1. Introduction
urgery of cranial base tumors has historically been one of the most complex and challenging disciplines in Neurosurgery. The difficult access and its intimate relationship with critical neurovascular structures make any surgical procedure a high-risk one. 1 Endoscopic approaches through natural corridors, Endoscopic Endonasal Approaches, allow minimizing the degree of cerebral invasiveness and improving tumor resection, with excellent results, visualization and dynamism. 2 With endoscopic approaches, there is evidence of a lower frequency of complications compared to traditional transcranial approaches, however, the CSF leak increases and can trigger other cascading complications such as meningitis and hydrocephalus. 3 In the following article, surgical cavity are classified depending on the contact with the intracranial hydrodynamic system and are related to the appearance of CSF fistula.
2. II.
3. Method
A descriptive observational study was performed in 550 patients operated for skull base tumors through Extended Endoscopic Endonasal Approaches, between 2010 and 2021 at the Ameijeiras Hospital. Surgical cavities were classified in relation to the intracranial hydrodynamic system into: type 0 (no contact with the hydrodynamic system), type 1 (subarachnoid cavity), type 2 (cisternal cavity), and type 3 (ventricular cavity) (Table 1) (Figure1). The statistical analysis was performed using the IBM® SPSS® version 23.0 program. To determine the relationship between postoperative CSF leak and the type of surgical cavity, it was performed the Pearson's chi-square test, with statistical significance p<0.05. In all cases, the same multilayer repair method was used at the cranial base, which included: fat, fascia lata, and Hadad-Basagasteguy nasoseptal flap. III.
4. Results
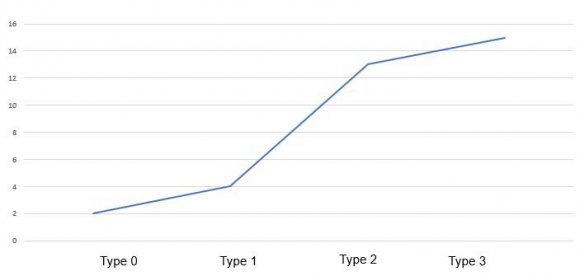
Table 2 shows the distribution of patients with CSF leak according to the type of surgical cavity. It can be seen that in type 0 the incidence of fistula was 0.7%, in type 1 it was 5%, while in type 2 it was 10.8% and in type 3 it was 18%. Figure 2 shows the increase in the CSF fistula as the type of surgical cavity increases.
5. Discussion
The intracranial CSF circulation system is considered a hydrodynamic system. In physics and physiology, liquids do not flow through a pressure or velocity gradient, but through an energy gradient, which explains why sometimes the liquid flows against pressure and velocity gradients, which constitutes the Bernoulli Effect, where the pressure and velocity are part of that energy. 4,5 The CSF circulates from central hydrodynamic points of high energy, for example the cerebral ventricles, to points of lower energy such as the cisternal and subarachnoid spaces, until it is finally absorbed into the venous system through the arachnoid villi (point of very low energy). 6 Intracranial Approaches, achieving radical surgical exeresis in most cases. However, the resulting surgical cavity may contact or be part of some point of the intracranial hydrodynamic system therefore receives the influences of the hydrodynamic laws. 1,2,6 Table 2 and Figure 2 show a significant increase in the CSF leak index as the type of surgical cavity increases, showing a higher incidence in types 2 and 3.
Before analyzing this behavior, it is important to consider some concepts: Surgical cavity: after a systematic review we did not find a precise concept, therefore, we define it as the anatomical space resulting from the surgical approach once the tumor exeresis has been performed. Hydrodynamic pressure: It is the force exerted by the fluid in motion on the walls of the cavity. This movement is defined by a vector field of velocities corresponding to the particles of the fluid and a scalar field of pressures, corresponding to the different points of the fluid in the cavity. 6,7 Flow rate or output: It is the amount of liquid that flows in a given time by a part of the hydrodynamic system, for example, the amount of liquid that flows through the surgical cavity in 1 second. 6 How do the laws of hydrodynamics influence surgical cavity?
First, if the surgical site is high-energy (the ventricular system), the hydrodynamic effect can overcome the resistance of the repair barrier, impede healing, and cause a CSF leak.
