1.
In Vitro and In-Vivo Studies of Tolmetin Release From Natural Gel Base Extracted From Okra Seed (Abelmoschus Esculentus) That Cultivated In Egypt S. Abd El Rasoul ? , Sayed H. Auda ? & Alaa M. Nafady ? Abstract -Tolmetin is a non-steroidal anti-inflammatory drug commonly used for the treatment of rheumatoid arthritis, osteoarthritis, ankylosing spondylitis and periarticular disorders. In this work, we prepared and evaluated tolmetin release from mucilage extracted from Okra (Abelmoschus esculentus L) as a natural gel base. The in vitro release of tolmetin from natural gel base was studied using Franz diffusion cells with cellophane membrane placed between the donor and the receptor compartments. Possibility of solid state changes of Tolmetin with Okra seed mucilage (OSM) was studied using differential scanning calorimetery (DSC).
The anti-inflammatory activity of tolmetin from natural gel base was evaluated using the carrageenan induced rat paw edema method. The results revealed that the in-vitro release of tolmetin from OSM without any additives was about 75 % after 180 minutes. The drug was transformed from solid state to amorphous one indicating that there is a physical interaction between tolmetin and OSM in gel form. At the same time there is no interaction was observed in case of physical mixture. Finally, tolmetin from OSM gel base gave a significant antiinflammatory activity when compared with reference.
Keywords : Okra seed, mucilage, Natural Gel base, Tolmetin, In-vitro and In-vivo studies.
olmetin is a pyrrole, acetic acid derivative, nonsteroidal anti-inflammatory drug commonly used for the treatment of rheumatoid arthritis, osteoarthritis, ankylosing spondylitis and periarticular disorders. It inhibits cyclooxygenase activity with a reduction in the tissue production of prostaglandins. [1,2] A topical preparation of tolmetin would allow the administration of tolmetin in those patients who cannot tolerate the drug orally because of its adverse GIT effects. Chemical structure of Tolmetin is shown in figure 1.
It is well known that transdermal gels are more popular among all topical preparations due to ease of application and better percutaneous absorption than other semisolid dosage forms. Although many researches concerning the topical application of nonsteroidal anti-inflammatory drugs are existing in the literature, a few records are available regarding the release study of tolmetin from gel bases. [3] The synthetic polymers have certain disadvantages such as high cost, toxicity, environmental pollution during synthesis, side effects, less patient compliance. [4] At the same time, the advantages of natural plant based materials include low cost, natural origin, renewable source, environmental-friendly processing, local availability (especially in developing countries), better patient tolerance as well as public acceptance, from edible sources. [5] Mucilage is soluble hydrophilic polysaccharides and complex polymers of carbohydrate with branched structures. [6] It consists of polyuronides and galacturonides that chemically resemble the pectic compounds; upon hydrolysis, arabinose, galactose, glucose, mannose, xylose and various uronic acids are the most frequently observed components. [7] High concentration of hydroxyl groups in the polysaccharide has high water binding capacity. The complex polysaccharide is a part of dietary fibers which can absorb a large amount of water. It can dissolve and disperse, and can form viscous or gelatinous colloids. [8] Moreover, mucilage is, being used for their binding, thickening, stabilizing and humidifying properties in medicine. [9] Okra seed mucilage (OSM) is extracted from the seeds of Abelmoschus esculentus L. which is a common herbaceous annual occurring weed throughout Egypt.
Up to date, no research articles have dealt with formulation and evaluation of tolmetin from natural gel bases. The aim of this work was to prepare topical gel of tolmetin using natural gel base extracted from seeds of Abelmoschus esculentus. The prepared gel formulation was evaluated for in vitro release study and anti-inflammatory activity using the carrageenan induced rat paw edema method.
2. a) Materials
Tolmetin sodium salt was kindly provided by Minapharm Co. for pharmaceuticals (10th Ramadan, Cairo, Egypt). Standard cellophane membrane of molecular cut of rang = 1200, carrageenan, urethane (Sigma Chem. Co., USA). Male albino rats weighing 90-110 gm (Animal house, Assiut University, Assiut, Egypt). Okra plant (Abelmoschus esculentus L) was cultivated on the Experimental station, Department of Pharmacognosy, Faculty of Pharmacy, Al-Azhar University, Assiut, Egypt. A voucher specimen was kept on Department of Pharmacognosy, Faculty of Pharmacy, Al-Azhar University, Assiut, Egypt.
