1. Introduction
hock is the clinical expression of circulatory failure that results in inadequate cellular oxygen utilization. 1 Shock is a common condition in critical care, affecting about one third of patients in the intensive care unit (ICU), both over resuscitation and under resuscitation can adversely impact the outcomes. 2,3,4 End point of resuscitation has always been a matter of debate, initially continuous SCvo2 monitoring as introduced by Rivers et al had the obvious limitation that normal/high values cannot discriminate whether delivery is adequate or in excess to demand 5,6,7 . High ScvO2 profiles have even been shown to be related to elevated blood lactate concentration and poor survival rates. 8 Lactate cannot differentiate between different etiologies of shock and it can get elevated in various other conditions. 9 Carbon dioxide (Co2) is highly diffusible and can be a marker of adequacy of venous return, the central venous and arterial CO2 gap, as an easily available clinical monitoring tool. Observational study has shown that Persistence of such a large pCO2 gap after 24 hours of treatment was predictive of higher mortality. 10 In conclusion, determining the PCo2 gap during resuscitation of critically ill patients is useful in deciding when to stop resuscitation. 11 Central venous-arterial carbon dioxide difference (PCO2 gap) can be a marker of cardiac output adequacy in global metabolic conditions that are less affected by the impairment of oxygen extraction capacity. Assessing the adequacy of oxygen delivery with oxygen requirements is one of the key-goal of hemodynamic resuscitation. Clinical examination, lactate and central or mixed venous oxygen saturation (SvO2 and ScvO2, respectively) all have their limitations. Many of them may be overcome by the use of the carbon dioxide (CO2)-derived variables. The venoarterial difference in CO2 tension ("Î?"PCO2" or "PCO2 gap") is not an indicator of anaerobic metabolism since it is influenced by the oxygen consumption. By contrast, it reliably indicates whether blood flow is sufficient to carry CO2 from the peripheral tissue to the lungs in view of its clearance: it, thus, reflects the adequacy of cardiac output with the metabolic condition. We investigate the relation between be determined objectively as we get more substantial evidence supporting the fact that both under resuscitation and over resuscitation is detrimental to overall outcomes. Since carbon dioxide is more diffusible than oxygen it readily gets in to the blood in low perfusion states whereas oxygen doesn't. Hence widening the PCO2 gap. Since this PCO2 gap can be determined easily in the ICU we propose that PCO2 gap can be used as a reliable indicator of endpoint of resuscitation and predictor of mortality in patients with shock.
Aim: To evaluate the association between PCO2 gap and outcome of resuscitation in patients with shock. The Objectives of the project are to study the association between PCO2 difference and in-hospital mortality in patients admitted with shock and to study the correlation between PCO2 difference and lactate clearance.
Materials and methods: 71 adult patients presenting with shock to our ER were enrolled in the study. They were resuscitated according to standard protocols. PCO2 gap was measured at presentation, then every 2 hours until the resolution of shock which were correlated to the lactate clearance, hemodynamics and the IVC index of the patient. The data was then analyzed using the R software and logistic regression was done to analyze various factors associated with mortality. P value less than 0.05 was considered statistically significant.
Results: The correlation between pCO2 gap and the in hospital mortality was statistically significant at 0,2,4,6 and 24 hours. The correlation between pCO2 gap and the end point of resuscitation was statistically significant at 2,4,6 and 24 hours implied by the pearson's correlation. We also found a positive correlation between PCO2 gap and lactate clearance which was statistically significant.
2. Conclusion:
The PCO2 gap can be used a marker of the adequacy of the cardiac output in patients with shock. Using pCO2 gap has potential to avoid administration of unnecessary fluids and inotropes in patients, who have lactate elevated in the absence of tissue hypo perfusion. We suggest using pCO2 gap as a complementary tool to evaluate the adequacy of blood flow to global metabolic demand. A high pCO2 gap on initial presentation was associated with high mortality rates. So it can be used as a predictor of outcomes in patients with shock.
3. PCO2 gap -
4. Review of Literature
Shock is defined as inability to maintain MAP which is refractory to fluid resuscitation. It has a guarded prognosis, there are many upstream and downstream markers for resuscitation, septic shock guidelines endorses Lactate as a prognostic marker; has got its own limitations as it can be elevated in other clinical conditions9 and it cannot differentiate the cause of shock9. With enough evidence coming up about over resuscitation and positive balance being one of the predictor of mortality there is a need for ideal resuscitation marker which can be easily employed bedside with present day equipment used on day to day basis.
