1. I. Introduction
epair of penoscrotal hypospadias is a true challenge to the surgeons. This is evidenced by the large number of procedures available for such repair. Treatment of penoscrotal hypospadias was performed by using two stage repairs to avoid the complications such as urethral fistula formation and strictures . [1] One stage repair has the advantages of minimizing operative trauma, allowing the use of unscarred skin with good vascularity and thus decreasing number of hospitalizations. [2] The utilization of a vascularized flap as neourethral tube from the ventral aspect of the prepuce has been popularized by Duckett in 1980. [3] When the urethral plate is adequate for utilization tubularized incised plate repair is preferable. [4] However this is not always the case especially in penoscrotal hypospadias where the surgeon finds that the urethral plate is poorly developed and unsuitable for utilization in repair after correction of chordae in many cases and preputial vascularized flap is a good alternative for repair. [5]Unfortunately, there are common problems that may occur with conventional onlay flap techniques including penile rotation and asymmetry of the penis since the vascular pedicle is brought around one side of the penis. [6] The dissection of the preputial vascularized flap from dorsal skin has been reported to affect the vascularity of the skin which may lead to gangrene and skin loss. Hence the idea of double faced tubularized repairs appeared where the tube is transferred to the ventral aspect of the penis with its skin coverings as one unit. [7]No current evidence suggests the superiority of one surgical technique over the other. Also is still no consensus among surgeons about whether a single stage or staged procedure is the proper treatment for penoscrotal hypospadias.
Here, we present our experience with the use of transverse ventral preputial tube for single-stage penoscrotal hypospadias repair in 80 patients, and
2. Global
3. II. Materials and Methods
This was a prospective, descriptive (comparative) study conducted at Alazhar University (Al Hussain Teaching Hospital) in the period from May 2012 to October 2015, to compare transverse preputial tube with double faced tubularized penoscrotal hypospadias repairs. All patients during study period who fulfilling the criteria were included which were 80 consecutive patients with penoscrotal hypospadias who underwent single-stage repair using the prepuce. Simple random sampling was done initially to select the first type of operation then followed by the other type. The patients were divided into two groups according to the used technique. The first group (Group I) comprised 40 patients who underwent hypospadias repair using transverse ventral island preputial tube. The second group (Group II) included 40 patients who underwent double faced preputial tube (with its skin cover) repair of hypospadias. All operations were done by the same surgeon.
The subjects were limited to the patients diagnosed as penoscrotal hypospadias with extensive chordae more than 30 degree after surgical degloving of the penis, who underwent one of the surgical techniques (Group one and two) and on regular follow-up. The exclusion criteria were: Patients with other types of hypospadias (distal and shaft), operation done by other surgeon or junior staff, penoscrotal hypospadias with straight or less than 30 degrees curved penis after degloving and if the patient disappeared or not on regular follow-up.
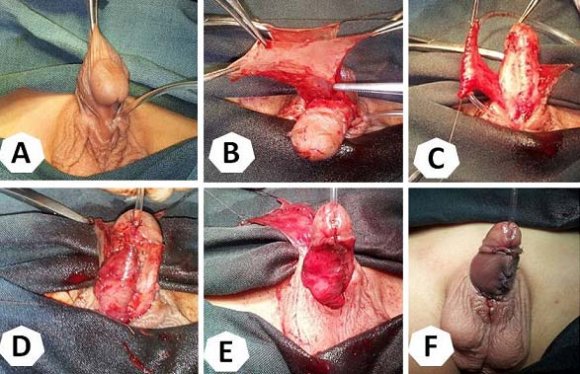
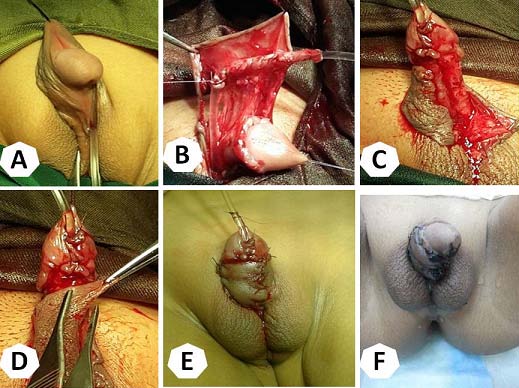
The surgical technique and patient follow-up: All procedures were performed under general anesthesia and loupe magnification after signing written informed consent by the parents. Surgical steps were started by circumferential coronal incision extending proximally by two vertical incisions 6-8 mm apart along the urethral plate up to the external urethral meatus and then going around the urethral meatus then degloving of the penis down to its root and proceeding to the correction of chordae assessed by artificial erection. All patients had extensive chordae more than 30 degree after complete penile degloving, excision of the fibrotic urethral plate and the dysplastic corpus spongiosum allow straightening