1. Introduction
orld Health Organisation (WHO) on January 30 2019, declared the outbreak of corona virus disease caused by the Severe Acute Respiratory Syndrome Corona Virus-2 (SARS-CoV-2) as international public health crisis. The first case of SARS-CoV-2 was reported in China in December 2019 which has expeditiously spread to the other countries and continents affecting highest number of population 1 . In a 3 months span of its first appearance in Wuhan, China, it was declared as Pandemic by WHO. In India about 3-10% patients are requiring intubation and 10-20% are requiring ICU admission 2,3 . The mortality rate was 49% 4 . The disease is characterised with dysregulated immune response with elevation in the levels of cytokines likeIL6, IL10, CXCL 10, lymphopenia and neutrophilia along with the systemic inflammation as seen by elevations in the levels of CRP, D-dimer, LDH, Ferritin. Lungs being the primary organ effected later leading to multi organ dysfunction 5 . To combat the disease several new molecular entities are being developed. On the basis of pathophysiology of the disease, it was thought that extra corporeal therapies specially designed to filter the cytokines can provide a hope in treating the critically ill COVID 19 patients and prevent organ failure and improve survival rate 6 . The same is demonstrated and supported by Ronco et al & Tay et al in their studies and clinical experience 7,8 . One such extracorporeal therapy designed to filter the cytokines was Cytosorb. Cytosorb was incorporated into the treatment guidelines in the early of the pandemic by several national medical societies. Use of cytosorb in COVID 19 patients with AKI (Acute Kidney Injury) stage 3 and are with Continuous Renal Replacement Therapy (CRRT) was first recommended by Italian Society of Nephrology 9 . USFDA also approved the usage of Cytosorb in critically ill COVID-19 patients on April 10, 2020 10 . In 2011, Cytosorb was originally approved by the European Union for treating the systemic hyperinflammation and refractory shock.
Cytosorb is an extracorporeal cytokine adsorption cartridge with blood compatible porous polymer beads used as an adsorptive material in this blood purification technology 11,12 . Through this highly porous polymer beads, Cytosorb can continuously remove molecules upto 50kD and help in treating certain conditions like hypercytokinemia and in conditions like severe inflammatory response 13 . Each adsorber cartridge can be used for 24 hours and then need to be replaced with another. The flow rate to be maintained is between150-700 ml/min and can be used as standalone approach in hemoperfusion technique or can be connected into ECMO or CRRT circuit 12 . This therapy aids in removal of cytokines from the blood stream through concentration gradient and the binding of molecules to the adsorptive polymer is size dependent making it a broad-spectrum purification technique 14 .
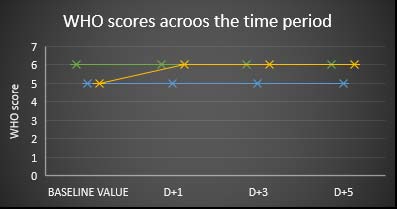
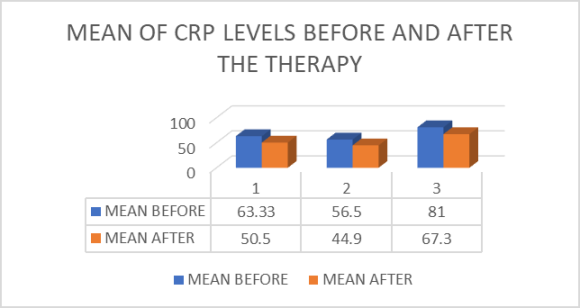
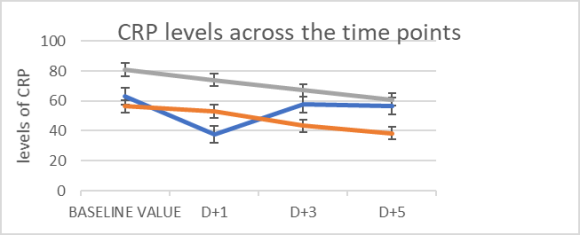
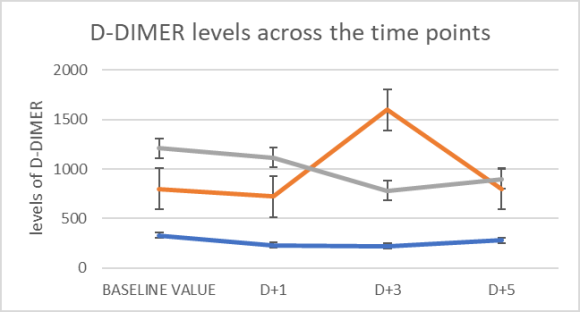
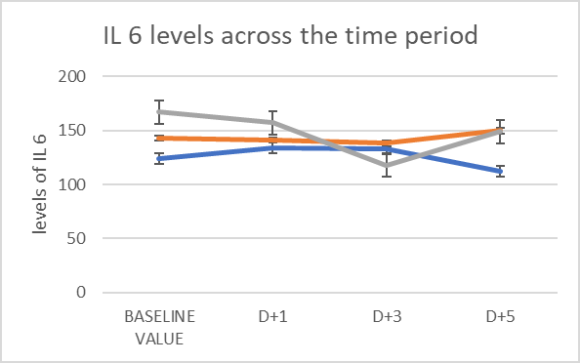
