendix A.
It is mandatory for the physician to report cases suspected to be NAI. Of major concern was the data provided by the social worker with respect to cases that were to be referred to the police and to be followed up by the social worker for the first and second time after the child was placed in a place of safety. It appeared not to tally with the decision taken as represented above. There was a huge gap in data recording in the management of the children sent to places of safety and those cases referred to the police. Following assessment regarding NAI, investigations ordered included blood work, X-rays, CT Scans, dressings and sutures. Due to poor recordkeeping, the majority of the cases (53.45%) were not specified in the type of investigation. For the recorded cases, the highest was 28.35% for X-rays, which correlates with the high number of physical assaults recorded. A combination of bloods, CT scans and Xrays accounted for 2.68%, the lowest being 0.77% for dressings/sutures. It is most likely that the 279 unspecified cases were given dressings and sutures since physical assault was the highest cause of NAI. Table 5 below gives an outline of the investigations ordered.
( D D D D ) H g) Perpetrators of NAI casesTable 6 shows the relationship between cause and perpetrator. Most of the perpetrators were not known, accounting for 65.52% of total NAI cases. Other children accounted for 20.11%, parents for 6.7%, known/family friend for 4.02% and relatives for 3.6%. Of the sexual abuse cases, 72% of perpetrators were unknown, 8% were family friends, 2.67% were committed by parents, 2.66% were committed by relative/siblings, and 14.67 were other children. With the null hypothesis of no association between cause and perpetrator, the Fisher test of 0.220 suggests we cannot reject the null hypothesis and assume no association between the two variables. Cramer's V test notes the association to be of 0.1224, which is a very weak strength of association.
42. Discussion
The abuse of children is a universal problem. [7] It affects children from all social classes, racial and religious groups. The Red Cross Hospital Trauma unit is the primary referral centre for injured children in the province and we expect that this may not be representative of other health care facilities, such as community clinics or private hospitals. Due to a lack of detailed information, we were not able to ascertain the deeper clinical conditions as did van As et al in the fractures study at the Red Cross Hospital. [8] Serious head injury in children younger than 2 years old is often the result of child abuse. [9] Though most studies note that intracranial trauma caused by shaking is the most frequent cause of death, [10] our study noted that head injuries in the 0-4 group were more prevalent, followed by genital and sexual assaults and injuries to the hands and arms. Though it is unclear whether the head injuries were associated with shaking or direct trauma, 85.3% were soft tissue injuries resulting International studies show that non-accidental head injuries among infants represent one of the most severe forms of child abuse, mortality rates of between 13% and 30% and significant neurological impairments in at least a half of the survivors. [11] Other studies show that inflicted head injuries are the leading cause of death of children who have been abused-there is an estimated prevalence of 1 per 3,000 in babies of less than six months. [12] The limitation of this study is that outcomes, morbidity and mortality for these cases were not included. A follow-up would help to determining what happened to those children, to allow for a comparison with the 50 000 deaths supposedly caused by NAI worldwide on an annual basis. [13] Incidence studies of non-accidental head injuries in the UK suggested figures ranging from roughly 10 -14 per 100,000 infants per year, [14] and it is estimated that approximately 12 children per 100,000 under the age of two years suffer from non-accidental subdural haemorrhage, with at least half of these injuries being related to shaking. [15] Children under the age of 4 years have considerable morbidity from head trauma, as this age group has a prevalence of traumatic brain injury (TBI) that is more than twice the rate of the general population and nearly twice the rate of older children. [20] In our study, the 5-9 age group had approximately 2% more head injuries that the 0-4group (36%), while the 10-13 group accounted for 26%. We cannot firmly assert that these resulted in subdural haemorrhage, though to a certain degree we can attribute child abuse.