of the penis. Glanular wings were fashioned and the length of ventral preputial flap needed was measured and outlined. In group I, the ventral preputial tube was fashioned to allow easy passage of 10 F. Nelaton's catheter, then the tube was completely designed with its pedicle then separated from preputial and dorsal skin of the penis and corpora by dissection plane developed between the flap and the dorsal skin, down to the base of the penis. The neourethral tube was rotated to the ventral surface of the penis from the left side and fixed to the corpora at its suture line. The stitches knots were kept outside the lumen of the neourethra (Figure 1). In patients of group II wide flap was required to make tabularization easier around a 8 F. Nelaton's catheter. Great care was taken to preserve the vascular pedicle of the flap. The tube was then transposed ventrally within its dorsal preputial skin and sutured to the corpora without any penile rotation using two interrupted suture (5/0 vicryl) (Figure 2). In both groups, the tube was sutured to proximal urethra using interrupted suture (6/0 vicryl), the original meatus was spatulated to make wide proximal anastomosis then the stent was put in the neourethra and sutured to the glans. Glanuloplasty was performed with two or more 5/0 vicryl sutures. The neomeatus is made oval. In group I, the rest of the preputial tissue was used for ventral penile coverings, while in group II the skin over the tube was sutured to remaining skin on both lateral sides by 5/0 vicryl suture. The stent was fixed to the glans by 4/0 vicryl suture, and then it was left into the diaper for two weeks. Post-operative antibiotics, analgesics, and antispasmodics are given. Dressing was removed after one week and the penis was kept moist with antibiotic ointment. The patients were discharged from the hospital after one or two days, to be followed in outpatient clinic. Follow up assessment was made after one month and 3 months by uroflowmetry. Statistical Analysis: Data was collected using a data collecting sheet (annexes). All statistical analyses were performed using SPSS (statistical package for social science) version 20.0; Chicago, IL, USA) with p-value?0.05 considered statistically significant. Our institutional ethical review board approved the study.
4. III. Results
This study was a prospective, descriptive study conducted at Alazhar University (Al Hussain Teaching Hospital) in the period from May 2012 to October 2015, 80 consecutive children (age 2 to 7 years with mean age of 3.2 years) underwent single-stage repair of penoscrotal hypospadias using preputial tube. All of them underwent urethral plate excision because it was rudimentary or unsuitable for utilization in repair. In Group I (40 children) hypospadias was corrected by transverse ventral island preputial tube. In Group II (40 children), double faced preputial tube (with its skin cover) repair was performed. The mean length of the neourethra in tubularized repairs was 34 mm. The follow-up ranged from 3 to 30 months (mean 14 months) (Table 2). 2). Complications developed in 10 cases (25%) in group I (1 glans dehiscence, 1 penile rotation, 2 urethral strictures and 6 fistulae), while 6 of group II (15%) who underwent double face tubularized repair developed complications (2 developed meatal stenosis, 2 urethral strictures, and 2 fistulae). The difference between the complication rates in both group was statistically significant (p= 0.001). The 8 children underwent fistula repair at a second operation and was successful in seven. The remaining one children with fistula (from group I) developed recurrence of the fistula and lost to follow up. The parents of the child with penile rotation refused the second operation. The child with glans dehiscence was treated successfully in a second repair. Meatal stenosis was managed by meatotomy in one and meatoplasty in another case. Two children with urethral strictures were treated successfully by anastomotic urethroplasty. Another two children with urethral strictures were lost to follow up. After management of the complications 76 of 80 children (95%) had good urine flow with satisfactory cosmetic result. Uroflow studies were performed in 76 children and showed normal curves and normal flow rates.
