1. I. Introduction
lobally, HIV kills more than 8000 people daily while more than 5000 people die of tuberculosis (TB) every day. It is estimated that one-third of the world's population are infected with TB, and 40 million people currently living with HIV/AIDS [1]. In addition, without proper treatment, 90% of HIV-infected individuals could die within months of contracting TB. Four million people infected with HIV have also TB disease worldwide making TB the major killer in HIVinfected patients [1].
Tuberculosis is the leading cause of death for HIV-infected patient and HIV is the most important risk factor for developing active TB [2; 3]. The double epidemic of TB and HIV is great concern, especially in sub-Saharan Africa where 80% of the burden of coinfection resides and health systems are already weak and overstretched [4]. The risk of death from TB is significantly higher in the HIV-infected population even if the organism is sensitive to and responsive to anti-TB medications [5]. The convergence of the tuberculosis (TB) and the HIV epidemics has posed new public health challenges [6].
The interaction of HIV and TB in co-infected persons is bidirectional and synergistic: HIV-1 infection predisposes to the development of active TB and the course of HIV-related immunodeficiency is worsened by active TB infection [7].
The HIV/AIDS pandemic is a major challenge to the control of TB in Ethiopia. The dual epidemic has a number of impacts on the health sector because it increases TB and HIV burden, demands for more care and worsens the situation of the already overstretched health care delivery system in the country. HIV increases susceptibility to infection with M. tuberculosis, the risk of progression to TB disease, and the incidence and prevalence of TB. The life time risk of HIV positive individuals to develop TB is 20-37 times greater than HIV negative individuals. It also increases the likelihood of re-infections and relapses of TB. In a population where TB/HIV is common, health services struggle to cope with the large and rising number of TB [8].
G Year 2015 © 2015 Global Journals Inc. (US)Volume XV Issue V Version I ( ) F Furthermore, 22 high burden countries (HBCs) with TB accounted for approximately 80% of the estimated number of new all form of TB cases which rising worldwide on the same year. Ethiopia was ranked seventh among the world 22 high burden countries (HBCs). In Africa, those countries with high rates of TB-HIV co-infection are the main focus of intensified efforts in directly observed treatment short course (DOTS) expansion [9]. Ethiopia adopted the DOTS strategy since 1997 after success of the pilot program with the development of the first combined Tuberculosis and Leprosy Prevention and Control Program manual. TB-HIV collaborative activities was piloted in 2004 and afterward scaled up nationally. The STOP TB strategy was launched by World Health Organization (WHO) in 2006 to achieve the millennium development goals (MDGs) for TB in 2015. Ethiopia also adopted this strategy to achieve the national TB-leprosy and TB/HIV targets [8].
The main reason of this study was to assess the level of TB-HIV co-infection and factors associated with TB-HIV co-infection at Fenote Selam district hospital, Amhara, Northwest Ethiopia, 2014.
2. II. Methods and Materials
Study settings: The study was conducted at Fenote Selam district hospital, which is about 378 km from capital city of Ethiopia, Addis Ababa, and data collection, was conducted in May 2014.
Study design: retrospective cohort study was employed to identify the level of TB-HIV co-infection and factors associated with TB-HIV co-infection.
Study population: the population of the study was medical records of all TB and TB-HIV co-infection patients who were on anti tuberculosis treatment at TB clinic from March, 2009 to march, 2014.
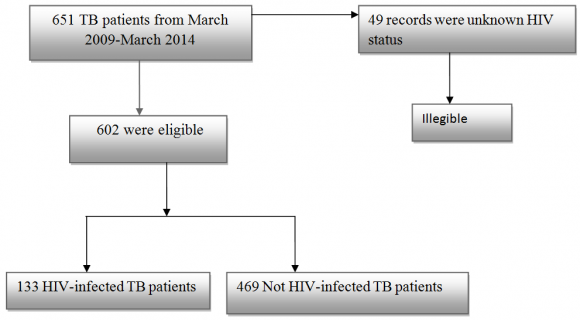
Sample size: Medical records of all TB patients who were on anti tuberculosis treatment from March, 2009 to March, 2014 were included in the study. There were a total of 651 patients in the TB clinic in a given five years. Of these, 602 of patients were included in the study. One hundred thirty three (133) of them were TB-HIV coinfected cases and the remaining 469 were diagnosis only TB cases. Exclusion criteria: Unknown HIV status and incomplete records were excluded in the study.