Although the established consensus on fracture patterns in NAI is that long bone fractures are the most frequently experienced in clinical practice, the van As study [8] noted that nearly 40% of all fractures were skull fractures. Approximately one-third were inflicted with a weapon. Our study reveals that a high number of cases were the result of physical abuse with use of a weapon that in turn caused head injuries. Of the remaining hand, abdominal and leg injuries, the likelihood of these suspected to be fractures is high, given the request for X-rays in 148 cases. Alternative conditions must be considered before making a final diagnosis of NAI, e.g. osteogenesis imperfect a also presents with skeletal injuries. [26] Radiology is used to detect the type of injury inflicted, as well as to establish whether injuries are likely to be caused by NAI. [16][17][18] The radiologist involved must be familiar with the imaging, clinical, surgical, pathological, biomechanical, and forensic literature. [16] Our study was limited and did not focus on NAI being revealed by radiological evidence. It only went as far as noting whether the child was sent for Xrays, but not the results.
There is always some doubt concerning the authenticity of reported perpetrators due to fear by the child or caregiver. Child abuse is a sensitive issue with potential criminal implications; consequently, identification of the perpetrator or cause of injury is made harder and may influence the conclusions drawn from available data. Madu and Peltzer's study in the Northern Province of South Africa reported that many victims did not identify the perpetrator and where they did, the culprit was usually a 'friend'. [19] Our study noted that of the sexual abuse cases, 72% of the perpetrators were unknown, 8% were family friends, 2.67% were committed by parents, 2.66% were committed by relative/siblings, and 14.67 were other children. There is a huge possibility that the unknown cases are perpetrators known to the victims, but who the victims decided not to name due to fear, and other negative consequences.
Prevalence studies have revealed the widespread and hidden nature of child maltreatment. Maltreatment includes physical abuse and neglect. It occurs in all countries and cultures and results from the interaction between several risk factors; such as parental depression, stress, and social isolation. [19] Our study does not identify the risk factors that resulted in child maltreatment, only describing cases where it has already been inflicted. The trauma and ward registers make no provision to note the socioeconomic status/income bands of parents or caregivers, there by renderingan examination of the potential link to NAI difficult.
Sexual abuse is one of the most prominent forms of NAI and is mostly common in females. [20] Our results show the same picture, noting that of the sexual abuse cases, 93.3% were female and 6.7% male. In cases of physical abuse, specific attention should be paid to the genital areas to exclude possible associated sexual abuse. [21] Our study concurs, noting that the primary diagnosis of genital assault and sexual assault was mostly caused by sexual abuse.
Unfortunately, not all cases are reported and many of them go unnoticed. [22] A variety of individuals may identify NAI; such as, for example, social workers, health visitors, neighbours, teachers, family practitioners and many other people working with children. [23---24] Though our study identifies places of occurrence as schools, home, public spaces and unknown, it does not explicitly identify who reports or detects NAI. We can only deduce from the places of occurrence, such as schools, that teachers tend to notice and take further action, such as calling an ambulance or using private transport to seek medical attention for the child. This is required by the South African's Children's Act, chapter 7, section 110, which makes it mandatory for any professional dealing with children to report suspected cases of NAI. [25] VIII.
43. Conclusion
It is clear from the above analysis that Nonaccidental Injury (NAI) cases are not clear cut and need proper investigation and management for immediate clinical treatment and successful prosecution of perpetrators. The results of this study helped to describe common injury patterns in different age groups and genders. Hopefully, this will increase awareness of the NAI among healthcare practitioners and identify areas for advocacy.
44. IX.
45. ( D D D D ) H
I would like to thank God for giving me the strength and knowledge to write this article. I also appreciate the input and effort of my supervisors. Thanks to their constant guidance I was able to write this article.
46. Ethical Approval
Ethical approval for the study was obtained from the relevant ethics committee at the University of Cape Town. Appendix C contains the ethics approval letter. Style: Abbreviations and symbols must be standard and SI units used throughout except for blood pressure values which are reported in mm Hg. Acronyms should be used sparingly and fully explained when first used.
47. Volume XIV Issue IV Version I
Figures/illustrations: Black and white images should be saved and supplied as GIF, TIFF, EPS or JPEG files, at a minimum resolution of 300 dpi and an image size of 9 cm across for single column format and 18.5 cm for double column format. Colour images should be saved and supplied as GIF, TIFF, EPS or JPEG files, to a minimum resolution of 600 dpi at an image size of 9 cm across for single column format and 18.5 cm for double column format. Images should be mentioned in the text and figure legends should be listed at the end of the manuscript. During submission, when you upload the figure files please label them as Figure 1, Figure 2, etc.
