1.
burden is assumed to be due to iron deficiency (2). Many studies documented the adverse effects of maternal anemia, 12.8% and 3.7% of maternal mortality in Asia and Africa respectively is directly attribute-able to anemia (3). In Ethiopia; anemia is the severe problem affecting 62.7% of pregnant mothers and 52.3% nonpregnant women (4,5). For women, the consequences of anemia include reduced energy and capacity for work poor pregnancy and birth outcomes including premature delivery, low birth weight, and increased prenatal mortality, and increased risk of death during delivery and postpartum. It is estimated that as many as 20% of maternal deaths are caused by anemia and that anemia may be an associated cause in as many as 50% of maternal deaths worldwide (6).
As a public health measure, iron/ folic acid supplementation has been the recommended strategy for alleviating anemia in pregnant women. WHO recommended daily dose of 30-60 mg of elemental iron and 400 g (0.4 mg) Folic acid on daily bases throughout pregnancy (7).
To combat Iron deficiency anaemia, many developing countries including Ethiopia have interventions and programme during pregnancy. Provision of IFA supplement to all pregnant women free of charge is among the key interventions. The recommended dose by the Ministry of Health in Ethiopia is 60 mg/day for 90 days for iron and 400 g of folic acid daily (8,9). And, Although National Nutrition Strategy adopted key target of increasing the proportion of mothers who get IFA for more than 90 days during pregnancy and the post-partum period to 50% by 2015, there is discrepancy in the ANC coverage and the IFA intake level. The 2011 DHS documented IFA supplement of 17%. More importantly the IFA intake 90 or more tablets found to be 0.4% (18).
Gastrointestinal side effects, inadequate Supply of tablets, inadequate counselling, poor utilization of prenatal health-care services, lack of knowledge and patient fears about the tablets affect women's perception regarding tablet use in many countries (11)(12)(13)(14). Therefore, the findings of this study will give valuable information on compliances of IFA and its determinate factors for policy makers and service providers.
2. II.
3. Materials and Methods
A community based cross-sectional study using quantitative methods of data collection was conducted in Goba District, South East Ethiopia from March to May 2014.
Those postnatal mothers who give birth 6 months before the survey were included in the study. The sample size for this study was determined using a single population proportion formula estimation, with the assumptions of; an expected compliances to IFA 50%, a 95% confidence level, a 5% margin of error and a none response rate of 10%. The final calculated sample size was 422.
Goba district is divided into 2 urban and 24 rural kebeles (the smallest administrative unit in Ethiopia). From the district's 24 rural kebeles 4 were selected randomly and from the 2 urban kebeles 1 is selected randomly. In selected kebeles, preliminary survey was conducted to identify households with mothers who have child birth within 06 months prior to the study and sampling frame was developed. After the total sample size was allotted proportionally to the selected kebeles based on the total number of deliveries in the past 06 months, respondents were selected using systematic random sampling technique.
Data was collected using semi-structured, interviewer administered, pretested questionnaire after Obtaining informed consent. The completed questionnaire were given codes, checked for completeness and consistencies then entered into EPIinfo version 3.5.3 statistical software and then transferred to SPSS version 20 statistical package for further analysis. Data cleaning were performed to check for accuracy and consistencies, missed values and variables were also checked and corrected. The results were presented in the form of tables, figures, and text.
In this study, women were categorized as compliant to IFA supplement if she took 90 or more IFA tablets on daily base during her pregnancy (20).
Mothers Knowledge of anaemia was assessed using 20 questions. The questionnaire were composed of cause, health consequence, risk group and method of prevention in anaemia, Mothers who score mean value and above were considered as having good knowledge of anemia.
To assess mother's knowledge of IFA, 12 questions were employed, mothers who score mean value and above were considered as having good knowledge of IFA.
Both Bivariate and multivariate logistic regressions were used to identify factors associated with compliances to IFA. Odds ratio with 95% confidence interval was used to identify the presence and strength of association between variables.
Ethical clearance was obtained from the Institutional Ethical Review Board of Institute of Public Health, College of Medicine and Health Sciences, University of Gondar. Correspondingly written letters were offered from Bale Zone Health Department. Finally informed consent was obtained from each mother before the start of the interview.
4. III.
5. Results
6. a) Socio-demographic Characteristics
A total of 405 PNC mothers who give birth 6 months before data collection were included in the study with a response rate of 95.9%. The mean age of the respondents was 26.3 (±5.1) years. Around 35.6% of respondent were in age group of 21-25 years and about 28% were in age group of 36-40 years.
