1.
Addressing Inadequacy in the Quality of Palliative Care of Multiple Myeloma in Nigeria using Actionable Frameworks Ogbonna Collins Nwabuko ? , Innocent Ijezie Chukwuonye ? , Kingsley Akaba ? & Martin Anazodo Nnoli ? Abstract-Background: Nigeria ranks within the top eleven countries of the world with the least average life expectancy from birth. As a result, the middle-elderly population is fast eroding. The worse hit in this scenario is the palliative care of the elderly who is neglected due to poor social determinants of health occasioned by leadership failure. Multiple myeloma is a common haematological malignancy in the middle-elderly target population that requires palliative care. Unfortunately, the quality of palliative care of people living with multiple myeloma in Nigeria is low partly due to grossly inadequate annual health budget.
Aim: To improve the quality of palliative care of multiple myeloma in Nigeria using actionable quality improvement frameworks.
Methodology: This was a systematic review and critical appraisal of palliative care of multiple myeloma in Nigeria and feasible frameworks that could improve quality of care. Three pairs of Medical Subject Headings (Multiple myeloma/Challenges in management in developing countries; Palliative care/Multiple myeloma; Palliative care/Quality assessment) were used as search strategy to demystify the research question. The issues of quality of palliative care of multiple myeloma were addressed from the perspectives of challenges of care of people living with multiple myeloma, methods of improving the quality of life of multiple myeloma patients in Nigeria, critical analysis of relevant quality areas, relevant structures and frameworks that could play key roles in mitigating healthcare needs of myeloma patients in Nigeria.
Results: The palliative care of multiple myeloma in Nigeria is grossly inadequate. The two major actionable quality improvement frameworks for palliative care of multiple myeloma are the Plan-Do-Study-Act-(PDSA) and Team-Based Outpatient Early Palliative Care (TO-EPC) frameworks. While PDSA model is more effective for quality improvement of health literacy, policy-making, health financing and diagnosis of multiple myeloma (preventive quality improvement), TO-EPC is more effective in the therapeutic intervention (curative quality improvement). Both are public health approaches of quality improvement in palliative care.
2. Introduction
ccording 2019 Central Intelligence Agency (CIA) report, Nigeria ranks 214 th in average life expectancy among the 224 member nations recognized by the United Nations with 54 years as the average number of years from birth. 1 This makes the country the 11 th worst nation to live on earth with respect to average life expectancy from birth and disease burden. In addition, the high-income gap between the ruling class and ordinary citizen creates inequality in distribution of resources including access to Medicare, hence making the nation a non-egalitarian society. [2][3] The middle-elderly population is therefore, gradually going into extinction in Nigeria as a result of negligence and poor social determinants of health, which if properly managed could improve their quality-adjusted life years and average life expectancy from birth. These nuances are the fall-out of leadership failure. Leadership failure is the major contributor of low (inadequate) quality of palliative care in Nigeria and this has heavily impacted on survival outcome of hematological malignancies including such as MM. 4 MM is a hematological malignancy due to monoclonal proliferation of long-lived plasma cells in the bone marrow leading to end-organ damages which include chronic bone pain, anaemia, orthopedic complications (i.e., pathological fracture), and chronic kidney failure (renal myeloma). 5 It is simply defined as cancer of the bone marrow which targets predominantly the middle-elderly population group (geriatric cancer). It is the second most common hematological malignancy of public health importance globally with a documented racial disparity for the blacks compared to their white counterparts. 6 MM is one of the hematological malignancies that requires adequate palliative care in order to improve the quality of life and survival intervals of the sufferers. Unfortunately, the quality of palliative care of people living with multiple myeloma in Nigeria is low due to grossly inadequate annual health budget. 7 Palliative Care is a holistic intervention that improves the quality of life of people facing lifethreatening illnesses through prevention and relief of their sufferings by means of risk identification, assessment and management of the conditions using approaches ranging from physical, socio-economic, psychological and legal in nature. 8 PC uses preventive and curative measures to improve QOL of the target population. The term ''holistic'' refers to a constellation of strategic approaches of intervention including physical, psychological, spiritual and social modes of attaining to the needs of the sufferers (i.e., PLMM) in order to improve their QOL. The term ''quality'' as used in this context connotes 'standard of care that is productive, effective, efficient and result-oriented' which is what differentiates level of PC in HICs from LICs and LMICs. The quality of PC is a predictive marker of activity and longevity (average life expectancy or survival outcome) of the sufferer. The higher the level of quality of PC, the higher the quality-adjusted life years and survival intervals. This disparity is evidenced by 5-years post-diagnosis survival interval of 7.6-15% for PLMM in Nigeria (a LMIC) 7,9 as against 50.7% in the United States of America, a HIC. 10 In all these, there is an interplay of leadership models, health economics, health governance and level (quality) of healthcare which invariably play key role in determining the QOL and life expectancy of PLMM in both transiting and developed countries. 11 These inequalities could be mitigated by implementation of the actionable PC models operable in HICs in transiting countries such as those found in sub-Saharan Africa.
