1.
Abstract-Background: Mycobacterium Tuberculosis (TB) has been an important cause of mortality and morbidity all over the world but is specifically affecting developing countries like India where the disease is endemic. Inspite of being asymptomatic, female reproductive system is found to be very vulnerable to tubercular infections and by the time, Nontuberculous mycobacterial infections are also emerging and are found to cause serious genital infections in the females of child bearing age leading to infertility.
Objectives: Detection of Mycobacterial (MTB & NTM) infections among infertile females via different techniques like MRT-PCR, staining and their isolation by liquid media (using BACTEC 320).
Material and Methods: A total of 217 samples were processed involving the isolation of both (MTB and NTM). All three techniques were processed staining, culture and MRT-PCR to find the prevalence and efficacy of the techniques. For NTM and MTB differentiation SD MPT 64 card test was done.
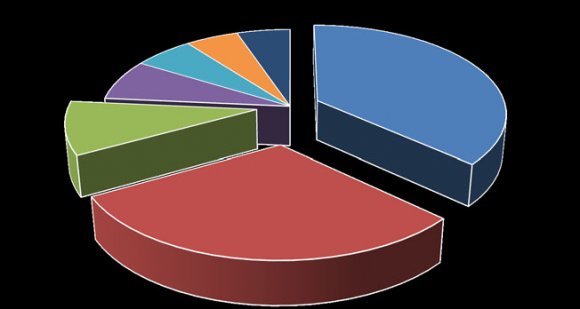
Results: Out of 217, TB suspected infertile female's maximum lies under the age group of 26-30 i.e. 34.10% (approximately 74 females) and the lowest were under the age group of 15-20 years i.e. 2.3% (5 females). There were total 24 NTM MRT-PCR positives and 29 MTB positives. So the total number of female patients who were positive by MRT-PCR technique was 53, whereas in liquid culture there were 23 positives (12 NTM & 11 MTB). 4 samples were found to be AFB smear positive by ZN staining.
2. Conclusion:
As Mycobacterium tuberculosis remains one of the leading causes of female infertility. According to a few studies, NTM's were found to be increasingly important pathogens causing male genital infections and infertility, but this study gave an insight that NTM's can even lead to female infertility and infections.
3. I. Introduction
uberculosis remains to be the foremost Killer disease for Indians among all other infectious diseases. It is anticipated that 5-13% of pulmonary tuberculosis develops genital involvement [1,2,3] .
This disease is a significant cause of infertility, menstrual irregularity, pregnancy loss, and in involvement with pregnancy, death rate to both the mother and child increases. HIV co-infection and resistant tuberculosis (MDR or XDR-TB) along with increased population immigration from developed to developing countries have now increased the tendency of the infection. Although new and finer diagnostic techniques for the detection of TB has been progressively available in the form of bacterial cultures and polymerase chain reaction (PCR) and other diagnostics, but still suspicion by clinician's continues to be the main tool for diagnosis of the disease.
Therefore, clinician's necessitate to be well trained to become "Tuberculosis Minded" [4] . Tuberculosis seems to be an important under diagnosed aspect in infertility. The possibility therefore exists that patients with genital tuberculosis can be classified as infertile.
Female Genital Tuberculosis (FGTB) which is commonly drawn in as a cause of infertility [5][6][7][8][9][10] , is often asymptomatic, rare disease with non-specific, mild clinical pictures and low indicator of clinical suspicion. There are no consistent confirmatory analytical procedures to ascertain the cause of infertility [8,9] . This is the most common form of extrapulmonary tuberculosis (TB), ranging about 27% (range, 14 to 41%) worldwide [10] . The prevalence of infertility in genital TB worldwide varies from 10-85% [8][9][10][11] ; it is endemic in India, with an incidence of 58% [12] and common is in the reproductive age group (15-45 years) [13] . In 80-90% cases, it affects women with menstrual irregularities and other particular significant symptoms accounting for about 27% of manifestations of FGTB [14] , even this rate can be higher among patients with tubal factor infertility (39-41%) [16] .
