1. I. Introduction
ausea and vomiting are universal symptoms encountered in daily clinical practice, mostly as a part of medical illnesses involving the gastrointestinal tract with causes ranging from relatively benign to at times serious pathology. In either case, these symptoms are very distressing to patients. Therefore, a systematic approach is warranted to determine the cause particularly in cases of intractable nausea and vomiting. We report a 76-years-old female with intractable nausea and vomiting where diagnosis of systemic amyloidosis was made after an extensive workup. Being a systemic disease, amyloidosis affected multiple systems including extremely rarely involved organs.
A76 years old non-alcoholic female with history of coronary artery disease (CAD) developed intractable nausea and vomiting lasting two months with repeated admissions to various hospitals. An upper endoscopy (EGD) was done which showed duodenal ulcer and Helicobacter pylori was identified on biopsy. She was subsequently treated with triple therapy. At the same time, she was diagnosed with severe primary hypothyroidism and was started on levothyroxine supplementation. Despite completing triple therapy for Helicobacter pylori infection, she had persistent nausea and vomiting, and presented to our hospital. Furthermore, she had developed generalized body swelling and a skin rash.
On examination, she was noted to have bilateral feet and leg swelling, epigastric tenderness and a faint maculopapular rash was evident on the abdomen. Laboratory investigations were noteworthy of the following: BUN 26 mg/dl, Cr. 1.30 mg/dl, Na 129 mEq/l, K 5.2 mEq/l, HCO 3 16 mEq/l, AST 169 U/l, ALT 86 U/l, ALP 2390 U/l, total bilirubin 0.6 mg/dl, albumin 1.2 gm/dl and ?-glutamyl transpeptidase (GGTP) 849 U/l. Hemogram showed a WBC count of 10.2 x 10 3 per µl, hemoglobin level of 18.7 gm/dl and platelet count of 238 x 10 3 per µl. Thyroid function tests showed elevated TSH at 51 IU/ml (which was markedly elevated at > 200 per µIU/ml on previous admission to another hospital), decreased free T4 at 0.59 ng/dl and decreased free T3 at 1.13 pg/dl. Her troponin level was also found to be elevated at 0.47 ng/ml.
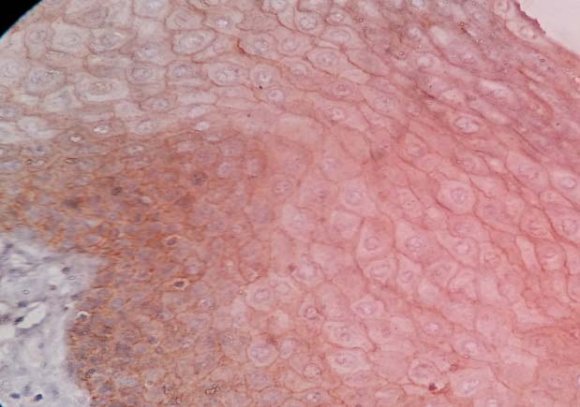
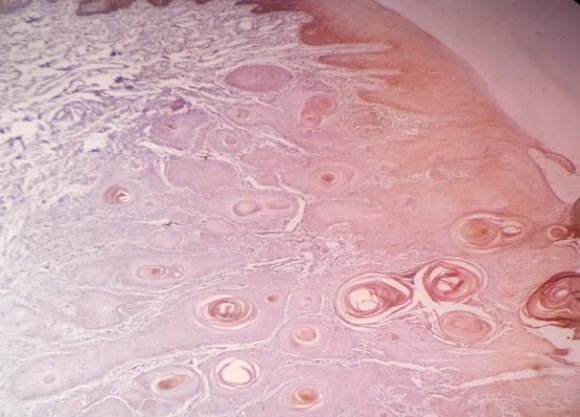
Renal function abnormalities were presumed to be secondary to pre-renal etiology from dehydration consequent to vomiting. Electrolyte derangements were corrected and therapy was instituted for severe hypothyroidism as intravenous levothyroxine. Deranged hepatic enzymes were evaluated for hepatobiliary pathology with a computerized tomography (CT) scan of the abdomen which showed bilateral pleural effusions and findings compatible with hepatic cirrhosis and ascites (Figure 1). Further evaluation of hepatic cirrhosis was negative for infectious or autoimmune causes. The elevation in liver and biliary tract enzymes in particular markedly elevated alkaline phosphatase was presumed to be due to severe hypothyroidism. During the course of her treatment, she developed worsening anasarca and severe hypoalbuminemia raising suspicion of nephrotic syndrome. Therefore, a 24 hour urinary protein quantification demonstrated proteinuria of 4 grams. As part of nephrotic syndrome workup, she was noted to have IgA lambda monoclonal gammopathy