The current study is to demonstrate the effect of Cytosorb in severe COVID 19 patients in terms improvement according to 9-point ordinary scale developed by WHO 15 The outcome is measured in terms of reduction in the levels of inflammatory markers (C-Reactive Protein/CRP, D-dimer & IL6) before & after the therapy. The day of therapy is considered as D0 and the following post administration days as D+1, D+2, D+3, and so on. The levels of inflammatory markers and the scores according to the WHO ordinary scale on the D+1, D+3 and D+5 was observed and noted. The baseline value of each inflammatory marker is calculated by taking the average of the last 3 values before D0 which is considered as the mean value before the therapy. Similarly, taking the levels on the time points of our study (D+1, D+3 & D+5) another average value is calculated which is taken as the mean value post therapy. These 2 average values are compared to establish the role of Cytosorb in reducing the levels of inflammatory markers.
The trend of reduction in the values is statistically tested using annova single factor assay. In case of WHO ordinary scale score, the score on D0 and on 3 time points were taken directly (without calculating the average score value) to establish the cytosorb role in reducing the score value. The outcome of the patient on D+7viz, out off NIV or MV or Death (7-day survival rate) & duration of ICU stay is observed.
2. f) Procedure
After applying the inclusive and exclusive criteria individual patients given with respective number, P1, P2 & P3, in the sequence of their inclusion in the study.
All the patients received SoC which included Oxygen support to maintain SpO 2 ? 93%, Glucocorticoid; Dexamethasone (0.2-0.4 mg/kg/day), Remdesivir (200mg stat dose followed by 100mg once daily for 4 days to a cumulative dose of 600mg given in 5 days), i.v. Antibiotics at physician discretion (when a bacterial infection is suspected), prophylactic dose of low molecular weight heparin/ Unfractionated heparin with dose adjusted according to the body weight and renal function of the individual patient, along with symptomatic treatment that includes antitussives, antihistamines, antipyretics, etc.
In addition to the SoC, patients who are on NIV/ MV are randomly selected for treating with cytosorb after explaining the risks and benefits associated with the therapy. Cytosorb therapy is given as stand-alone treatment with blood pumps in hemoperfusion mode. The flow rate of the cytosorb was set to 150-200ml/min with unfractionated Heparin of 5000 IU as prophylaxis & to a duration of 8-12 hours depending on the clinical condition of the patient viz, elevated levels of markers, hemodynamics during the cytosorb, side effects to the therapy.
The baseline values (Mean before the therapy) of the inflammatory markers along with the score according to the WHO ordinary scale are compared with that of on D+1, D+3 and D+5 to observe for any reduction in the values.
3. h) Statistical Analysis
All the numerical data in the study, levels of inflammatory markers and score according to the WHO scale, are tested for statistically significant different across the time period using ANNOVA one-way methos in Microsoft Excel software. The p-value obtained by the test is used to confirm the assumed hypothesis, "levels of inflammatory markers/ score value according to the WHO ordinary scale are reduced upon cytosorb therapy". The p-value < 0.05 indicates the significant reduction in the values across the time period accepting the assumed hypothesis and vice-versa.
Non numerical data, population out off NIV/ MV/ ICU 7 days after the procedure, are calculated as % population with the respective outcome.
III.
4. Results
Our study included 3 male patients, Patient 1 or P1, Patient 2 or P2 & Patient 3 or P3, of age 61, 36 & 49 respectively with mean age 48.6 years. All the patients presented to the ICU in the study period received Cytosorb therapy after 5-7 days of admission in the ICU.