This study aims to address the inequality in the QOPC of PLMM in Nigeria (a LMIC) using frameworks that can improve quality of PCMM.
3. II.
4. Materials & Methods
This was a hybridized version of review and critical appraisal of evidence-based research publications on PCMM in Nigeria, LICs, LMICs and HICs and feasible framework that could improve the QOPC in the region.
Three pairs of medical subject headings (namely MM and Challenges in management in Developing countries; Palliative care and MM; and Palliative care and Quality Assurance) were used as search strategies in Medline, PubMed, Scopus, African journal online, CINAHL, Cochrane library and Google search engine for problem identification, comparative analysis and outcome evaluation of research questions.
The issues of quality of PCMM were addressed from the perspectives of challenges of care of PLWMM, methods of improving the QOL of PLWMM in NGA, critical analysis of relevant quality areas, relevant structures and frameworks that could play key roles in mitigating healthcare needs of PLMM in NGA. This paper presented a synthesis of the reviewed articles and the suggested interventions (frameworks) that could scale-up the quality of PCMM in a developing country such as Nigeria.
5. III.
6. Results
There are 3 strategic challenges in managing MM in Nigeria and these are: The two arms of an ideal PC (namely the preventive and curative arms) are defective in Nigeria. These defects accounts for grossly inadequate and under-utilized PC in Nigeria and other LICs. The term ''inadequate'' as used in this context connotes poor-or low-quality care.
The identified pillars of preventive arm of PC that require quality improvement include:
7. Study
The observed impacts are recorded and data generated evaluated to test for quality improvement.
8. Act
Translating the outcome of data (result) into policy and useful frameworks for decision-making.
The identified pillar of curative PC that requires quality improvement is therapeutic intervention (early treatment).
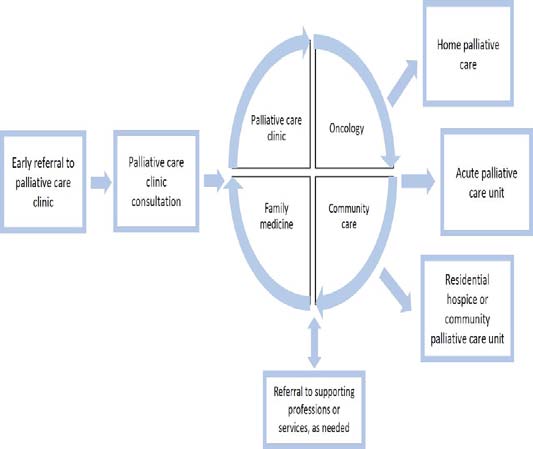
The Proposed Framework for Quality Improvement of Curative Arm of PCMM is the Teambased Early Palliative Care Conceptual Framework, TO-EPC (Figure 1). This is the current framework used in HIC where patients are referred palliative clinic by their attending physician. In TO-EPC, a longitudinal interdisciplinary collaborative care is given to patient by oncologist, family physician, community physician and other specialist depending on secondary problems associated with the disease. In addition, a follow-up care or visitation is extended to patient via the satellite home palliative care, acute palliative care unit and residential hospice or community palliative care unit. 12 It operates on 4 principles (patient-led, familycentredness, attentive and flexible) of care under 4 domains (namely copping and support, symptom control, decision-making and future planning). IV.