CO2 is the end product of aerobic metabolism, PCO2 in the venous blood reflects the global tissue blood flow relative to metabolic demand. CO2 is about 20 times more soluble than O2 so it more reliably diffuses out of ischemic tissues into the venous effluent making it a sensitive marker of hypoperfusion in situations where an O2 diffusion barrier exists (e.g. nonfunctional and obliterated capillaries), "masking" poor O2 extraction (O2ER) and increased tissue O2 debt, CO2 still diffuses to the venous effluent, "unmasking" the low perfusion state for the clinician when venous-toarterial CO2 difference is evaluated the gap is a marker of adequacy of venous blood flow to remove CO2 produced rather than a marker of tissue hypoxia or dysoxia 11
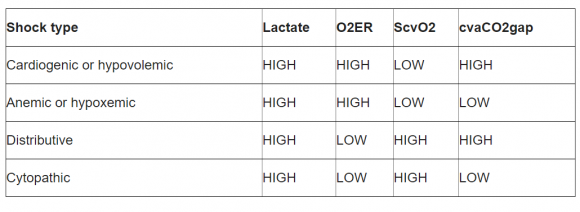
5. Table 1: PCO2 Gap in Different Shock States
Conversely, in HH, pCO2 gap did not increase in spite of a marked VO2 and VCO2 reduction. 12 There is a good correlation between Mixed CO2 and Central CO2 difference with Arterial CO2 as demonstrated by Van Beest et al in severe sepsis and septic shock patients, hence Central CO2 can be substituted for mixed CO2 for determining the CO2 gap which acts as surrogate marker for Cardiac Index. 10 Cushieri J etal conducted study in ICU patients to see the correlation between Central Venous and Arterial CO2 gap and Cardiac index determined by thermodilution technique and showed statistically significant correlation. 13 Hence CO2 gap can be used as a marker of Cardiac output.
6. a) Role in Sepsis
In sepsis although Cardiac output may be normal but regional compromise of circulation is well documented phenomenon which may lead to increase in CO2 secondary to micro-circulation compromise. P(cv-a)CO2 could be considered as a better indirect assessment of systemic blood flow than ScvO2 in resuscitated-septic shock patients. 14 A cutoff value for pCO2 gap of 0.8 kPa (6mmHg) discriminated between high and low lactate clearance and CI. 15,16 In study done by Vallee et al done in septic shock patients compared When the 70% ScvO2 goal value is reached, the presence of a P(cva)CO2 larger than 6 mmHg shown to be an useful tool to identify patients who still remain inadequately resuscitated. 14 We hypothesize that CO2 gap is non inferior to lactate clearance in resuscitation of critically ill patients.
As illustrated in table 1, Lactate is high in all types of shock, PCO2 Gap is high in cardiogenic and distributive shock which is amenable to fluid resuscitation and inotropic support and low in hypoxemic and cytopathic shock where fluid resuscitation has no role thus it can be concluded that PCO2 gap is useful in determining when to start and stop fluid resuscitation. 11 Co2 gap is a marker of adequacy of venous blood rather than marker of tissue hypoxia or dysoxia as shown by Vallet et al in an experimental model of isolated limb in which ischemic hypoxia (IH) and hypoxic hypoxia (HH). The authors demonstrated that when DO2 was reduced beyond its critical threshold in IH (dysoxia), this was associated with an increased limb venous-to-arterial PCO2gap. 12 III.
7. Research Question
Would pCO2 gap serve as an ideal bedside marker to predict the outcome of resuscitation in a patient with shock?
V.
8. Methods and Methodology
9. Statistical Methods
10. a) Sample Size Calculation
Sample size was calculated using nMaster software v2.0
In a study done by Beest PV et al, the mortality of patients with sepsis was 24.5% (13 out of 53) and risk of mortality for those with high PCO2 gap ranged from 1.6 to 5. 3 Keeping a conservative value in odds ratio as 2.5, with power of 80% and 5% alpha error the minimum required sample size is 71.
11. b) Statistical Analysis Plan
Data was analyzed using R software. Continuous variable were described using mean and standard deviation. Categorical variables were described using frequency and percentage. Patients were categorized based on PCO2 difference and logistic regression was done to analyze various factors associated with mortality. Correlation between PCO2 difference and lactate was done using appropriate statistical methods. P value less than 0.05 was considered statistically significant.