Data quality control: Before study conducted, orientation was given for supervisor and data collector nurses concerning to standardized checklist, the purpose of the study, techniques and procedures of data collection methods. The researcher gave a guideline for data collectors and the supervisor for data collection process. The supervisor was monitoring the data collection process.
Data processing and Analysis: Before data entry, data were monitored and checked for its completeness by the supervisor and each completed checklist was coded on pre-arranged coding sheet by the researcher. Data were entered into Epi Info version 3.5.1, then exported and analyzed by using SPSS Windows software (version 16.0). Data were cleaned for its consistency by running simple frequencies and percentage. Then, printed frequencies were used to check for outlier and to clean data. Tables and graphs were used to present data frequencies and percentage. It also used to describe the study population in relation to relevant variables.
Stepwise bivariate and multivariate logistic regressions techniques were used to analyze data and control the adverse effects of confounding variables. The crude and adjusted odds ratios together with their corresponding of 95% confidence intervals were computed. A P-value < 0.05 was considered to declare a result as statistically significant.
Ethical consideration: Ethical approval and clearance was obtained from Debre Markos University, medicine and health Science College ethical review board. A formal letter for permission and support were obtained to Fenote Selam district hospital administrator. Then, the hospital administrator wrote a letter to the TB clinic focal person.
3. III. Results
4. a) Socio-demographic characteristics of study participants
A total of 651 patients were registered in the TB clinic from 2009 to 2013/14.
Of the total, 602 participants were included in this study. Of these patients, 133 (22.1%) were TB-HIV co-infected and 469 (77.9%) were only TB cases. The majority of participants were in the age groups of 15-24 and 25-34 years old which accounts 160(26.6%) and 163 (27.1%) respectively. Of the total participants 328(54.5%) were males. The urban participants were accounted about 367(61%) (Table1).
Table1: General characteristics of the study participants registered at Fenote Selam district Hospital TB clinic, Amhara, Northwest Ethiopia, 2014. In bivarate analysis, age group from 15-24 and 25-34 years old were 2.544 and 3.409 times likely to be risk of TB-HIV co-infection ,respectively, as compare to age groups ?55 years old. And also cured and died were 2.733 and 4.603 times risk for TB-HIV confection, respectively, as compare to completed treatment outcomes.
5. Characteristics of variables
After controlling the confounder variables through multivariate logistic regression analysis, age groups 15-24 years (AOR: 2.586, 95% CI: 1.010, 6.617) and 25-34 years (AOR: 3.370, 95% CI: 1.332, 8.525) were independently associated with TB-HIV co-infection. Died (AOR: 4.326, 95% CI: 2.039, 9.176) and cured (AOR: 2.758, 95% CI: 1.456, 5.227) were independently associated with TB-HIV co-infection (Table 2).
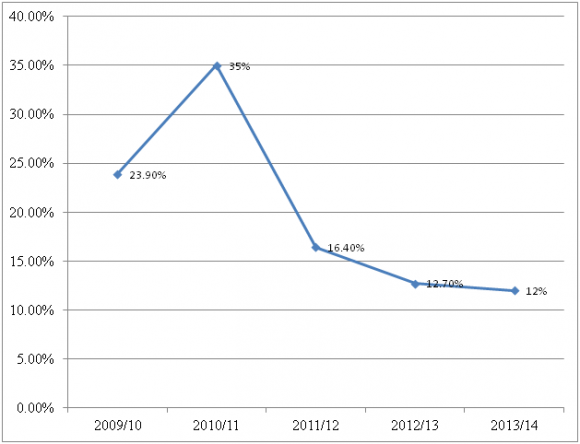
Trend of TB-HIV co-infection increased from 23.9% to 35% in the years 2009/10 -2010/11 and decreased from 35% to 12% in the years 2011/12 -2013/14 (See figure 2 below).
This study showed that the prevalence of HIV co infection among TB patients was 22.1%. This is nearly similar to a study done by Daniel G D et.al. [10]. However, this finding is higher than a report by WHO in 2012(13%), report of WHO in 2012 for Ethiopia (8%) [11] , in northwest Ethiopia ( Dabat) 11.4 % [12]. On the other hand, this is lower than the studies conducted in sub-Saharan African countries which were 70%[13], a study conducted in Nigeria (44.2 %) [14] and study conducted in Debre Markos, Ethiopia 44.8% [15]. This discrepancy might be due to a preference of patients towards quality of care at referral hospital, especially, when the disease becomes serious and complicated, as compare to care in district hospital. The other possible reason might be due to fear of stigma and discrimination that they may seek care away from their village in the bigger town.