3. b) Extraction of Okra Mucilage
Seeds of Abelmoschus esculentus L. (250 g) was powdered and defatted by soxhlet extraction using petroleum ether as a solvent (1.5 L, five times) at temperature 60-70ºC this was repeatedly extracted with stirring using double distilled water and boiled for 5hrs till the complete mucilage was extracted and a slurry was formed. The slurry was cooled and kept in refrigerator overnight for settling protein and fibers so that the undisclosed portion was settled out. The mucilaginous solution was then filtered off and concentrated at 60oC on water bath until the volume reduced to one third of its original volume. Solution was cooled down to room temperature and was poured into thrice the volume of acetone by contentious stirring. The precipitate was washed repeatedly with acetone, absolute ethanol, diethyl ether and petroleum ether and dried at 50ºC under vacuum. The dried material was powdered, sieved and kept in desiccators. [10,11,12,13,14] c) Preparation of Tolmetin Free Acid Tolmetin free acid was prepared from its sodium salt by dissolving a weighed quantity of the salt in deionized water and precipitating out the free acid with an excess of concentrated hydrochloric acid. The precipitate was then washed with copious amounts of deionized water to remove unreacted hydrochloric acid. The tolmetin free acid was dried under vacuum at 40oC, to a constant weight. The free acid was obtained and then examined by melting point method, UV assay and infrared spectrum.
4. d) Preparation of Topical Gel
Gel was prepared by cold mechanical method. [15] Briefly, required quantity of OSM (20 % w/w) was weighed and slowly sprinkled on the surface of purified water for 2 hours. After which it was continuously stirred by mechanical stirrer till become completely soaked in water. Triethanolamine was added with continuous stirring to neutralize the gel. Finally tolmetin was added to the natural gel with continuous stirring until the drug completely dispersed in the gel base. The prepared gel base was packed in wide mouth screw capped glass container and kept in dark and cool place.
5. e) Drug Content Determination
Drug content of medicated gel was determined by dissolving accurately weighed (1gm) of gel in phosphate buffer of pH 5.5. After suitable dilution, absorbance was recorded at 324 nm. [16] f) In-Vitro Release Studies
The release of tolmetin from gel bases were studied using Franz diffusion cells with cellophane membrane placed between the donor and the receptor compartments. The membrane was soaked in sorensen's buffer overnight and then washed before use. A known amount (1 gm) of gel was added to the donor side and a known volume of Sorensen's buffer was added to the receptor side.
The receptor compartments were maintained at 32oC ± 0.5 throughout the experiment. At predetermined time intervals, a sample was removed from the receptor compartments and analyzed spectrophotometrically at 324 nm. The withdrawn samples were replaced immediately with an equal volume of fresh buffer. A control experiment was carried out using gel formulation without drug in order to ascertain any interference in the analysis by either the formulation or the membrane. g) Differential Scanning Calorimetry (DSC) Differential scanning calorimetry (DSC) was recorded using T.A. 501 Differential scanning calorimeter (Shimadzu Co., Japan). Samples of about 5 mg were accurately weighed and encapsulated into flatbottomed aluminum pans with crimped-on lids. The scanning speed of 10°C/min from 0°C to 200°C was used in presence of nitrogen at flow rate of 40 ml/min.
6. h) Preparation of Samples for DSC
The prepared plain and medicated gel base (5%) were dried in a desiccator for one week. After complete dryness, the co-precipitate was scratched, powdered and stored in capped amber-glass containers until use. For preparation of physical mixture, Samples having the same composition of the medicated gel base were prepared by simply mixing the triturated powdered drug and the tested mucilage powder in a porcelain mortar. The mixtures were then sieved, and the particles below 420 ?m were collected and stored in capped amber-glass containers until use. The samples were analyzed within one week after their preparation.