5. Global
6. IV. Discussion
The increasing number of procedures involved in hypospadias repair in the literature indicates that none of such procedures is ideal for all cases and the reconstructive technique should be tailored according to the type of hypospadias, the availability of the urethral plate, the state of circumcision, the state of penile skin and the degree of chordae. In the presence of good urethral plate, it should be utilized in the reconstruction since many studies found that preservation of urethral plate led to a high success rate repair with minimal complications. [8][9][10] However, in the presence of severe chordae, as in cases of penoscrotal hypospadias, the urethral plate may be rudimentary or unsuitable for utilization in the repair after excision of the chordae and need complete transection to allow proper penile straightening. The alternatives to the urethral plate include: the prepuce, penile skin or buccal mucosa. [11] Several surgical techniques have been designed for penoscrotal hypospadias repair as one stage or staged procedures. The staged technique was found simple and safe; however, the need for another hospital admission and anesthesia with additional costs limit the use of staged procedures. The one-stage repair is gaining more popularity by many surgeons recently because of its high success rate and comparable safety but still there are high complication rates that may necessitate another intervention. [12] The problem with penoscrotal hypospadias repair is the need for reconstruction of the deficient urethra and penile skin. The prepuce presents a good substitute for both the urethra and penile covering. Transverse preputial island tube urethroplasty has been reported to be more reliable than free tube operations, whether skin [13][14][15] or bladder mucosa. [16] In the present study, we performed a one-stage procedure using two established techniques to repair penoscrotal hypospadias in 80 cases with significant chordae more than 30 degrees categorized into two groups (40 cases each).The first group underwent transverse island tube procedure. The second group underwent double face repair of hypospadias. In fact, our aim was to try to answer the question: Does the dissection of the vascularized tube from dorsal preputial skin affect the outcome of the repair? Final outcome was satisfactory in 76 of 80 children (95%) (All cases except two urethral strictures, one fistula and one penile rotation) which is comparable to the results of Hayashi and coworkers (2001). [17] The overall complication rate in the present study was 20 % (16 of 80 children). The complication rate for group I was 25% and for group II 15% which was statistically significant (p= 0.001). This suggests that the dissection of the vascularized pedicle tube from dorsal preputial tissue may affect the vascularity and increase the complication rate and also shows that transferring the tube with its skin covering appears to achieve better results.
Duckett reported complication rates ranging from 7.5% to 18%. [18,19] Subsequent studies reported higher postoperative complications of one-stage Duckett urethroplasty, the rate varying from 8.6% to 56%. [20][21][22] The complication rate in our study was 20%, lies in that range. Another study with larger number of patients is needed to give more accurate success rates. Nuhogluand associates (2006) suggested that the complication rate can be lowered by proper skin care before surgery, tension free anastomosis, fine tissue handling, minimizing the use of electrocautery, the use of fine instruments with optimal magnification as well as the administration of prophylactic antibiotic as long as the catheters are in place. [23] In our study as well as in others urethrocutaneous fistula was the most common complication which can be minimized by avoiding tissue ischemia, closing the tube in two different layers invaginating the epithelium inward and covering the new urethra and the anastomosis site with adequate tissue before skin closure . [21] The additional coverage of the tunica vaginalis or scrotal dartos on the neourethral ventral side significantly decreased the risk of urethrocutaneous fistula, while also making phalloplasty safer and easier because of the additional coverage . [24] This technique has previously been applied in hypospadias surgery with excellent results. [25][26] Risk factors for complications include the following: Severity of hypospadias, the situation of the urethral plate, the patient (age, endocrine environment etc), the procedure I and surgeon experience [22]despite Zhonghua et al (2011) mentioned no significant difference in the rate of complication among either different age groups or different surgical times [27]. Hayashi et al (2001) attributed their low complication rate (7.7%) due to not only the two-layer closure of the neourethra but also the wrapping of the proximal anastomosing site with corpus spongiosum tissue. [17] There is much controversy whether to use suprapubic drainage or urethral catheterization for urinary diversion. Demirbilek and Atayurt (1997) found that the Duckett procedure without suprapubic diversion had two or three times higher complication rates than those with suprapubic diversion. [ 24] Chuang and Shieh (1995) reported no significant difference in the complication rate between the two diversions, but still preferred suprapubic diversion to an indwelling urethral catheter as disruption of the suture lines may occur during removal of the silicone Foley catheter. [25]In the current study, we did not employ suprapubic urinary diversion because it is thought to cause more bladder spasms than urethral catheterization. [15]We put a small caliber (6-8 Fr) Nelaton's catheter as a stent reaching the bladder fixed by the stay suture in the glans during the operation and we cut it to drain in a diaper. We have not experienced any complications related to this type of drainage.