The file label will not appear in the pdf but the order in which the figures uploaded should be sufficient to link them to the correct figure legend for identification. Histograms should be presented in a simple, twodimensional format, with no background grid.
Tables: Tables should be submitted in the same format as your article and embedded into the document where the table should be cited. Tables should be selfexplanatory and the data they contain must not be duplicated in the text or figures.
References: Authors are responsible for the accuracy of references cited: these should be checked against the original documents before the paper is submitted. It is vital that the references are styled correctly so that they may be hyperlinked.
In the text: References must be numbered sequentially as they appear in the text. References cited in figures or tables (or in their legends and footnotes) should be numbered according to the place in the text where that table or figure is first cited.
Reference numbers in the text must be given in square brackets immediately after punctuation (with no word spacing) -for example, [6] not [6]. Where more than one reference is cited, separate by a comma, for example, [1,4,39] For sequences of consecutive numbers, give the first and last number of the sequence separated by a hyphen ---for example, [22][23][24][25].
References provided in this format are translated during the production process to superscript type, which act as hyperlinks from the text to the quoted references in electronic forms of the article. In the reference list: References must be double spaced (numbered consecutively in the order in which they are mentioned in the text) in the [slightly modified] Vancouver style.
If there is uncertainty about acceptance after review, papers are reviewed by the editors.
All material submitted is assumed to be submitted exclusively to the journal unless the contrary is stated. Submissions may be returned to the author for amendment if presented in the incorrect format. The title page must contain the following information: 1. The title.
48. Original articles
For full length accounts of original research, often shorter articles are better. Additional information may be placed on the web site as a data supplement. Word count: up to 3000 words. Illustrations and tables: up to 6. References: 25. Peer review: all papers are reviewed by at least one reviewer.
Appendix C : Emergency Medicine Journal Instruction to Authors Only papers published or in press should be included in the reference list. (Personal communications or unpublished data must be cited in parentheses in the text with the name(s) of the source(s) and the year.


| Year 2014 | ||
| Volume XIV Issue IV Version I | ||
| D D D D ) H | ||
| ( | ||
| Primary Diagnosis | Frequency | Per cent |
| Abdominal | 15 | 2.9 |
| Arm | 33 | 6.3 |
| Back | 7 | 1.3 |
| Face | 85 | 16.3 |
| Face/Head | 4 | 0.8 |
| Full Body | 1 | 0.2 |
| Genitals | 55 | 10.5 |