In this study, that treatment success was 71.9%. In line with this, a report showed in India, treatment success of TB-HIV co-infection was 74.5% [16]. This may be due to similar in socio-economical status of the study participants and universal implementation of DOTS program throughout the world.
Gender had no significant difference on TB-HIV co-infection. Similarly, the study conducted in Addis Ababa, Ethiopia, showed that no significant difference between male and female [17]. This could be due to similarity in socio-cultural perspective of study participants.
In contrast, the study conducted in Dabat, Ethiopia [12], Northwest Ethiopia [18] and São Paulo state [19] indicated that TB-HIV co-infection case was higher in men than women. Besides, Tabarsi et al. found that the TB-HIV co-infected intravenous drug user were males [20]. This attributed that males are economically active and influential in the community and they may smoke, drink and have multi-sexual partners.
This study showed that 8.5 % of patients were died. This is lower than study conducted in Malaysia 23.3% [21], Thailand 29 % [22], and in Vietnam 26% [23]. This may be due difference sample size and may be due to socio-cultural and economical difference.
This study showed that there is no significant difference in the rate of HIV infection among type of TB. Similarly, study conducted in Ethiopia showed that there was no significant difference among type of TB [10; 24]. However, other studies indicated that rates of HIV infection among smear-negative and EPTB cases were higher than smear-positive cases [25; 26]. This could be due to the relatively low prevalence of HIV infection in the catchment area of the study population. Another possible explanation could be under diagnosis of TB This study revealed that study participants in age groups of 15-24 and 25-34 years old were independently associated with outcome variables. This is similar to previous study conducted at Debre Markos referral hospital [15]. The fact is that these age groups are more active for sexual activity and they are vulnerable to HIV infection than any other part of the population.
According to the study conducted at Debre Markos referral hospital showed that TB-HIV co-infection was 49.2% in 2008/9, 42.7% in 2009/10, 39.3% in 2010/11, 32.9% in 2011/12, 44.6% in 2012/13, and 44.8% in 2013. This result showed that there was a decreasing trend from 2008 to 2011 and some increasing trend from 2012 to 2013 of TB-HIV coinfection [15]. This study revealed that the trend of TB-HIV co-infection was increased from 23.9% to 35% from 2009/10 to 2011/12, respectively; then decreased from 35% to 12% from 2011/12 to 2013/14. This is due to intensive provision of INH prophylaxis to prevent opportunistic infection of TB as soon as they detect HIV positive. The other possible explanation may be due to the current strategic plan of the ministry of health in Ethiopia, which expands health facilities across the country and increased awareness of the community through health education and mass media on prevention and control of HIV.
6. V. Conclusion
The overall result of TB-HIV co-infection was 22.1%. The age groups of15 -24 and 25-34 years old which accounts 27.2% each, TB-HIV co-infection was strongly associated with death, defaulted and TB categories. The age groups 15-24 and 25-34 years old were 2.544 and 3.409 times likely to be risk of TB-HIV co-infection as compared to the age groups ?55 years old. Died and cured were independently associated with TB-HIV co-infection as compared to completed treatment outcome.
This study showed that there was increasing rate of TB-HIV co-infection from 23.9% to 35% in the year 2009/10 to 2011/12 then decreasing from 35% to 12% in the year 2011/12 to 2013/14. The main reason is that provision of INH prophylaxis to prevent opportunistic infection of TB as soon as they detect HIV positive. The other reason may be due to expanded health facilities across the country, the increased awareness of the community through health education according to current strategic plan of the federal ministry of health of Ethiopia. Generally this study shows relatively lower TB-HIV co-infection than a number of other studies held in different countries in sub-Saharan African.
7. VI. Recommendations
The author of this study suggested that health education should be given for the community on mode of transmission of TB, prevention of HIV infection, impact of TB-HIV co-infection on TB treatment outcomes and productivity of population and national country. Besides this, regional health bureau, zonal health department, higher officials should create networking the health facilities each other to identify treatment outcome of the referred patients. In addition, the data registration system of patients should be improved to include patients' personal practice like smoking habits, alcoholism and chronic illness. This should also be collected by health professionals as they interview patients.
8. VII.
9. Acknowledgement
The author would like to thanks all data collectors and supervisors for thier assistance to me on data collection. Secondly, my sincerely appreciation extends to Adugaw Dessie for his unpreserved constructive comment. Next to this my appreciation goes to Debre Markos University, Medicine and Health Sciences College for proper review and approval of this paper. My gratitude thanks goes to Fenote Selam District Hospital official and TB clinic focal person and data collectors for their cooperation and assistance.