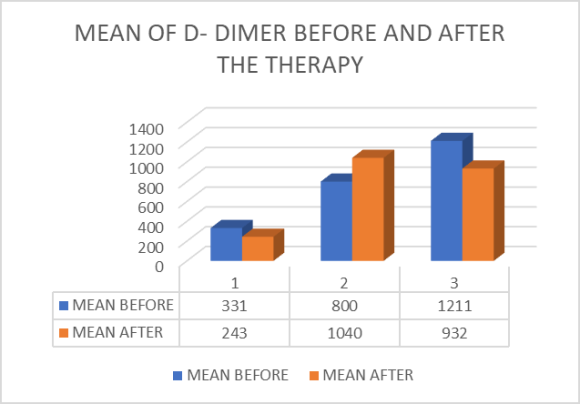
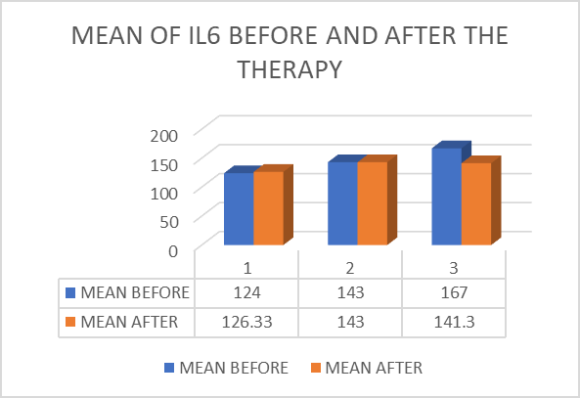
As detailed in the methodology and procedure sections, the baseline value of the levels of inflammatory markers are calculated and analyzed accordingly. The mean baseline value of CRP before therapy, was 63.3, 56.5 & 81 respectively for P1, P2 & P3. The mean average value of CRP after the therapy of P1, P2 & P3 was 50.5, 44.9 & 67.3 respectively. Figure 2 represents the mean levels of CRP before and after the therapy in all the 3 patients. The annova single factor assay done that resulted a p value of 0.60 reporting no statistically significant difference in the levels of CRP across the time period. Figure 3 shows the baseline levels of CRP of all the patients along with the levels on D+1, D+3 and D+5. The mean values of IL 6 levels before and after the therapy were almost similar with 124, 143& 167 and 126.33, 143& 141.3 before and after the therapy in P1, P2 & P3 respectively. Figure 6 represents the mean levels of IL6 before and after the therapy in all the 3 patients. Annova single factor assay done to test the statistically significant difference between the values reported 0.70 indicating no significant difference between the values across the time points. The 7-day outcome showed a complete mortality with 100% population (3 out of 3 patients) due to acute respiratory distress syndrome& AKI& cardiac arrest.
The table 2 provides the summary of our study at a glance.
5. Discussion
Despite the data relating to the use of Cytosorb usage in COVID is very limited, its application as a adjuvant therapy is been carried out at several educational institutions, being a new therapeutic approach in treating COVID 19 12 .
A case series of COVID 19 patients along with AKI treated with CRRT+ cytosorb published by Alharthy et al. reported reduction in the inflammatory biomarkers and 70 % population with favorable results surviving the condition and 30% died despite the therapeutic approach 16 . The first randomized, prospective pilot study conducted to study the effect of cytosorb in COVID 19 patients reported significant improvement in terms of Procalcitonin levels and vasopressor requirements. However, this study did not look for any improvement in terms of other inflammatory markers, ICU admission, Mechanical ventilation support, limitations of the study according to us 17 .
Another case series published by Mehtha et al., reported the use of Cytosorb after 72 hrs of ICU admission for 24 hrs reported a significant decrease in the levels of CRP and 100% survival rate 18 al, reported a case study of a 51 years old male COVID 19 patients who survived cytokine storm upon treating with Cytosorb and definite treatment 20 . Another case study conducted by Berlot et al, reported use of Cytosorb along with Tocilizumab reported a positive result in terms of extubation after 10 days of the therapy and radiological imaging suggestive of improvement in the lung fields 21 .
Rieder et al. studied the use of Cytosorb incorporated in tht ECMO circuit in comparison with the ECMO alone in treating severly ill COVID 19 patients. The study resulted in the higher reduction in the levels of IL6 in Cytosorb + ECMO group than in ECMO alone treated group 22 . However use of Cytosorb on the first day of ECMO initiation is not suggested and can be incorporated into the ECMO circuit after 24 hours of initiation according to the studies conducted by Alexander Supady MD 23 .