9. Discussion
This study has shown that an ideal PC uses preventive and curative measures to improve QOL of target population. The same principle is operative in the care of PLWMM. These two measures, also known as the arms of PC are mutually in-exclusive. Therefore, the quality improvement in level of PC must holistically address the two arms of PC to be effective. In order to improve PC, the World Health Organization (WHO) has proposed a model known as ''the WHO enhanced Public Health Approach Model for PC.'' This model operates on the premise that an effective level of PC must be founded on four pillars namely: appropriate policy, education, drug availability and strategic implementations. 13 This appears to be in keeping with the identified pillars of preventive arm of PC of MM which are grossly defective in Nigeria. There is a need to step-up the level of health literacy, policy-making processes, health financing and implementation strategies in the palliative care of people living with MM in Nigeria. 14 This may require application of other strategic leadership models for bringing about community and institutional change in the PCMM. 15 To achieve a high level of quality of PC in any health organization therefore requires swinging into action the essential components of care. Quality improvement which is the gateway for transformational healthcare delivery requires a sustainable effort of healthcare stakeholders and it does not work in isolation but in synergy in association with quality assurance and quality management. 16 The PSDA model and TO-EPC of MM are the strategic frameworks for achieve effective PC of PLWMM in Nigeria. While the PSDA model is more effective in the quality improvement of the diagnosis, education, funding, awareness creation and policy formulation, the TO-EPC takes care of definitive and supportive treatment of PLWMM. However, both frameworks in addition with the WHO enhanced PUBH approach model for palliative care are important in the comprehensive care of MM. These QI models (frameworks) should form integral part of the various components of comprehensive cancer care center in underserved setting including academic model providing access to healthcare. It is strongly believed that these actionable QI frameworks have the capacity to address the grossly inadequate quality care of MM in the middle-aged and geriatric populations which are gradually going into extinction in Nigeria and other sub-Saharan Africa regions.
However, actualization of actionable QI frameworks that could address the inadequate PCMM in Nigeria would be mirage without the key players coming together to embrace good governance, transformational leadership model and good health financing. The future healthcare leaders who must drive these operations must be visionary competent change agents who have the capacity and character to influence personal and institutional changes. 15 V.
10. Conclusion
The quality of PCMM in Nigeria is still grossly inadequate. There is a need to address the underlying causes which are primarily the defective preventive and curative arms of PC using actionable QI frameworks (namely the PDSA-and TO-EPC conceptual frameworks) and good health governance. This would require a healthcare-policy-driven government in order to be actualized. In all these, education, drug availability, funding, collaboration and strategic implementation of the policies are the tools to scale up the level of quality of PCMM, hence, improving survival outcome of PLWMM in Nigeria (SDGs. 1 & 4). This approach serves as the WHO enhanced public health approach model for improving PC. This intervention is a strategic leadership approach to achieve United Nations sustainable developmental goal (SDG) 1 and 4.
| 1. Education |
| 2. Policy-making |
| 3. Periodic Screening test/early detection (Diagnosis) |
| 4. Funding |
| The proposed public health Model for improving this arm of PC is the Plan-Do-Study-Act (PDSA) Model. |
| MODEL | DESCRIPTION | |||||
| Plan | Capacity building of Palliative | |||||
| Medicine via training and re-training | ||||||
| of | healthcare | professional | ||||
| workforce in palliative care using | ||||||
| 'catch them young' approach. | ||||||
| Advocacy to government and | ||||||
| donor agencies for support of | ||||||
| palliative care medicine through | ||||||
| funding or grants for procurement | ||||||
| of equipment and execution of | ||||||
| research projects in palliative care. | ||||||
| There is a need for health insurance | ||||||
| coverage for PLWMM. | ||||||
| Establishment | of | center | of | |||
| excellence for management of MM; | ||||||
| appropriation | of | adequate | ||||
| budgeting for MM care and | ||||||
| research, Public health awareness | ||||||
| campaign | on | MM | and | |||
| institutionalization of periodic MM | ||||||
| screening test policy in health | ||||||
| institutions. | ||||||
| Do | Strategic | implementation | and | |||
| monitoring | of | performance | ||||
| indicators of Preventive PC (i.e., | ||||||
| MM cancer registries, published list | ||||||
| of healthcare professionals who | ||||||
| received PC trainings over a given | ||||||
| period, the number of grants | ||||||
| received, lists of centers of | ||||||
| excellence for MM care as | ||||||
| evidenced by adherence to the | ||||||
| guidelines for PCMM as follow-up. | ||||||