Female genital tuberculosis is secondary to tuberculosis infection elsewhere in the whole body. Haematogenous or lymphatic spread is the most wellknown method of spread. Infection may also spread from the adjacent and contagious intra abdominal sites. Patients may also have chief complaints like persistent lower abdominal or pelvic pain, or alterations in the menstrual cycles. Symptoms of tuberculosis toxaemia may not manifest and physical examination may be unexceptional [17][18][19] .
On the other hand, Nontuberculous mycobacteria (NTMB) are saprophytic organisms capable of causing chronic disease in humans [20][21][22][23][24][25][26] . The Nontuberculous Mycobacteria (NTM) refers to all the species in the family of Mycobacteria that may cause human disease, but do not cause tuberculosis (TB), in other words it is also known as MOTT (Mycobacteria other than tuberculosis). There are about more than 120 identified Mycobacterial species recognized today to cause disease in human [26][27][28][29][30] . The prevalence of NTMB disease is gradually increasing and has emerged in formerly unrecognized populations. The diagnoses of Nontuberculous infections are often complicated or unconvincing. Treatment is also difficult and often controversial, requiring prolonged, inadequately tolerated courses of therapy that are unlikely to produce eradication.
4. II. Material and Methods
The present study was done at Santosh Medical College and Hospital (Ghaziabad Delhi NCR) in collaboration with Oncquest Laboratories Pvt. Ltd. (03 factory road, Safdarjung Delhi) in which a total of 217 samples were processed using different techniques like AFB smear microscopy, AFB liquid culture via BACTEC 320 and MRT-PCR.
5. c) Exclusion Criteria
Eligible female patients not willing to participate and patients already on ATT were excluded for the study.
6. III. Methodology a) Specimen Collection
Clinical specimens for female genital infections including endometrial and ovarian tissues along with menstrual blood were taken. Specimens were transported to the laboratory as soon as possible after collection. In case of delay, the specimens were refrigerated to inhibit the growth of unwanted microorganisms.
7. b) Sample Processing
1. The sample was divided into three parts. First part was subjected for ZN staining, second was used for isolating the mycobacterial species by culturing and third was being used for molecular detection via MRT-PCR.
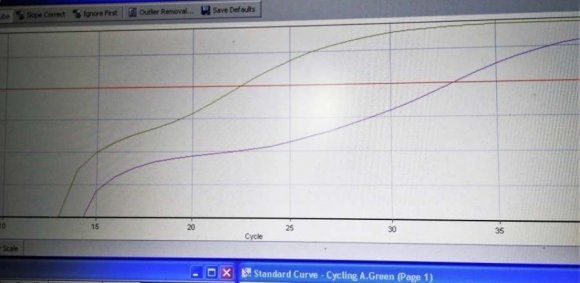
2. Samples were smeared with Ziehl-Neelsen (ZN) [31] staining to confirm Acid -fastness followed by Homogenization and decontamination by NAOH-NALC method. [31] 3. Isolation of Mycobacteria was carried out by culturing on liquid media by BACTEC 320 which works on the same principle of BACTEC 960 using MGIT tubes. Out of total 23 culture positives 11 were found to be MTB strains (i.e. 5.06%) and 12 were NTM strains (i.e. 5.52%). Out of total 53 PCR positives 29 were found to be MTB strains (i.e. 13.36%) and 24 were NTM strains (i.e. 11.05%). Out of total samples for liquid culture, Endometrial Biopsy / Tissue (195), 11 were MTB positive whereas 11 were found to be NTM strains. Menstrual Blood ( 17), only 1 NTM was detected. The other specimen didn't show any positivity for either of them. Out of total 217 samples, 10.59% were culture positive, 24.42% PCR positive and 1.84% was AFB smear positive by microscopy. Out of total 217 samples, 4 (1.84%) were observed positive for all the three techniques (Culture, AFB Smear and MRT-PCR), 3 (1.38%) were positive for Culture and AFB, 76 (35.02%) were detected Culture and PCR positives whereas PCR and AFB were only 4 (1.84%).
8. IV. Results
9. Out
10. Global Journal of
11. V. Discussion
Genitourinary tuberculosis is manifestation of extra pulmonary tuberculosis and claim 15% of all EPTB cases.
