1.
Genitive Communication -Anogenital Warts -Condylomata Acuminatum Anubha Bajaj I. Preface uman Papilloma Virus (HPV) is a miniature DNA (deoxy ribonucleic acid) virus of the family Papovaviridae which primarily access the squamous cells. The categories of HPV exceed a 100 (11) . Histological transformation and infiltrative malignant neoplasm in the vulva and anogenital area such as Condyloma, Verrucous lesions, tiny Papules or Plaque like modification and Vulvar Intraepithelial Neoplasia (VIN) are elucidated with various HPV classes. Condylomata acuminatum is a classic, well differentiated lesion which exemplifies acanthosis, hyperkeratosis, parakeratosis, dyskeratosis with koilocytosis (2) . Bowenoid papulosis comprises of multiple, red -brown genito-anal papules with epidermal adaptations identical to the Bowen's disease on histology. Malignant conversion has been scripted in what is essentially a benign disease (10) . Female companions of males contaminated with the virus display an enhanced probability of cervical cancer (4) . Histopathology and Serological investigations may be required as the clinical elucidation may be inadequate. Classification of the high risk genotypes of HPV is desirable due to the affiliation with cervical cancer and bowenoid papulosis. Anogenital warts (condylomata acuminatum) are a viral disorder with a frequent sexual transmission. Women are implicated in two-thirds of the patient population, though both sexes are afflicted.
2. II. Causatum and Prospects
Condylomata acuminatum commences from the Human Papilloma Virus (HPV), a family of highly contagious double stranded DNA viruses, essentially exhibiting a sexual transmission. Lesions appear in 3 weeks to 8 months after initial exposure. Majority of the infections are transitory and dissipate within 2 years. Almost 35 sub-categories of HPV are limited to the anogenital epithelium with a probability of malignant conversion such as cervical and anal cancer (5) . High risk serotypes 16 and 18 collaborate with low risk subtypes of HPV such as 6 & 11 to elucidate benign condylomas and low grade intra epithelial neoplasia without incorporating in the host genome. Intermediate risk HPV subtypes delineate a high grade dysplasia which may persevere with negligible evolution and invasion.
Author: e-mail: [email protected] Condylomata emerge from sexual activity Digital / anal, oral / anal and digital / vaginal contact possibly disperses the virus besides various fomites. Immune suppression predisposes to the disorder. The contamination in women is largely transmitted by vaginal intercourse. Anal condyloma may evolve from vulvar or perineal infections or by recipient anal intercourse. Numerous sexual participants enhances the occurrence of the disease (condylomata 7 times frequent and recurrent condylomata 12 times) in contrast to a singular partner with equivalent predisposition in both the genders. Previous exposure to a sexually transmitted disorder or oral herpes is concordant with a possible condyloma. The cavity of the prepuce or the penile shaft is implicated in the heterosexual or homosexual process. Heterosexuals may elucidate perianal lesions, although these are usually encountered in the homosexuals. Condylomas are preponderant in the HIV (human immune deficiency virus) infected individuals besides those with variants of STD (7%) and may evolve into a squamous cell carcinoma if the contamination persists. Diminished CD4 T lymphocyte count (<500 cells/µl) and frequent administration of drug injections may elucidate a vulvovaginal or perianal lesion. Efficacious antiretroviral therapy reduces the incidence of these lesions.
3. III. Scientific Indications
Condylomata acuminatum manifests clinically contingent to various lesions with pertinent locations. A smattering of warts frequently lack characteristic features. However patients exhibit itching, bleeding, burning, localized tenderness, pain and vaginal discharge (in females). Occasionally, exophytic and extensive warty clusters are evidenced which may impede defecation, intercourse or vaginal delivery. Proximal anal canal configurations may incite a stricture.
4. IV. Interpretation
Visual inspection of the site of involvement is recommended. Smooth, flattened, skin coloured or pink papules or verrucous papillae may be encountered. Anoscopy, Sigmoidoscopy, Colposcopy and/or a Vulvovaginal examination is indicated to evaluate the magnitude of the disease. High resolution anoscopy is frequently employed to augment tissue visualization. Application of 5% acetic acid produces a pearly white H lesion which simplifies the recognition of the lesion, though the measure is non-specific.