| Hand | 22 | 4.2 |
| Head | 184 | 35.3 |
| Lower Body | 50 | 9.6 |
| Not Specified | 6 | 1.2 |
| Sexual Assault | 45 | 8.6 |
| Upper Body | 15 | 2.9 |
| Total | 522 | 100 |
| Gender | |||
| Cause | Female | Male | Total |
| Physical Assault | 121 | 289 | 410 |
| Row per cent | 29.5 | 70.5 | 100 |
| Column per cent | 60.5 | 89.8 | 78.5 |
| Dog Bite | 1 | 3 | 4 |
| Row per cent | 25 | 75 | 100 |
| Column per cent | 0.5 | 0.9 | 0.8 |
| Genital Assault | 4 | 17 | 21 |
| Row per cent | 19.1 | 81.0 | 100 |
| Column per cent | 2 | 5.3 | 4.02 |
| Neglect | 0 | 1 | 1 |
| Row per cent | 0 | 100 | 100 |
| Column per cent | 0 | 0.3 | 0.2 |
| Not Specified | 4 | 7 | 11 |
| Row per cent | 36.4 | 63.6 | 100 |
| Column per cent | 2 | 2.2 | 2.1 |
| Sexual Abuse | 70 | 5 | 75 |
| Row per cent | 93.3 | 6.7 | 100 |
| Column per cent | 35 | 1.6 | 14.4 |
| Total | 200 | 322 | 522 |
| Row per cent | 38.3 | 61.7 | 100 |
| Column per cent | 100 | 100 | 100 |
| b) Injury types according to age group | |||
| Year 2014 | ||||
| Volume XIV Issue IV Version I | ||||
| D D D D ) H | ||||
| ( | ||||
| Age Category (years) | ||||
| Cause | 0-4 | 5-9 | 10-13 | Total |
| Physical Assault | 111 | 182 | 117 | 410 |
| Row per cent | 27.07 | 44.39 | 28.54 | 100 |
| Column per cent | 73.51 | 77.45 | 86.03 | 78.54 |
| Dog Bite | 1 | 2 | 1 | 4 |
| © 2014 Global Journals Inc. (US) | ||||
| Severity |
| Year 2014 | ||
| Volume XIV Issue IV Version I | ||
| Investigations | Frequency | Per cent |
| Bloods | 12 | 2.3 |
| CT Scan | 65 | 12.45 |
| X-ray | 148 | 28.35 |
| Scan/X-Ray-combination | 14 | 2.68 |
| Dressings/Sutures | 4 | 0.77 |
| Not Specified | 279 | 53.45 |
| Total | 522 | 100 |
| Gender versus Primary Diagnosis Age versus Primary diagnosis Place of occurrence versus Cause Transportation of NIA cases versus Cause Decision taken versus Severity of NIA cases | |||||||||||||||||
| Severity | |||||||||||||||||
| Mild | Gender Moderate | Transport Not Specified | Severe | Total | |||||||||||||
| Decision Diagnosis Abdominal Cause Admit Cause Physical Assault Physical Assault | Female Creche/School Ambulance 6 2 40 3 107 \ \ \ \ \ \ \ 26.42 138 1.33 35.29 1.82 | Home Police 129 199 49.14 3 86 0.77 34.68 | Male Other/Unknown Public Place Total Private School 9 12 7 15 60 100 2.8 2.87 36 63 8.89 15.56 246 4 8 4.67 62.92 1.02 36.36 100 28.74 150 100 | Total Total 405 100 391 100 | |||||||||||||
| Discharge | 90.2 | 89.92 94 | 76.25 42.86 206 | 15 | 59.02 74.1 | 0 | 85.14 8 | 315 | 78.64 78.67 | ||||||||
| Arm | 13 29.84 | 65.4 | 20 4.76 | 0 | 33 | 100 | |||||||||||
| Year 2014 | Back Face Dog Bite Dog Bite Genital Assault Genital Assault Not Specified Place of Safety | 0 0 0 2 10.53 1.31 | 39.39 6.5 2 28.57 1 19 22.35 0 85.45 0 0 7 33.33 5.88 2.73 60 11 21.15 10 3 | 0 55.38 0 0.54 0 0 0 0 40 35 67.31 9.41 2 | 3 75 1.15 7 33.33 2.68 | 60.61 6.21 5 71.43 1.55 66 77.65 45.45 0 0 6 11.54 18.18 0 | 0 0 0 2 9.52 100 4 3.28 1.2 17 89.47 5.12 | 0 0 0 0 0 0 0 | 100 6.32 7 100 1.34 85 100 1 60.34 25 0 0 1.35 5 23.81 6.76 0.96 0 0 0 0 100 52 100 9.96 5 | 4 4 100 100 0.78 21 100 4.08 0.8 19 100 3.82 | Year 2014 Year 2014 Year 2014 Year 2014 | ||||||