on serum protein immunofixation, however, serum protein electrophoresis did not show any abnormal monocloncal spike. Serum immunoglobulin analysis revealed elevated immunoglobulin A level at 544 mg/dl and decreased IgG level at 442 mg/dl. Serum kappa free light chains were 30 mg/l, lambda free light chains were 148 mg/l and kappa/lambda ratio was decreased to < 0.2. Ultimately, a kidney biopsy was done to find out the exact cause of nephrotic syndrome which stained positive for Congo red and birefringence (Figure 4a & 4b). PAS, Jones and trichrome stain were compatible with amyloidosis. She was diagnosed with type AL systemic amyloidosis with gastric, cardiac, thyroid, liver and kidney involvement. The morbiliform skin rash was thought to be secondary to amoxicillin which she received as part of H. pylori treatment and it improved over the course of her hospital stay. She was given diuretics, albumin infusions and steroids. After stabilization in the hospitalization, she was discharged. Unfortunately, bone marrow biopsy could not be performed as patient was readmitted to another hospital and passed away.
2. III. Discussion
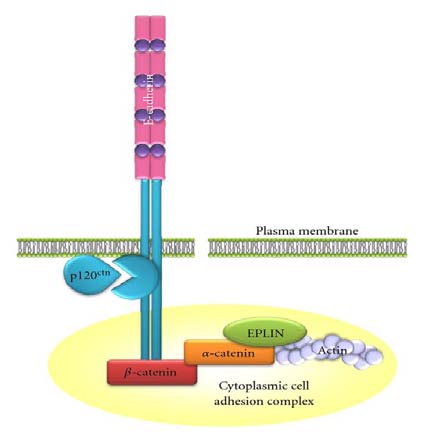
Amyloidosis is characterized by deposition of misfolded filbrillar proteins in the extracellular space, leading to multiple organ and tissue derangements [1]. The primary pathogenetic mechanism involves antiparallel beta-pleated sheet conformation of polypeptide molecules resulting in insoluble protein aggregates that get deposited in tissues as amyloid. This abnormal folding of native proteins occurs due to various factors including intrinsic amyloidogenic propensity, increased serum concentrations, aging, genetics and proteolytic remodeling [2]. Amyloidosis is classified according to the precursor protein. Primary or AL amyloidosis is caused by deposition of monoclonal immunoglobulin light chains and occurs in association with plasma cell dyscrasias. Secondary or AA amyloidosis is derived from serum amyloid A protein and occurs in association with chronic underlying inflammatory disorders. Several familial forms of amyloidosis have been identified such as transthyretin, apolipoprotein A-1 and fibrinogen A. Long term dialysis also results in amyloidosis derived from ?-2 microglobulin [1,3,4].
Gastrointestinal disease is present in as many as 60 percent of patients with amyloidosis which can occur as an isolated entity or as part of multiorgan involvement [5,6]. GI involvement is more common in AL type rather than AA type amyloidosis [7,8]. Gastrointestinal disease in amyloidosis results from either mucosal or neuromuscular infiltration. In addition, an extrinsic autonomic neuropathy may also affect gut function [5]. Infiltration may occur anywhere along the GI tract presenting as GI bleeding, malabsorption, protein losing enteropathy and chronic GI dysmotility. GI dysmotility presenting as nausea, vomiting and pseudo obstruction is a rare presentation that occurs in 1% of patients with GI amyloidosis [5,6,7,9]. There have been rare cases reported with systemic amyloidosis presenting solely as a gastrointestinal obstruction or pseudo obstruction [10,11,12,13]. Even though there were multiple systems involved in this patient, but amyloid gastropathy presenting as nausea and vomiting was most predominant.