Majority of the women interviewed were married (98.1%) and rural dwellers (83.2%). About (32.1%) of the respondents were unable to read and write, (27.4%) can only read and write, (13%) had primary school level and (19.5%) had secondary school level. Regarding occupation majority of the respondents were house wives (72.6%) (Table1).
7. b) Pregnancy and Obstetric related characteristic of respondent
Around half of the respondents had less than three times ANC visit. Around eleven percent of the respondents had history of abortion and 3% had history of still birth. Among the respondents 21.7% started ANC while their pregnancy was less than 12 weeks of gestation, and 26.7% started after 24 weeks of gestation (Table2). c) Respondent's knowledge about anemia and benefit of IFA supplement Two third (62.5%) of respondents had good knowledge on cause, consequence, risk group, and method of prevention in anaemia, while 60.7% of the respondents had good knowledge on benefits of IFA. d) Service related characteristics About 78.9% were provided with health education and 21.1% were not provided health education on iron/folic acid supplements during their IFA collection. . Regarding dispensing of supplement; majority of the respondents (87%) collected 30 tablets whereas 12.8% were collected more than 30 tablets per visit (Table 4).
8. Volume XVII Issue I Version I
9. f) Factors Associated with Adherence
Bivariate analysis for compliances to IFA revealed that place of residence, educational status of mother, education level of the husband, mothers knowledge of anaemia, mothers knowledge on benefits of iron folic acid and receiving health education at the time of supplement collection have significant association with compliance to IFA at p value 0.02. Multivariable logistic regression was done to control potential confounders and educational status of mother, knowledge on anaemia, knowledge on benefits of iron folic acid and receiving health education at the time of supplement collection have significant association with compliances to IFA at p value (Table 5).
IV.
10. Discussion
This study revealed that only 18% of the studied subjects were compliant to IFA supplement.
The compliance rate of this study is lower than a study conducted in Kenya (24.5% (15), study conducted in Cambodia (47%) (16) and study conducted in India (35.5%) (17). This could be due to differences in socioeconomic status of the study population. But the finding of this study is higher than EDHS 2011 which was 0.4%. This could be because of the present study has been conducted among ANC follower and the time gap between the present study and EDHS 20011 (18).
Educational status of mother was important socio demographic factor which showed significant association. The compliance rate of IFA supplement was significantly increases with educational status of mother. Mothers who can't read and write were 91%, mothers who can read and write were 77% and mothers who had primary education were 76% less likely to adhere to IFA when compared with those who had above secondary education. This might be because, when women are educated, they might have accessible to information and advices from different sources about IFA and threats of anaemia.
Another important variable that showed a significant association is knowledge of cause, consequences, risk group and method of prevention in anemia. The rate of compliance to IFA was 59% times less likely among women with poor knowledge.
This finding was similar with the study done in Nepal which identifies high proportion of compliances among pregnant mothers with good knowledge (19). This could be due to reason that knowledge of pregnant women about anaemia related to causes, consequence and method of prevention affect their compliance of IFA.
In addition good level of knowledge about anaemia was a factor which could promote individuals in preventing iron deficiency anaemia and following recommendation.
It was found out that there was a significant association between respondent's knowledge on benefit of IFA and compliance to IFA. Women with poor knowledge on benefit of IFA were 62% times less likely to adhere than women's with good knowledge on benefit of IFA. This could be due to the fact that good levels of knowledge promote mothers to take the supplements based on the recommendation.
Receiving health education during prenatal visit was also an important predictor of compliance to iron foliate supplements. This study showed that mothers who were provided with health education at the time of receiving supplements have about 4.03 (AOR 4.03 (95% CI 1.4-11.5) times more likely to adhere to IFA supplement than those who were not provided. This could be due to the fact that health education at the time of supplement provide important information of IFA supplement V.
11. Conclusions
Compliance to IFA supplements was low among pregnant women attending ANC in the study communities. Increase awareness of the community about anemia and IFA supplement during pregnancy, improving educational status of women, providing alternative community based delivery mechanisms and sustainable supply of IFA is highly recommended.