7. i) Anti-Inflammatory Effects of OSM Gel Containing
Tolmetin on Carrageenan-Induced Paw Edema
The experiment was conducted on male albino rates weighing 90-110 g divided into four groups each group consisting of 5 rats. Group 1: control, injected with carrageenan.Group 2: received plain natural gel base (without drug).Group 3: received medicated natural gel base (5%). Group 4: received commercial indomethacin synthetic gel base (Indotopic®, Ramida Pharmaceuticals Co. Cairo, Egypt). Paw edema was induced by subcutaneous injection of 0.1 ml of 1% carrageenan in physiological solution in the plantar surface of rat hind paw. [17] The rats were fasted for 16 hrs before the experiment with free access to water. The rats were anaesthetized by urethane (0.5 ml intraperitoneal) then 100 mg of each topical preparation were applied to the right hind of the rat. The thickness of rat hind was determined before and immediately after injection of carrageenan. Subsequent measurements for resulted edema were carried out at 0.5, 1, 2, 3, 4, 5 and 6 hrs after induction of edema. The anti-inflammatory effect was expressed as percentage inhibition of edema thickness compared with control according to the following equation; % inhibition of edema = (T o -T t ) / T o x 100. Where To is the edema thickness in control group, T t is the edema thickness in treated group. [18,19] a) In-Vitro Release Studies
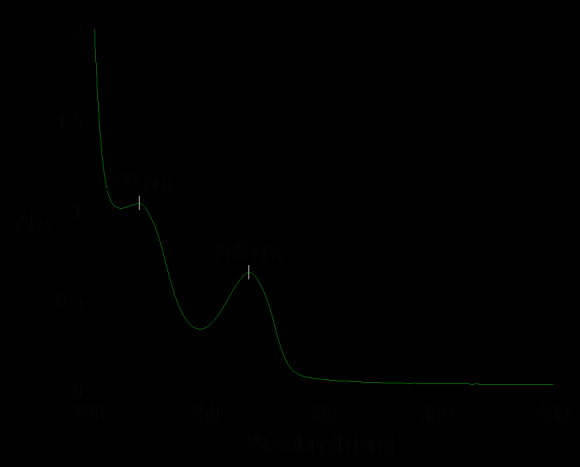
The in vitro release study of tolmetin from natural gel base was investigated in table (1) and graphically represented in figure (1). The results indicated that tolmetin released freely from natural gel base without any addition of penetration enhancers (about 75% after 3 hrs). This suggests that tolmetin free acid forms a hydrophobic complex with TEA, whereas, the OSM is hydrophilic. Hence, an increase in the aqueous content of the gels may have possibly increased the escape tendency of the relatively hydrophobic drug-TEA complex. [3] b) Differential Scanning Calorimetry DSC In order to shed a light on the possibility of solid state changes of tolmetin free acid, when dispersed in mucilage gel base extracted from Okra, DSC were performed on 5% medicated gel after complete dryness, its corresponding physical mixture and plain gel base after its dryness as well as the individual solid components. The DSC scan of untreated tolmetin free acid showed an endothermic peak (Figure 3A), at 160°C which is corresponding to tolmetin free acid melting point. DSC tracing of OSM in solid powdr and gel state exhibited a broad shallow peak at about 78°C (Figure 3B and C). Concerning the corresponding physical mixture (Figure 3D), characteristic endothermic peak of tolmetin were seen again at 158 °C but with low intensities. Upon scanning the DSC thermogram of tolmetin -OSM 5%, a complete disappearance of the drug fusion peaks (Figure 3E), suggesting a homogeneous dissolution of the drug in the polymer matrix. [20,21] Any abrupt or drastic change in the thermal behavior of rather the drug or excepient may indicate a possible drug-polymer interaction. [22] The endothermic peak of pure drug was observed at about 160° (figure 3A). However in the thermogram of the medicated gel there was no endothermic peak of the drug melting, suggesting the amorphous state of the drug in the microparticles. Pignatello et al. [23] studied the thermal behavior of Diflunisal-Eudragit RS100 and Eudragit RL100 coprecipitates (1:5). They found that a blend of the drug with polymers resulted in the disappearance of such a fusion peak, replaced by broad endothermic signals exhibiting a reduced melting endotherm and a lowering of the peak temperatures. These findings suggest that Diflunisal is able to dissolve in the polymer to a certain degree to form a solid solution.
8. c) Anti-Inflammatory Activity
The effect of topical formulation on the antiinflammatory activity of the drug was studied. The percent inhibition of carrageenan induced edema by 5% tolmetin in natural gel base and commercial indomethacin synthetic gel base is graphically represented in Fig. (4). the edema swelling was inhibited in all groups of rats either treated with the medicated natural gel base or in the group received topical indomethacin as standard drug. Three hours after carrageenan injection the percent edema inhibition was 43.30 and 48.70 % for medicated natural gel base and standard indomethacin respectively. The slight increased inhibition effect in case of reference group may be attributed to the incorporation of penetration enhancers. The group treated with natural gel base showed the highest inhibitory effect at 5 hrs after injection of carrageenan (percentage of edema inhibition was 58.59%). These results were nearly equal to inhibitory effect that obtained in group treated with commercial indomethacin gel as a reference (percentage of edema inhibition was 64.04 %). The results of this study show the possibility of commercial formulating tolmetin in natural gel topical formulation, which can produce a desirable local anti-inflammatory effect. It has been reported that topical application of NSAID containing formulations in animals can markedly attenuate inflammation pain and related behaviors. [24,25,26] Tolmetin gel is prepared by using Okra seed mucilage (OSM) as gel base. The prepared gels are evaluated for in vitro release, possibility of interaction between the drug and base and the anti-inflammatory activity. From the results, it has been observed that, the in-vitro release of tolmetin from OSM without any additives was 75 % after 180 minutes. The drug was transformed from solid state to amorphous one indicating that there is a physical interaction between tolmetin and OSM in gel form. At the same time there is no interaction was observed in case of physical mixture.
Tolmetin from OSM gel base gave a significant antiinflammatory activity when compared with reference. It can be concluded that tolmetin-natural mucilage gel for use as an anti-inflammatory dosage form is possible and may be applicable in future.