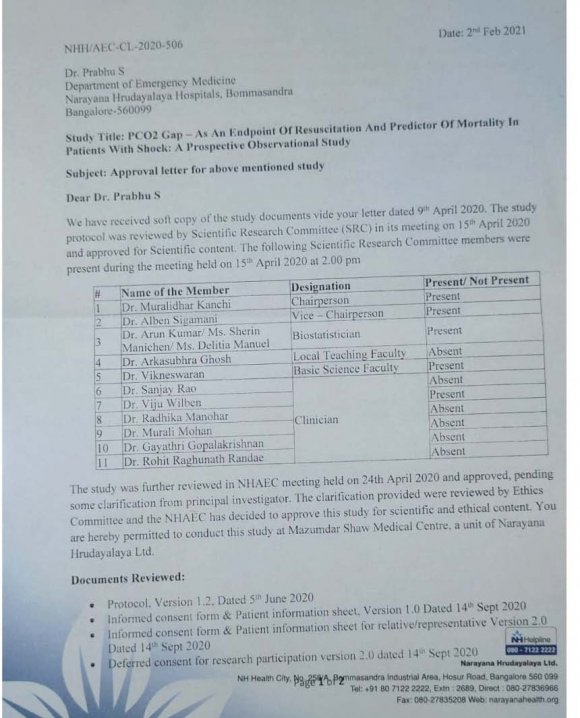
12. c) Ethical consideration
Ethical clearance was obtained prior to the study from the ethics committee of the institution. Informed consent was obtained from the patient or guardian before the onset of study. Confidentiality of
13. Aims and Objectives
Aim of the Project: To study the association between PCO2 gap and outcome of resuscitation in patients with shock.
Objectives of the Project: The Objectives of the project are as follows:
? Primary objectives-To study the association between PCO2 gap and in-hospital mortality in patients admitted with shock.
? Secondary objectives ? To study the correlation between PCO2 gap and lactate clearance. ? To study the role of PCO2 gap as a marker for endpoint of resuscitation in patients with shock.
patient details are and will be maintained. It was explained to the patient that the study is purely descriptive and merely for data collection. There is no intervention required specifically for the study. Management of these patients were along the standard international guidelines. As the study did not involve any extra procedure, no compensation was offered during and after the study.
VIII.
14. Results
A total of 71 patients were enrolled in the study. 7 patients died from the 48 to 72 hours time period. Their samples were collected and analyzed till the 24th hour of admission. The mean age of the patients was 54 years (SD 16.2; range 18-81 years). The primary outcome of the study was the correlation between the PCO2 gap and the in hospital mortality at each of the sampling time points. The correlation between the PCO2 gap and the in hospital mortality was positive at 0, 2, 4, 6 and 24hours. The correlation was statistically significant at 0 and 2 hours. (Table 2) There was a statistically significant negative correlation between end point of resuscitation and pCO2 gap at 2h,4h, 6h and 24 hours as implied by the Pearson's correlation in Table 3.
15. Discussion
The association of lactate accumulation and oxygen debt during shock states has been described for decades15. Throughout the years, there has been continued interest in refining resuscitation triggers, and response to therapy. Lactate clearance as an endpoint of resuscitation is supported by at least two multi-center studie 16,17 .
However, lactate clearance has disadvantages as lactates can sometimes be normal in septic shock 18 , lactate elevation not solely due to oxygen delivery-consumption mismatch and it has different prognostic implications based on the initial value.
It was recognized in sepsis that pCO2 gap (or its mathematical derivatives) outperformed other markers in detecting tissue hypoperfusion 13,[19][20][21] . The arterial carbon dioxide is dependent on the pulmonary gas exchange and the venous carbon dioxide is dependent on the blood flow to the tissue 22 . So, when the flow reduces in low cardiac output states like shock, the difference between the venous and arterial carbon dioxide increases. It has been demonstrated that the pCO2 gap increases in various types of shock. 2 In our study we found a statistically significant correlation of pCO2 gap at 0 hour and and 2nd hour of resuscitation and mortality in patients. It shows that high pCO2 gap on initial presentation can be used as a predictor of outcomes in patients with shock. Ospina-Tascón, G.A. et al., 24 found that the persistence of high PCO2gap during the early resuscitation of septic shock was associated with higher 28 day mortality.
We also found that there was a statistically significant correlation between end point of resuscitation and pCO2 gap at 2h,4h, 6h and 24 hours. Hence, pco2 gap can be used as an endpoint of resuscitation in patients with shock. This was similar to the findings of Vallet B et al., 11 who found that determining the gap during resuscitation of critically ill patients is useful when deciding when to stop resuscitation.
