1.
Wernicke's Encephalopathy Associated with Hyperemesis Gravidarum: A Case Report Soraya Saleh Gargari ? , Maasoumeh Saleh ? , Fereshteh Bagherifard ? & Maasoumeh Alizadeh ? Abstract-We report the case of a 30 year-old woman, at 16 weeks of gestational age, with hyperemesis gravidarum. She presented with blurred vision and ophthalmoplagia, VI nerve palsy, distraction and gazing were detected in physical examination. The resonance magnetic imaging was repoeted normal. Her pregnancy was terminated with suspected preeclampsia, but she had gradually decline in GCS and heparin was started with suspected sinus venosus thrombosis.
Unfortunately, she died and then in review of brain imaging in the mortality conference, she had typical changes of Wernicke's encephalopathy. WE is a potentially reversible condition if treated early. We would like to emphasize the importance of prompt thiamine supplementation in pregnant women with prolonged vomiting in pregnancy, especially before starting intravenous or parentral nutrition. Early thiamine replacement will reduce maternal morbidity and fetal loss rate. It was a missed management WE in another center, so we have decided to report it to think of this diagnosis in cases of hyperemesis garavidarum with neurologic symptoms. This report is according to documents.
Keywords: hyperemesis gravidarum, wernicke encephalopathy, thiamin.
2. I. Introduction
G is characterised by severe, protracted nausea and vomiting associated with weight loss of more than 5% of pre-pregnancy weight, dehydration and electrolyte imbalances (1). Wernicke's encephalopathy (WE) and Korsakoffs psychosis are severe manifestations of thiamine deficiency. WE is commonly associated with alcoholism, probably because chronic alcohol ingestion results in increased thiamin utilization, reduced GI uptake and impaired phosphorylation of thiamin. WE has also been reported in an increasing array of conditions that affect nutrition, however, including prolonged intravenous feeding, gastrointestinal procedures and diseases, malignancies, infections, starvation and hyperemesis gravidarum. WE has classic triad of oculo-motor abnormalities, cerebellar dysfunction, and altered mental state, which might manifest as disorientation, confusion or even coma. The majority of patients with WE do not have all three triad signs, only 10% of patients exhibit all three features (2). Untreated WE is fatal. Mortality rate is 10% to 20% among treated patients (3). In patients suspected of WE, thiamine treatment should be started immediately (4). Blood should be immediately taken to test for thiamine, other vitamins and minerals levels. Following this an immediate intravenous or intramuscular dose of thiamine (50-100 mg) should be administered (5) two or three times daily. Thiamine administration is usually continued until clinical improvement ceases. Concomitant liver failure, infection or delirium tremens often makes the cause of death unclear (6).
If glucose is given, such as in hypoglycaemic alcoholics, thiamine must be given concurrently. If this is not done, the glucose will rapidly consume the remaining thiamine reserves, exacerbating this condition (4).
Other nutritional abnormalities should also be looked for, as they may be exacerbating the disease (7,8). In particular, magnesium, a cofactor of transketolase which may induce or aggravate the disease (4).