Fazal-ur-Rehman et al found AFB smear positive in 13 patients i.e. sensitivity of 51.5% from 50 symptomatic patients of genitourinary TB [32] .The study of Warren D et.al, also found Acid-fast staining as the most reliable test, with a sensitivity of 22% to 81% [33] . A study by A. Webster and D J Wright showed only 0.2% positive results on ZN staining [34] . Khaled G et al reported positive genital TB of 0.66% on ZN staining [35] . However, the results of our study were just contradicting showing 1.84% of AFB smear positive to P Pranali et al where all the samples were negative for Acid fast bacilli by ZN staining technique [36] .
S Rishi, in their study demonstrated that M960 system provided better isolation rate of Mycobacteria 98.06% from a variety of clinical samples than the LJ media 63.95% [14] . Various authors have reported similar findings ranging from 80 to 100% for M960 and from 59.7 to 87.2% for LJ [37][38][39] . According to the present study, isolation rate by M960 system was 10.58% in which 5.06% was MTB strains whereas 5.52% were NTM's. Besides higher isolation rate, even the time to detect Mycobacteria was shorter on M960 than on solid media, average being 9.66 days (2-39) with M960 and 28.81 days (7-48) with conventional solid media. Similar findings have been reported in the literature [40][41][42][43][44][45] .
PCR positive patients in the study of P Pranali et al were 8.69% which is very less as compared to the study by Negi S et al 74.4%, Hemal A K et al (80.95%), and Bhanu et al. 53.3% [46][47][48] .The study by Leonardo A. Sechi et al 6.3% showed low positivity as compared with the current study [49] which represented 24.41% for MRT-PCR positives constituting 13.36% MTB and 11.05% NTM's.
We compared the piece of various tests in different clinical samples for diagnosis of TB. PCR showed the uppermost sensitivity as compared to other tests as reported by others [50] . With the use of PCR test, we were able to detect M.tuberculosis in 97.87% smear negative samples which were positive by either of the culture methods. In a few samples, ZN smear examination and PCR results were positive but culture was negative; this could be due to the existence of nonviable mycobacteria in the samples [51] . The only drawback is that sometimes there may be false positive results by PCR test which could be due to the ability to detect very low number and even dead bacteria in a sample which can be present in a symptomatic individual [52] .
The purpose of this investigation was to evaluate the usefulness of multiplex polymerase chain reaction (MRT-PCR) in detecting uterine tuberculosis in women with infertility.
According to a prospective study, the mean age of the women was 29.75 ± 4.66 years. A total of 25.48% women were diagnosed as having uterine tuberculosis by in any case one of the diagnostic methods. Smear for acid fast bacilli in 2.53%, and liquid culture in 15.18% patients. The in-house MRT-PCR was positive in 85.44% women. Of these, 95.55% samples were positive for Mycobacterium tuberculosis, while 4.44% were positive by MRT-PCR for Nontuberculous mycobacterial DNA. So, the diagnosis of uterine tuberculosis, MRT-PCR was found to be the most efficient diagnostic tool compared to the other methods in that study [53] .
MRT-PCR test detected M.tuberculosis in less than one day, compared to average 24.03 days required for detection by liquid culture BACTEC 960 [54] .
Molecular diagnosis of tuberculosis by MRT-PCR has a great potential to improve the clinician's ability to diagnose tuberculosis. This will make certain early treatment to patients and put a stop to further transmission of disease.