Being a systemic disease, amyloid can infiltrate the thyroid gland. Thyroid infiltration can present as progressively enlarging goiter and can be confused with rapidly enlarging thyroid cancer. The majority of amyloidosis affected patients develop infiltration of the thyroid gland; yet thyroid dysfunction in the form of hypothyroidism rarely occurs [14]. Literature search reveals only a few case reports of severe hypothyroidism as manifestation of systemic amyloidosis and most of these cases were diagnosed at autopsy [15,16]. Severe hypothyroidism in this case was presumed to be due to amyloidosis involving thyroid gland. Interestingly, we did not see goiter in our patient which is a more common manifestation of thyroid infiltration.
Secondly, cardiac involvement occurs in up to 50 percent of patients with AL amyloidosis compared to less than 5 percent with AA amyloidosis [21,22]. The heart is considered involved if either an endomyocardial biopsy demonstrates amyloidosis in the presence of clinical or laboratory evidence of involvement or echocardiographic evidence of amyloidosis is found in a patient with a positive result of noncardiac biopsy [23]. Besides EKG which shows low voltage QRS complexes, echocardiography is particular useful in diagnosis especially if there are not significant cardiac symptoms [22]. In our patient, asymmetrical septal hypertrophy and lack of outflow tract obstruction favored an infiltrative disease. It is of great importance to pay particular attention to details such as low voltage QRS complexes, as it may be a clue towards a rare yet significant disease.
Thirdly, severe hypoalbuminemia and nephrotic range proteinuria were secondary to renal involvement of amyloidosis, which was confirmed by renal biopsy. The kidney is affected in 50% to 80% of patients with AL amyloidosis and is the most common cause of mortality in these patients along with cardiac manifestations [24]. Diagnosis is made by renal biopsy demonstrating Congo red staining and apple-green birefringence upon polarization [24,25]. Renal manifestations in amyloidosis are characterized by nephrotic syndrome with heavy proteinuria and impaired renal functions [26].
Our patient exhibited both nephrotic syndrome and impairment of renal functions.
The present case is very unique in presentation as there were two exceedingly rare manifestations of systemic amyloidosis: amyloid gastropathy and severe hypothyroidism. The diagnosis in the patient was confounded by recent diagnosis of H. pylori related duodenal ulcer. However, the symptoms persisted even after undergoing therapy leading to repeated admissions in various hospitals. Moreover, the diagnosis was challenging in the presence of another systemic disease, hypothyroidism. Although recurrent nausea and vomiting is relatively uncommon in hypothyroidism, its concomitant presence in this case complicated the diagnosis. After extensive investigations, the clue towards a systemic infiltrating disease (amyloidosis) was provided by EKG which showed low voltage complexes, underscoring the importance of even basic investigations. Ultimately, diagnosis of systemic amyloidosis was reached after renal biopsy.
Amyloidosis, being a great masquerader, is one of the unusual diseases that physicians encounter and often presents a diagnostic challenge as in our patient. Suspicion of GI involvement may be very low if other organs are unaffected. However, unexplained nausea and vomiting and lack of resolution of these symptoms should raise possibility of such rare yet significant disease as amyloidosis. It becomes more crucial to consider amyloidosis in the differential if there is multiorgan involvement. Lastly, early diagnosis is important to initiate timely therapy as the response to treatment could be very different, and ultimately affects patient morbidity and mortality.
Because amyloidosis is a systemic disease, we find involvement of multiple systems in our case besides GI tract and thyroid gland. Firstly, involvement of liver was noted when CT scan of the abdomen was done. Although hepatic involvement is very common in patients with amyloidosis, the clinical manifestations of hepatic involvement are usually mild [17,18]. Liver infiltration is more common in AL amyloidosis than AA amyloidosis [6]. Hepatomegaly is present in up to 81-92% of patients in amyloidosis [6,20]. Contrastenhanced CT scan, although not diagnostic, may show an enlarged liver with heterogeneous decreased attenuation or rarely a mass [18,19]. The patients are often misdiagnosed with hepatic cirrhosis based on imaging features. In this patient, cirrhosis was thought to be secondary to amyloidosis because all causes of hepatic cirrhosis (HBV, HCV, autoimmune, alcohol, hemochromatosis) were excluded. Elevated alkaline phosphatase, usually along with elevated GGTP, is the most common laboratory abnormality in systemic amyloidosis [17,20]. In our patient, markedly elevated alkaline phosphatase and CT scan findings strongly suggested amyloid infiltration of liver.