Results of hypospadias repair can be analyzed using objective and subjective criteria. Objective criteria include functional evaluation of micturition. Uroflowmetry is difficult to interpret as its profile is often abnormal even if reconstruction is satisfactory. These flat profiles often reflect the poor compliance of the reconstructed urethra or the abnormal bladder behavior after hypospadias surgery. Subjective criteria are more difficult to define and evaluate in children, but certainly include cosmetic appearance, psychosocial adjustment, and body image. [26] The mean length of the reconstructed urethra in our study was 34 mm (range: 20 to 54 mm) which is similar to that previously reported (Hayashi et al. [17]-33.7 mm, Sorber et al. [27]-34.6 mm, Chuang and Shieh[28] -30 mm). It has been mentioned that patients with a neourethra less than 3 cm in length had significantly less complications than those with a neourethra longer than 3 cm [29]. We found that true, and 15 out of the 16 patients who developed complications had neourethra longer than 3 cm
The preputial pedicle tube has been reported to have cosmetic disadvantages such as ventral bulkiness from the pedicle and penile rotation (27) . [30]However, we had pleasing cosmetic results without bulking of the penile shaft. This is in agreement with the results of Hayashi et al. (17) . We had significant penile torsion in one child but his parents refused another corrective surgery. We used buttonhole technique in group I to bring dorsal skin to cover the ventral aspect of the penis to avoid penile torsion.
The first limitation in this study is the small number of cases in each group which makes statistical analysis inconclusive. This low number of cases is due to the fact that in many cases we find a satisfactory urethral plate that we can use for repair and such cases were excluded from the present series. The second limitation is the short-term follow up since it has been reported that more than 30% of posterior hypospadias patients develop complex long-term problems (28) . [31] However, since the purpose of the report is to evaluate the outcome of the preputial tube with and without dissection of the dorsal skin and skin necrosis occurs immediately after surgery, we believe that 14 months is a sufficient time to evaluate the outcome of the flap and skin.
7. V. Conclusion
Transverse preputial island tube and double face repair are good options to reconstruct proximal hypospadias after excision of chordee and urethral plate. Our results suggest that the dissection of the vascularized pedicled tube from dorsal preputial tissue may affect the vascularity and increase the complication rate and also shows that transferring the tube with its skin covering appears to achieve better results.
8. Global
| Year 2017 | |||||
| Volume XVII Issue I Version I | |||||
| D D D D ) | |||||
| ( | |||||
| Medical Research | |||||
| Global Journal of | Parameter | Mean (range) | Group I (n=40) | Group II (n=40) | P value |
| Mean age | 3.2 years (2-7) | 2.8 | 3.1 | 0.36 | |
| Mean length of neourethra | 34 mm (20 -54) | 32.7 mm (20 -49) | 33 mm(25 -54) | 0.51 | |
| Mean follow-up | 14 months (3to30) | 13.5(6-30) | 15.5(3-27) | 0.08 |
| Complications | Group I (n=40) | Group II (n=40) | P value |
| Urethrocutaneous fistula | 6 | 2 | 0.003 |
| Urethral stricture | 2 | 2 | 0.71 |
| Glanular dehiscence | 1 | 0 | 0.001 |
| Meatal stenosis | 0 | 2 | 0.004 |
| Penile rotation | 1 | 0 | _ |
| Total 16 (20%) | 10 (25%) | 6 (15 %) | 0.001 |