12. VI. Conclusion
As Mycobacterium tuberculosis remains one of the leading causes of female infertility. According to a study, NTM's are found to be increasingly important pathogens causing male genital infections and infertility, but the present study gave an insight that NTM's can even lead to female infertility and infections. NTM's are often misdiagnosed as tuberculosis and are considered to be TB MDR, XDR or even TDR now a days due to overburden of the disease, so the patients were diagnosed accurately and treated accordingly at the earliest. This study helped to highlight the current

| Age Range | Total Patients | (MTB + NTM) Culture Positive | Percentage |
| 15-20 | 5 | 0 | 0% |
| 21-25 | 33 | 6 | 18.18% |
| 26-30 | 74 | 9 | 12.16% |
| 31-35 | 70 | 4 | 5.71% |
| 36-40 | 29 | 3 | 10.34% |
| 41-45 | 6 | 1 | 16.66% |
| Total | 217 | 23 | 10.59% |
| By MRT-PCR technique there were 53 positives | |||
| and NTM | (24 NTM & 29 MTB). The maximum numbers of females | ||
| AFB Culture Positives (n = 217) | were from the age group of 21-25 (30.30%) whereas the minimum number lied under the age group of 41- | ||
| MTB | NTM | 45(16.66%). | |
| Total | 11 | 12 | |
| Rate (%) | 5.06 % | 5.52% | |
| Age Range | Total Patients | (MTB + NTM) MRT-PCR Positive | Percentage |
| 15-20 | 5 | 1 | 20% |
| 21-25 | 33 | 10 | 30.30% |
| 26-30 | 74 | 21 | 28.37% |
| 31-35 | 70 | 12 | 17.14% |
| 36-40 | 29 | 8 | 27.58% |
| 41-45 | 6 | 1 | 16.66% |
| Total | 217 | 53 | 24.42% |
| those 217, Endometrial Biopsy / Tissue (195), 24 were | |||
| MTB positive whereas 18 were found to be NTM strains. | |||
| MRT-PCR Positives (n = 217) | Menstrual Blood (17), 4 MTB and 4 NTM were detected. POC (4), out of which there was no MTB strain but 2 | ||
| Total Rate (%) | MTB 29 13.36% | NTM 24 11.05% | NTMs were detected. Tubal Biopsy (1), which was MTB positive. |
| Total 217 cases of infertile TB suspected | |||
| females were observed via MRT-PCR technique. Out of | |||
| MRT-PCR |
| AFB Liquid Culture | |||||
| Type of Specimen | Total MTB Positive | MTB Negative | NTM Positive NTM Negative | ||
| Endometrial Biopsy / Tissue | 195 | 11 | 184 | 11 | 184 |
| Menstrual Blood | 17 | 0 | 17 | 1 | 16 |
| Product of Conception | 4 | 0 | 4 | 0 | 4 |
| Tubal Biopsy | 1 | 0 | 1 | 0 | 1 |
| Total | 217 | 11 | 206 | 12 | 205 |
| Culture Positives PCR Positive | AFB Smear Positive | ||
| Total Number (n = 217) | 23 | 53 | 4 |
| Positivity Rate | 10.59% | 24.42% | 1.84% |
| While depicting sample wise details and | positive. For Menstrual Blood (17), 8 (47.05%) were PCR | ||
| positivity rate of MRT-PCR, culture and microscopy | positive and 1 (5.88%) culture positive whereas no AFB | ||
| methods. Endometrial Biopsy / Tissue (195), 42 | smear positive. For POC (4), 2 (50%) were PCR positive | ||
| (21.53%) were PCR positive, 22 (11.28%) culture | and in case of Tubal Biopsy (1), 1 (100%) was detected | ||
| positive and 3 (1.5%) were found to be AFB smear | PCR positive. | ||
| Type of Specimen | Number of Clinical Samples | MRT-PCR Positive | MRT-PCR Positivity Rate | Culture Positive | Culture Positivity Rate | AFB Smear Microscopy Positive | Smear Positivity Rate |
| Endometrial Biopsy / | 195 | 42 | 21.53% | 22 | 11.28% | 3 | 1.5% |
| Tissue | |||||||
| Menstrual Blood | 17 | 8 | 47.05% | 1 | 5.88% | 0 | 0% |
| Product of Conception | 4 | 2 | 50% | 0 | 0% | 1 | 25% |
| Tubal Biopsy | 1 | 1 | 100% | 0 | 0% | 0 | 0% |
| Total | 217 | 53 | 24.42% | 23 | 10.59% | 4 | 1.84% |
| (NTM + MTB) Culture | ||||
| Culture + AFB Smear + MRT-PCR | Culture + AFB | Culture + MRT-PCR | MRT-PCR + AFB | |
| Total (n = 217) | 4 | 3 | 76 | 4 |
| Positivity Rate | 1.84% | 1.38% | 35.02% | 1.84% |