Our analysis also showed that PCO2 gap at various time points had positive correlation with lactate clearance. This was similar to a study done by Shyam M et al., 25 who showed that the PcvCO2-PaCO2/CaO2-CcvO2 ratio and lactate are positively correlated during the first 24 hours of active resuscitation from sepsisinduced hypotension, Pco2 gap is not inferior to lactate levels as a hemodynamic marker. It can be substituted in place of lactate levels to predict outcomes in patients presenting with shock. It can also be used as a guide for therapy to achieve endpoint of resuscitation.
X.
16. Limitations
Our study has its limitations. It is a descriptive study without randomization of the patients. Also some technical aspects should be kept in mind when these indices are used in clinical practice. First, some errors in the PCO2 gap measurements may occur when sampling the venous blood: incorrect sample container, contaminated sample by air or venous blood or catheter fluid. Second, a too long delay of transport of blood sampling may significantly change the blood gas content at the venous and the arterial site.
17. Summary and Conclusion
The PCO2 gap can be used a marker of the adequacy of the cardiac output in patients with shock. Using pCO2 gap has potential to avoid administration of unnecessary fluids and inotropes in patients, who have lactate elevated in the absence of tissue hypo perfusion. We suggest using pCO2 gap as a complementary tool to evaluate the adequacy of blood flow to global metabolic demand. A high pCO2 gap on initial presentation was associated with high mortality rates. So it can be used as a predictor of outcomes in patients with shock. There may be some words that you do not understand. Please ask me to stop as we go through the information and I will take time to explain. If you have questions later, you can ask them of me, or the staff.
18. List of abbreviations
19. ICU
pCO2 gap is the difference between the venous and arterial carbon dioxide. When a patient presents with shock, they will be treated with IV fluids or medication to increase blood pressure (inotropes) by constriction of blood vessels depending upon the cause of the shock. To know when the shock has resolved, we are going to compare pCO2 gap to other parameters which have been previously established.
20. Purpose of the research
To evaluate if pCO2 gap can be used to predict mortality and marker for end point of resuscitation
21. Participant selection
We are inviting all adults with shock to participate in the research on pCO2 gap.
22. Voluntary Participation
Your participation in this research is entirely voluntary. It is your choice whether to participate or not. Whether you choose to participate or not, all the services you receive at the hospital will continue and nothing will change. You may change your mind later and stop participating even if you agreed earlier.
23. Procedures and Protocol
Once you understand the study and give consent, your pCO2 gap will be measured on presentation, 2nd hour, 4th hour, 6th hour and at 24th hour. Patients presenting with shock will have an arterial line for invasive blood pressure measurement and a central line for administration of inotropes to treat the shock. Blood samples from these lines will help us to measure pCO2 gap. Treatment will be given for the shock as per standard guidelines and hospital protocol according to the patient's condition. Other parameters such as mean arterial pressure, IVC collapsibility, lactates will be compared to find out if pCO2 gap has a good correlation for endpoint of resuscitation (resolution of shock)
24. Duration
The research takes place over the course of 1 year. You will be followed up for12 to 24 hours depending upon your clinical condition.
25. Side Effects
No new intervention or procedure is done for the study. You will already have lines from which blood samples will be taken. Hence there are no side effects for the study.
26. Risks
No additional risks and discomfort will be caused during this study.
27. Benefits
The findings of this study can change the views of using pCO2 gap as an endpoint of resuscitation. I confirm that the participant was given an opportunity to ask questions about the study, and all the questions asked by the participant have been answered correctly and to the best of my ability. I confirm that the individual has not been coerced into giving consent, and the consent has been given freely and voluntarily.
A copy of this ICF has been provided to the participant.