A comparative study conducted by Rampino T et al. reported the reduction of IL6, IL10, TNF ? and CRP in Cytosorb treated group in comparison to the control group. In test group, only 1 patient dies and 2 were intubated while that all of the patients in control group were intubated and died by the end of the study 24 .
VI.
6. Conclusion
A case cohort study conducted to establish the benefits of Cytosorb therapy in addition to the SoC in treating the severe COVID-19 illness in terms of reduction of inflammatory markers levels (CRP, D-DIMER, IL6), WHO score value along with the 7-day outcome of mortality or out off NIV/MV.
The results of our study didn't show any additional benefits of adding the CYTOSORB therapy to the existing SoC in improving the clinical outcome with no statistically significance in reducing the levels of inflammatory markers and even WHO score value. However, the 7-day outcome of our study reported 100% mortality, to confirm the complete ineffectiveness of the therapy in severe COVID 19 patients a study on large group population is encouraged.
| Patient state | Descriptor | Score | |
| Uninfected | No clinical or virological evidence of | 0 | |
| infection | |||
| Ambulatory | No limitation of activities | 1 | |
| Limitation of activities | 2 | ||
| Hospitalized mild disease | Hospitalized, no oxygen therapy | 3 | |
| Oxygen by mask or nasal prongs | 4 | ||
| Hospitalized severe disease | Non-invasive ventilation or high flow | 5 | |
| oxygen | |||
| Intubation or mechanical ventilation | 6 | ||
| Ventilation + additional organ | 7 | ||
| support-pressors, RRT, ECMO | |||
| Dead | Death | 8 | |
| II. | Methods | ||
| a) Aim | |||
| To measure the efficacy of CYTOSORB therapy | |||
| in reducing the levels of inflammatory markers in COVID | |||
| 19 patients. | |||
| b) Objectives | |||
| Primary Objective: To establish the beneficial role of | |||
| CYTOSORB in addition to the Standard of Care in | |||
| reducing the elevated levels of inflammatory markers in | |||
| severe covid 19 patients along with getting the patient | |||
| off the NIV/ MV/ICU. | |||
| Secondary Objective: To establish efficacy of Cytosorb | |||
| therapy in terms of improvement as per WHO scale | |||
| scoring & duration of ICU stay | |||
| c) Methodology | |||
| A case cohort study is conducted at Medisys | |||
| Hospitals, LB nagar, Hyderabad (city), Telangana | |||
| (State), India (Country) to establish the beneficial role of | |||
| cytosorb in addition to the SoC in patients with severe | |||
| COVID 19 illness and those who are on NIV/ MV in | |||
| reducing the levels of inflammatory markers and getting | |||
| the patients off NIV/ MV. | |||
| Study includes the patients admitted in ICU | |||
| from 01-05-2021 to 31-05-2021 with RTPCR proven | |||
| COVID 19 illness and HRCT severity ?14 and are on | |||
| NIV/ MV with age ? 35 years. | |||
| PARAMETER | PATIENT 1 OR P1 | PATIENT 2 OR P2 | PATIENT 3 OR P3 | STUDY GROUP | |
| AGE (YEARS) | 61 | 36 | 49 | 48.6 | |
| SEX | MALE | MALLE | MALE | ||
| D0 | 6 | 5 | 5 | ||
| D+1 | 6 | 5 | 6 | ||
| WHO SCALE | D+3 | 6 | 5 | 6 | |
| SCORE | D+5 | 6 | 5 | 6 | |
| D0 (mean before the | |||||
| therapy) | 63.33 | 56.5 | 81 | ||
| Mean after the therapy | 50.5 | 44.9 | 67.3 | ||
| CRP | P value | 0.6 | |||
| D0 (mean before) | 331 | 800 | 1211 | ||
| Mean after the therapy | 243 | 1040 | 932 | ||
| D-DIMER | P value | 0.95 | |||
| D0 (mean before) | 124 | 143 | 167 | ||
| Mean after the therapy | 126.33 | 143 | 141.3 | ||
| IL 6 | P value | 0.7 | |||
| 7 DAY OUTCOME | DEATH | DEATH | DEATH | ||
| V. | |||||
| Volume XXII Issue V Version I |
| D D D D ) F |
| ( |
| Medical Research |
| Global Journal of |
| © 2022 Global Journals |