| ( D D D D ) H ( D D D D ) H ( D D D D ) H | 2. | 9.5 1 25 0.5 0 0 0 31 56.36 15.5 6 27.27 3 60 32.61 30 13 26 6.5 3 66.5 ASE=0.069 38.89 ASE=0.034 133 0.001 Face/Head Full Body Genitals Hand Head Lower Body Not Specified gamma=0.2237 Kendall's tau-b Fisher's exact = Not Known Cramér's V=1.813 Kendall's tau-b = 0.1511 ASE = 0.037 4.5 likelihood-ratio chi2(15)=51. Pr=0.001 Cramér's V = 0.1579 42.86 Pearson chi2(15)= 50.782 Pr=0.000 Known/Family Friend 9 likelihood-ratio chi2(15) = 32.9357 Pr = 0.05 Neglect 0 0 0 Not Specified 1 11.11 0.84 Sexual Abuse 4 5.33 3.36 Total 119 23.11 100 100 gamma = -0.3980 ASE = 0.102 15 Pearson chi2(15) = 36.8697 Pr = 0.001 28.57 Another Child 30 Total 153 30.78 Female Perpetrator Neglect 0 0 0 Not Specified 1 10 0.65 Sexual Abuse 12 16.67 7.84 Total 110 21.07 100 Pearson chi2(9) = 71.5119 Pr = 0.000 likelihood-ratio chi2(9) = 89.3390 Pr = 0.000 Cramér's V = 0.2137 gamma = -0.4837 ASE = 0.067 Kendall's tau-b = -0.2392 ASE = 0.035 Fisher's exact = 0.000 Gender versus Perpetrator 20.5 3 75 0.93 1 100 0.31 24 43.64 7.45 16 72.73 4.97 124 67.39 38.51 37 74 11.49 3 64.91 61.11 209 3.73 57.14 12 0 1 0 100 0 1.64 6 2 66.67 22.22 2.3 3.28 46 20 61.33 26.67 17.62 32.79 261 61 50.68 11.84 100 100 100 100 23.29 71.43 75 7 332 1.41 66.8 Male 0 1 0 100 0 0.3 0 8 0 80 0 2.41 4 56 5.56 77.78 57.14 16.87 372 33 71.26 6.32 100 100 Gender | 7 1.34 100 | 16.28 4 100 0.77 1 100 0.19 55 100 10.54 22 100 4.21 184 35.25 50 100 9.58 6 65.52 100 342 4.02 100 21 100 0 0 0 0 0 0 5 6.67 6.76 74 14.37 100 100 20.11 100 105 5 1.01 Total 0 0 0 1 10 20 0 0 0 522 100 100 | 1 100 0.19 9 100 1.75 75 100 100 100 100 515 497 100 14.56 1 100 0.2 10 100 2.01 72 100 14.49 | Volume XIV Issue IV Version I ( D D D D ) H ( ( ( D D D D ) H D D D D ) H D D D H D ) Volume XIV Issue IV Version I Volume XIV Issue IV Version I Volume XIV Issue IV Version I | |||||||||||
| Parent | 50 1.5 | 17 48.57 | 50 0.93 51.43 18 | 100 35 1.15 100 | |||||||||||||
| 8.5 | 5.59 | 6.7 | |||||||||||||||
| Sexual Assault | 43 | 2 | 45 | ||||||||||||||
| Relative/Sibling | 95.56 | 11 | 4.44 | 8 | 100 19 | ||||||||||||
| 21.5 57.89 | 0.62 42.11 | 8.62 100 | |||||||||||||||
| 5.5 | 2.48 | 3.64 | |||||||||||||||
| Upper Body | 3 | 12 | 15 | ||||||||||||||
| Total | 20 | 200 | 80 | 322 | 100 522 | ||||||||||||
| 1.5 | 38.31 | 3.73 61.69 | 2.87 100 | ||||||||||||||
| 100 | 100 | 100 | |||||||||||||||
| Total Pearson chi2(4) = 9.0885 Pr = 0.059 200 | 322 | 522 | |||||||||||||||
| 38.31 likelihood-ratio chi2(4) = 9.1105 Pr = 0.058 | 61.69 | 100 | |||||||||||||||
| Cramér's V = 0.1320 | 100 | 100 | 100 | ||||||||||||||
| gamma = -0.2249 ASE = 0.081 | |||||||||||||||||
| Kendall's tau-b = -0.1124 ASE = 0.041 | |||||||||||||||||
| Fisher's exact = | 0.055 | ||||||||||||||||
| © 2014 Global Journals Inc. (US) | |||||||||||||||||