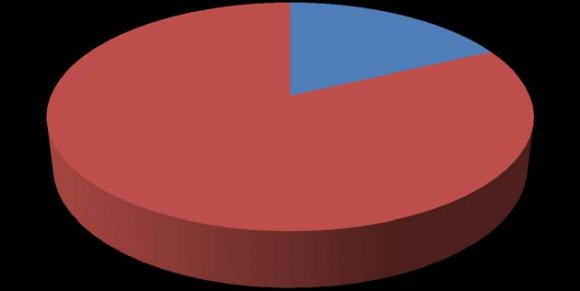
| 18% | |||||
| non compliance | |||||
| 82% | Year 2017 | ||||
| 25 | |||||
| Variable Age | 16-20 21-25 26-30 31-35 36-40 | Category | Frequency 51 144 132 50 28 | Percent 12.6 35.6 32.6 12.3 6.9 | Volume XVII Issue I Version I |
| single | 15 | 3.7 | D D D D ) L | ||
| Married | 370 | 91.3 | ( | ||
| Marital status Religion | Divorced widowed l Orthodox catholic Muslim protestant | 4 16 174 6 213 12 | 1.0 4.0 43.0 1.5 52.6 3.0 | Medical Research | |
| Residence Family size | rural Urban < 4 family 4-7 family >7 Family Can t read and write Can read and write | 337 68 71 253 81 122 117 | 83.2 16.8 17.5 62.5 20.0 30.1 28.9 | Global Journal of | |
| Educational level | Primary | 53 | 13.1 | ||
| secondary | 84 | 20.7 | |||
| Above secondary | 29 | 7.2 | |||
| House wife | 294 | 72.6 | |||
| Governmental employee | 41 | 10.1 | |||
| Occupation of mother | Private employee Daily laborer | 18 11 | 4.4 2.7 | ||
| Merchant | 24 | 5.9 | |||
| Farmer | 17 | 4.2 | |||
| © 2017 Global Journals Inc. (US) | |||||
| Ethiopia, 2014(n=405) |
| 2014 (n=405) | |||
| Variable | Frequency | Percent | |
| Knowledge on | Good knowledge | 253 | 62.5 |
| anaemia | Poor knowledge | 152 | 37.5 |
| Knowledge on | Good knowledge | 246 | 60.7 |
| benefits of IFA | Poor knowledge | 159 | 39.3 |
| Variable | Category | Frequency | Percent |
| Health education | Yes No | 319 86 | 78.8 21.2 |
| Waiting time | < 30 minute >30 minute | 354 51 | 87.4 12.6 |
| Problem faced | Yes No | 93 312 | 23 77 |
| Number of tab supplemented per | 30 tab | 353 | 87.2 |
| visit | >30 tab | 52 | 12.8 |
| Factors | Category | Compliance status of respondent | COR (95 % CI) | AOR (95 % CI) | |
| Compliance | Non-Compliance | ||||
| Place of | Rural | 54 | 283 | 0.49(0.26, 0.90) | 0.69(0.31, 1.5) |
| residence | Urban | 19 | 49 | 1 | 1 |
| Can t read and write | 9 | 113 | .20(0.7, 0.60) | ||
| Educational status of mother | Can read and write Primary education Secondary education | 20 8 28 | 97 45 56 | .54(.21, 1.39) 0.46(0.15-1.4) 1.31(0.51, 3.33) | 0.97(0.32, 2.8) |
| Above secondary | 8 | 21 | 1 | 1 | |
| Can t read and write | 10 | 70 | 0.38(0.13, 1.04) | 1.31(0.34, 4.9) | |
| Educational status of husband | Can read and write Primary education Secondary education Above secondary | 16 13 25 9 | 100 46 92 24 | 0.42(0.16, 1.08) 0.75(0.28, 2.75) 0.72(0.29, 1.75) 1 | 1.30(0.37, 4.4) 3.3(0.90, 12.3) 0.85(0.30, 2.3) 1 |
| History of | Yes | 15 | 32 | 2.4(1.23, 4.7) | |
| abortion | No | 58 | 300 | 1 | 1 |
| Knowledge on | Good | 58 | 195 | 1 | 1 |
| anemia | Poor | 137 | 15 | 0.36(0.20, 0.67) | |
| Knowledge on | Good | 56 | 190 | 1 | 1 |
| benefits of iron folic acid | Poor | 17 | 142 | 0.40(0.22, 0.72) | |
| Health education | Yes | 68 | 251 | 4.3(1.71, 11.2) | |
| at the time of | |||||
| supplement collection | No | 5 | 81 | 1 | 1 |