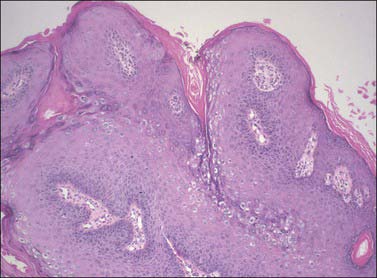
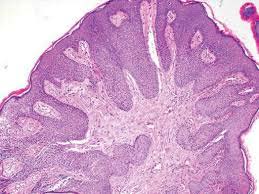
5. V. Histopathology
Condylomata acminatum or venereal warts (commonly an HPV 6 genesis) develop in the vicinity of the anus, vulva, glans penis and mucosal membranes such as the oral cavity. Focal epidermal hyperplasia is substantiated by hyperkeratosis, parakeratosis, varying or extensive acanthosis and papillomatosis. Trichilemmal type of keratinisation may emerge (13) . Vacuolated cells may be visualized in the upper malphigian layer in the early lesions. Atypical cells, characterized by abundant, eosinophilic cytoplasmic accumulations may be demonstrated. Miniature vacuolated cells and pyknotic nuclei are exhibited in the thick, basal stratum corneum (13) . Ancient verrucae may emerge as papillomas or keratosis. Flat warts with involution display a degenerative epidermis and a prominent mononuclear dermal or intra-epidermal inflammation. The viral nuclear inclusions are basophilic. They can be established with immunohistochemistry and in-situ hybridization procedures. The eosinophilic aggregates in the cytoplasm are indicative of aggregated tonofilaments. In concordance with the HPV induced lesions, benign or malignant skin tumours or tumour like conditions manifest, such as seborrheic keratosis, bowen's disease, invasive squamous cell carcinoma and epidermodysplasia verruciformis. The keratinocytes reveal altered keratin on account of the viral infection and further alterations ensue with malignant conversion. A biopsy may be contemplated with ambiguous lesions, in the patients refractory to therapy, in immune-deficient individuals, with extensive lesions or lesions which elucidate atypical components. A routine biopsy can be advocated to investigate a dysplasia.
6. VI. Determinants
Detection of the subtypes of the contaminant HPV is essential to specify the patients which may progress to squamous cell carcinoma. Anogenital tumours induced by HPV may be clinically challenging and troublesome to diagnose and treat. Determination of the virus incorporates In situ hybridization (ISH), Southern blot hybridization method, Dot blot hybridisation, Polymerase Chain Reaction (PCR) and real-time PCR. However the technique of ISH for diagnosing the HPV is inferior and insensitive. Besides PCR and real time PCR require valuable machinery such as a thermal cycle (8) . A Hybriobio geno array test for HPV genotyping can be utilized as a commercial kit. It is an expeditious, efficacious, specific and sensitive technique to ascertain the HPV DNA. The test displays a decisive concordance which exceeds that of 95% with the interpolation of the commercial kit and the viral DNA sequencing. The concurrence of the real time PCR and viral DNA sequencing is around 95%. Viral DNA sequencing is the gold standard. The real time PCR is a dependable, sensitive and a specific investigation to discover the infections created by the high risk and low risk HPV genotypes (6) .
7. VII. Distinguishing Diagnoses
Condylomata acuminatum requires distinction from condylomata lata, a pattern of condyloma which develops in secondary syphilis. Condylomata lata delineates flat and velvety lesions. Generally, micropapillomatosis of the vulva ensues. A solitary base abuts each individual papillary projection, in contrast to the condylomata acuminatum where multiple papillae emerge from a singular base. Verrucous lesions, which are painful and perianal, develop in concurrence with the contamination of Herpes Simplex virus and HIV infection. Anogenital squamous cell carcinoma may coincide with condylomata acuminatum. Ulcerated and ambiguous lesions require a biopsy. Lesions with three previous treatment protocols or if unresolved within six months of therapy require a histological re-assessment. Immune-deficient patients, those beyond 40 years of age, pigmented, anomalous lesions also necessitate a re-evaluation. Demarcation is also required from disorders such as hymenal remnants, vulvar intraepithelial neoplasia (in women), molluscum contagiosum, skin tags and angiofibromas.
8. VIII. Therapies Numero Uno
Three major modalities are instituted: Chemical or Physical destruction, Immune therapy and Surgical excision. Topical anti microbial agents have a restricted collusion. The number and magnitude of lesions dictate the mode of therapy. However, the therapeutic interventions for genital warts may be inadequate as the reoccurrence is up to 30-70 % within 6 months. Spontaneous retrogression may occur within 3 months in 20-30 % cases. An exceptional or a pertinent treatment option for the entire panorama of warts is nonexistent. Trichloracetic acid or podopyhllin may be applied to the warts. Imiquimod, podophyllin or
( D D D D )C extended patient analysis is then required. Self application of imiquimod or podofillox is beneficial in the absence of trichloracetic acid or podophyllin. Surgical intervention is recommended for enormous lesions. (Gynaecologic / Anorectal surgery).