Second, the pressure of the CSF in motion increases in the surgical cavity above the pressure of the corresponding hydrodynamic point, that is, the pressure in the type 3 or ventricular surgical bed is going to be higher than the pressure in the Monro hole, this effect occurs because this surgical space will constitute a widening of the hydrodynamic system. [6][7][8] If we take an Extended Endoscopic Endonasal Approach to the Tubercle and Sphenoid Plane in the excision of a suprasellar tumor that reaches the third ventricle (Example: Craniopharyngioma) as an example, the surgical cavity that is created is type 3 (ventricular). That is, a cavity is created wide in ventricular contact that will suffer an increase in pressure higher than other normal ventricular points, for example, the hole of Monro. 6,7,9,10 For this demonstration, the law of fluid continuity must be applied; the amount of liquid that flows through Monro's foramen in a given time is the same as that which will flow through the surgical cavity, that is:
6. Monro flow = Surgical cavity flow
As the areas of the Monro foramen and the surgical cavity are different; to establish that equality then the liquid experiences an increase or decrease in flow velocity. For example, it increases its speed at the level of Monro's foramen and decreases at the level of the surgical cavity.
If we apply Bernoulli's theorem, which deals with the law of conservation of energy, then the sum of the kinetic, potential and pressure energies of a moving liquid at a given point is equal to that of any other point and mathematically is expressed:
P1+ KE1+ GPE1 = P2 + KE2 + GPE 2If we take into account that the Potential Energy is similar in a patient lying down at rest with a slight flexion of the head of 15 degrees, at point 1 (Monro's hole) and Point 2 (surgical cavity), then: P1+ KE1+ GPE1 = P2 + KE2 + GPE 2 P1+ KE1 = P2 + KE2, so using the formula for kinetic energy: P1+ ½ Density x V1 2 = P2 + ½ Density x V2 2 , since it is the same fluid, the density is the same. P1+ ½ Density x V12 = P2 + ½ Density x V22, then this equality depends on the variables pressure and speed of the liquid.
We had previously defined that the velocity of the liquid in the surgical cavity was lower than in the Monro Foramen, then: according to the laws of hydrodynamics to maintain equality in this Bernoulli equation, the pressure of the liquid in the surgical cavity is greater than the fluid pressure in the Monro foramen. These equations can be applied to both ventricular, cisternal and subarachnoid points. 6,7,11 This hydrodynamic increase in CSF pressure in the surgical cavity explains the higher frequency of CSF fistula appearance as the type of surgical cavity increases.
7. V.
8. Conclusions
According to the obtained results, it is essential to define the type of surgical cavity resulting from tumor exeresis and predict consequent hydrodynamic effects. The skull base repair strategy should have a broader concept that includes a multilayer repair barrier as a point of high resistance, as well as a decrease in hydrodynamic pressure in the surgical cavity through different methods: transient continuous spinal drainage (in Type 2) as well as permanent or temporary ventricular drainage (in Type 3). This would favor total healing and a decrease in the incidence of CSF leak.
| Surgical cavity | Description | Examples of tumors |
| Adenomas with intracapsular dissection, | ||
| Type 0 | No contact with the hydrodynamic system | chordomas of the clivus and malignant |
| sinonasal tumors without intracranial invasion | ||
| Type 1 | Subarachnoid (contact and subarachnoid dissection) | Adenomas with rupture of the arachnoid, meningiomas of the olfactory groove, small meningiomas of the sellar tubercle |
| Adenomas with extracapsular dissection, large | ||
| meningiomas of the sellar tubercle, cisternal | ||
| Type 2 | Cisternal (contact and cisternal dissection) | craniopharyngiomas, clivus and petroclival |
| meningiomas or cholesteatomas, chordomas | ||
| with intracranial invasion | ||
| Type 3 | Ventricular (contact and intraventricular dissection) | Craniopharyngiomas with ventricular invasion, giant adenomas with ventricular invasion, gliomas, and hypothalamic hamartomas |
| Source: Medical records |
| Type 0 | Type 1 | Type 2 | Type 3 | |||||||||
| CSF leak | Type0 | % | Type1 | Type of surgical cavity % Type2 | % | Type3 | % | N | Total | % | P | |
| No | 265 | 99,3 % | 76 | 95 % | 107 | 89,2% | 68 | 82 % | 516 | 93,8 % | ||
| Yes | 2 | 0,7 % | 4 | 5 % | 13 | 10,8 % | 15 | 18 % | 34 | 6,2 % | 0,000 | |
| Total | 267 | 100 % | 80 | 100 % | 120 | 100 % | 83 | 100 % | 550 | 100 % | ||