3. II. Case Presentation
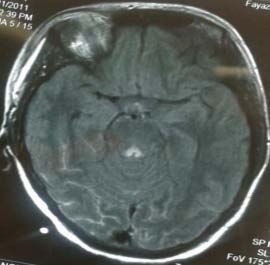
A 30 years old woman, gravidity 2, parity 1, with history of a vaginal delivery 13 years ago, with gestational age of 16 weeks, admitted in another center with chief complaint of blurred vision. She had gestational diabetes on diet and obsessive compulsive disorders (OCD) who discontinued her medications in early pregnancy. She had 20kg weight loss during pregnancy due to anorexia and vomiting and had two admissions in gestational age of 10 weeks and 12 weeks with diagnosis of hyperemesis gravidarum. In this admission, physical examination showed: Blood pressure fluctuation from 120 to 160 mmHg systolic and from 80 to 100 mmHg diastolic, Pulse rate: 120 beats per minute, Temprature: 370C. Also she had ophthalmoplagia, VI nerve palsy, distraction and gazing. In lab tests, elevated liver enzymes, elevated ESR, hypokalemia, proteinuria (1+) and ketonuria (1+) was detected. Methylprednisolon was started for the patient by internist due to increased ESR and elevated liver enzymes and CNS symptoms. Blood pressure was controlled with atenolol and Mg-SO4 started with diagnosis of preeclampsia. Brain MRI and MRV requested by neurologist due to CNS symptoms and suspected sinus venosus thrombosis, and were reported normal by radiologist. In examination by ophthalmologist, no abnormal findings were detected. Lumbar punctuation was done and her intracranial pressure was normal. With diagnosis of preeclampsia, pregnancy was terminated 10 days after admission with vaginal misoprostol. After pregnancy termination, her CNS symptoms were continued, so ANA and antiphoshpholipid antibodies were requested by neurologist that were normal. One day after pregnancy termination, she had gradually decline in GCS. During 24 hours, GCS decline to 3/15 and with suspected sinus venosus thrombosis, heparin was started for her, but unfortunately she died 18 days after termination. In mortality conference, the management of case was evaluated respectively and her brain imaging was reviewed. Brain MRI had typical changes of WE (image 1). This patient was a missed diagnosis WE.
Image 1: On the T2 and FLAIR images, increased signal intensity is present at periaqueductal gray matter and both mammillary bodies, highly suggestive of WE. Periaqueductal gray matter involvement is suggestive of two diagnoses: 1. Leigh disease, 2. WE. For differentiation between them: involvement of mammillary bodies is infavor of WE and is against diagnosis of Leigh disease.
4. III. Discussion
WE is a potentially reversible yet serious neurological manifestation caused by vitamin B1 (thiamine) deficiency (9). If the cells with high metabolic requirements have inadequate stores of thiamine, energy production drops, and neuronal damage ensues (10). Time to deplet the body's store of thiamine is about 3 weeks (11). The daily requirement of thiamine is around 1.1 mg/day for females, and it increases to 1.5 mg/day, particularly during pregnancy and lactation (12).The prevalence of WE in a non-alcoholic patient varies from 0.04% to 0.13% (13). Many cases of WE in pregnancy with hyperemesis gravidarum (HG), were first reported in 1914 (14). Most patients present with the triad of ocular signs, ataxia and confusion (9). MRI is the imaging modality of choice because it is highly specific (93%) and comparatively safer than computed tomography (CT) scan (9). On imaging, it is commonly seen on MRI as areas of symmetrical increased T2/FLAIR signal involving the mammillary bodies, dorsomedial thalami, tecatl plate, periaqueductal area, and around the third ventricle. Lab assessment of blood transketolase activity and thiamine pyrophosphate (TPP) are not very reliable (9). Almost 80% cases remain undiagnosed, as the majority are diagnosed on autopsy (15). Guidelines by the European Federation of Neurological Societies (EFNS) recommend that thiamine should be given 200 mg thrice daily via intravenous route, started before any carbohydrate, and continued until there is no further improvement in signs and symptoms (16). WE is precipitated by administration of glucose-containing fluids before thiamine supplementation (9). If the condition is not recognized and treated early, patients can have permanent brain injury, manifested by impairment of recent and remote memory, apathy, and confabulation, along with persistent manifestations of WE, including ataxia and varying degrees of ohthalmoparesis. The main factors triggering death are thought to be infections and liver dysfunctions (6). After acute recovery, patients should undergo detailed neurocognitive evaluation to document residual deficits. Cognitive deficits are the last to recover and they may not recover completely. Patients should be followed periodically to ensure they do not relapse and continue to be adherent to dietary supplementation with a multivitamin and thiamine. Our case shows highly clinical suspicion is needed for diagnosis of WE in cases of hyperemesis gravidarum and early treatment is essential for prevention of complications and death.
5. IV. Conclusion
Patients at high risk for developing thiamine deficiency may benefit from supplementary thiamine intake either parenterally or orally depending on clinical circumstances. All patients suspected of having WE after stabilization of their cardiovascular and respiratory systems should be treated with parenteral thiamine to avoid permanent brain injury, including the development later of Korsakoff's psychosis and death. Year