Chemical agents incorporate podophyllin, trichloracetic acid or 5 fluorouracil / epinephrine gel. Podophyllin is a decoction of podophyllum peltatum, comprising of an anti mitotic agent podophyllotoxin which arrests the cell cycle in metaphase with consequent cell demise. A 0.5% concentration of podofilox / podophyllotoxin can be employed. Reoccurrence occurs in 43% individuals in 12 weeks. Trichorlacetic acetic (TCA) decimates the wart by protein coagulation in 80 to 90% cases. 5 Flurouracil / Epinephrine gel is a pyramidine antimetabolite that mediates in DNA synthesis, arrests the methylation of deoxy uridylic acid thereby resulting in cellular demise. Intra-lesion injection of epinephrine enhances the resolution of the warts, particularly with integrated therapy. At 3 months 50-60% lesions tend to reoccur.
9. IX. Immune Modulation
Imiquimod and interferon alpha are dual immune modulating agents which can be utilized. Imiquimod is an immune transformer which activates local cytokines. Vulval and Anal intraepithelial neoplasia may be managed with the same. Interferon Alpha, when employed with for systemic therapy comprehensively remedies the anal condyloma in 25-80% individuals. Ancillary alpha interferon therapy in conjunction with the 5 fluorouracil cream or laser ablation elucidates a reoccurrence of 6% in contrast to a figure of 24% with no additional treatment.
10. X. Surgery
Excision or surgical ablation is optimal with the non performance of medical therapy and for warts susceptible to surgery. Cryotherapy is an outpatient technique which employs liquid nitrogen spray. Laser therapy necessitates an operation theatre or a mobile surgical and anaesthetic service. The warts are disposed of in a 100% cases (33), nevertheless reoccurrence ensues in 45%. Surgical intervention is an exorbitant procedure for treating warts.
11. XI. Excision Modalities
Knife or scissor excision requires anaesthesia. Infection and haemorrhage may probably emerge. Complete eradication occurs in 36% cases. Condylomata acuminatum treated with excision requires evaluation for squamous cell carcinoma. Antimicrobials can be topically adopted inclusive of Cidofovir and Bacille Calmette Guerin (BCG). Cidofovir competitively restricts the viral Deoxy Ribonuclease (DNA) by incorporating viral DNA polymerase. The drug mediates and prevents the extension of the DNA. Bacille Calmette Guerin (BCG) elucidates a partial or a negligible recovery.
12. XII. Infrared Coagulation
Tissue coagulation is attained by a narrow beam of infra red light focussed within a probe. Hemorrhoids, tattoos, chronic rhinitis, ablation of common warts and anogenital condylomata (82%) are benefitted by the modality. Reoccurrence can be managed with excision or fulguration. A partial biopsy is required for evaluating malignant conversion. Cryotherapy may be employed subsequent to recovery. Ancillary treatment with imiquimod cream is recommended.
13. XIII. Conclusion
Human Papilloma Virus (HPV) appertains to the Papillomaviridae family, a divergent class of viruses which contaminate the skin and the mucosal epithelium of numerous vertebrate species. Forty kinds of HPV pertaining to the genus papillomavirus have been identified. These contaminate the epithelium and mucosal lining of the anogenital tract (1) . HPV subtypes are categorized as per the probability of malignant transformation as low risk or high risk. Low risk HPV subtypes (HPV 6 & 11) produce common genital warts such as condylomata acuminatum, benign hyperproliferative lesion and a controlled development of malignancy. Condylomata acuminatum are discovered with HPV 6 or 11 or both in 90% individuals and with HPV11/18 in about 4% cases. Concomitant infection by dual DNA subtypes can be detected by Hybribio HPV geno array test or viral DNA sequencing. Numerous HPV genotypes are ascertained with the Bowenoid Papulosis consisting of HPV 16,18,31,35,39,42 and 48(5). HPV 16 contamination is particularly connected with the squamous cell carcinoma in situ of the external genitalia such as Bowen's disease and Erythroplasia of Queryat (9) .