| ? Screening 2D-echocardiography was done at the | |||||
| emergency department and inotropic agent was | |||||
| decided based on heart contractility. | |||||
| ? Patient demographic details, diagnosis, SOFA | |||||
| Score, was done in the first 6 hours of resuscitation | |||||
| (two hours apart) and the data was collected. | |||||
| Lactate and Co2 Gap were captured and | |||||
| documented after 24 hours of resuscitation. | |||||
| ? Aim of resuscitation was to target MAP of 65 mm Hg | |||||
| and two stable lactate values 2 hours apart. If | |||||
| lactates had not improved then further fluid boluses | |||||
| were decided upon reviewing pulmonary congestion | |||||
| in ultrasound (M mode of lung will be done and if B | |||||
| lines are more than 4 then it is indicative of | |||||
| pulmonary congestion). The corresponding CO2 | |||||
| Gap was noted. | |||||
| ? First choice of vasopressor was nor-adrenaline as | |||||
| per the standard infusion dose. If patient requires | |||||
| vasopressor support despite fluid boluses then | |||||
| steroid in the form of injection Hydrocortisone 50mg | |||||
| IV every 6th hourly was administered. | |||||
| ? Antimicrobial | administration | and | further | ||
| management was decided by clinical examination | |||||
| and supportive investigations as per clinician's | |||||
| judgement. | |||||
| Study population: ? Inclusion Criteria | Data collection methods: Proforma Data collection forms: Attached | ||||
| ? All adult patients (more than 18 years of age) in | VII. | ||||
| shock requiring vasopressor to maintain MAP of | |||||
| 65mmHg, having a central venous access and | |||||
| arterial line. | |||||
| ? Exclusion Criteria | |||||
| ? Patient Refusal | |||||
| ? Pregnancy | |||||
| ? Advance directive with consensus against active | |||||
| resuscitation | |||||
| ? Disseminated Malignancy | |||||
| Sample size: 71 | |||||
| Study design: Prospective observational study. | |||||
| Study intervention: No interventions | |||||
| Study duration: One Year | |||||
| VI. | Methodology | ||||
| ? All shock patients were resuscitated according to | |||||
| the standard protocol with fluid bolus of 30 ml/kg | |||||
| over 1 hour and guided therapy with fluid challenges | |||||
| targeting heart rate, base deficit, urine output and | |||||
| pulmonary congestion as per routine clinical | |||||
| practice. | |||||
| ? Lactate clearance was documented every 2nd | |||||
| hourly and VBG from Central line and ABG from | |||||
| Radial Line was analyzed at the same time and CO2 | |||||
| gap was checked every 2nd hourly. | |||||
| Variable | |||||
| Age | Median | Mean | SD | Minimum | Maximum |
| 57 | 54 | 16.2 | 18 | 81 | |
| Gender | Male -24 | ||||
| Female-47 | |||||
| SOFA score at enrollment | Mean | Minimum | Maximum | ||
| 9 | 2 | 19 | |||
| Type of shock | Frequency | ||||
| Anemic | 1 | ||||
| Cardiogenic | 14 | ||||
| Distributive | 50 | ||||
| Hypovolemic | 3 | ||||
| Hypoxemic | 2 | ||||
| Neurogenic | 1 | ||||
| Fluid requirement | Median | Mean | SD | Minimum | Maximum |
| In ml | 2000 | 2076 | 998 | 500 | 4500 |
| Time point | Point biserial correlation (rpb) | Probability (p) value |
| 0 hour | 0.309 | 0.009 |
| 2 hours | 0.358 | 0.002 |
| 4 hours | 0.200 | 0.108 |
| 6 hours | 0.096 | 0.473 |
| 24 hours | 0.170 | 0.207 |
| Time Point | Point Biserial Correlation (Rpb) | Probability (P) Value |
| 0 hour | -0.206 | 0.121 |
| 2 hours | -0.206 | 0.011 |
| 4 hours | -0.350 | 0.010 |
| 6 hours | -0.380 | 0.007 |
| 24 hours | -0.398 | 0.007 |
| It was also observed that the pco2 gap at | ||
| 0h,2h,4h, 6hours had a statistically significant positive | ||
| correlation with lactate clearance.(Table 4) | ||
| Time point | Point biserial correlation (rpb) | Probability (p) value |
| 0 hour | 0.390 | 0.001 |
| 2 hours | 0.362 | 0.002 |
| 4 hours | 0.318 | 0.009 |
| 6 hours | 0.311 | 0.018 |
| 24 hours | 0.311 | 0.068 |
| IX. |
| Name: Dr. Sanjay Rao |
| Designation: Member Secretary |
| Contact No. 9538008940; |
| Email: [email protected] |
| PART II: Certificate of Consent |
| Print Name of Researcher/person taking the consent________________________ | |
| Signature of Researcher /person taking the consent__________________________ | |
| Date ___________________________ | Day/month/year |
| Print name of the impartial witness in capitals_______________________ | |
| Signature of impartial witness________________________ | |
| Date ___________________________ Day/month/year | |
| Deferred Consent for Research Participation | |
| Title of Project: | |