1. I. Introduction
he entrance of small quantity of fetal red cells into the maternal circulation during or before delivery is commonplace in all pregnancies. However, a blood loss of more than half of fetal blood volume is rare and can potentially lead to severe neonatal anemia and death up to 0.04% of all births (1,2) . Usually the cause is idiopathic and happens in low-risk late pregnancies (3,4) .
Fetomaternal hemorrhage can take place early in pregnancy because of disorders of the placental circulation. About half of mothers have detectable fetal red cells in their circulation of a very small amount (5) . Volumes in the range of 10-150 ml can be associated with FMH (6,7) . Amount exceeding 150 ml happens in a very small number of pregnancies and the severity of FMH can be assessed by the quantity of fetal cells in the maternal circulation (8) .
Known incipitating factors of fetomaternal hemorrhage include placental abruption, vasa previa, amniocentesis, chorionic villous sampling, external cephalic version, choriocarcinoma (8) . In addition, Rhesus alloimmunization has been identified as a possible cause of fetomaternal hemorrhage (9) . In that case, Rhesus + fetal cells sensitize Rhesus -maternal cells resulting in alloantibody production. This in turn can lead to hemolytic disease of the newborn (HDN) (10) . The rates of such complications are very low due to Rhesus screening and immunoprophylaxis. However in up to 82% of cases of fetomaternal hemorrhage no causative agent can be identified (11) .
There are specialised tests that can confirm the presence of fetomaternal bleeding. The rosette screen can detect small quantities of fetal blood in the maternal circulation and the Kleihauer-Betke test remains the method of choice that can confirm the diagnosis and quantify the amount of fetal cells (12,13,14) . Moreover flowcytometry can also assist in the detection of fetal cells but has no increased sensitivity in comparison to KB (15) . In early pregnancy a sensitive marker supporting FMH is increased alfa fetoprotein (AFP). Later on, the diagnosis of FMH can be supported by both increased AFP and a positive Kleihauer-Betke test (16) .
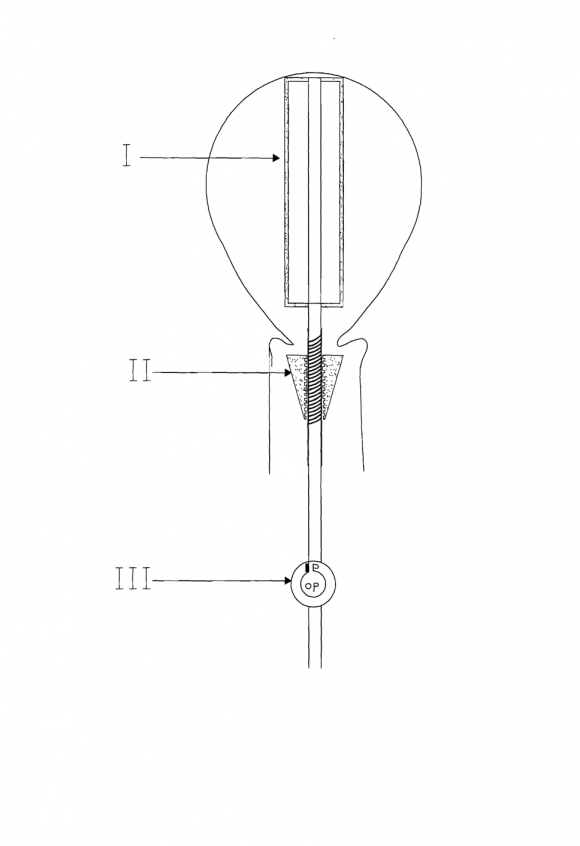
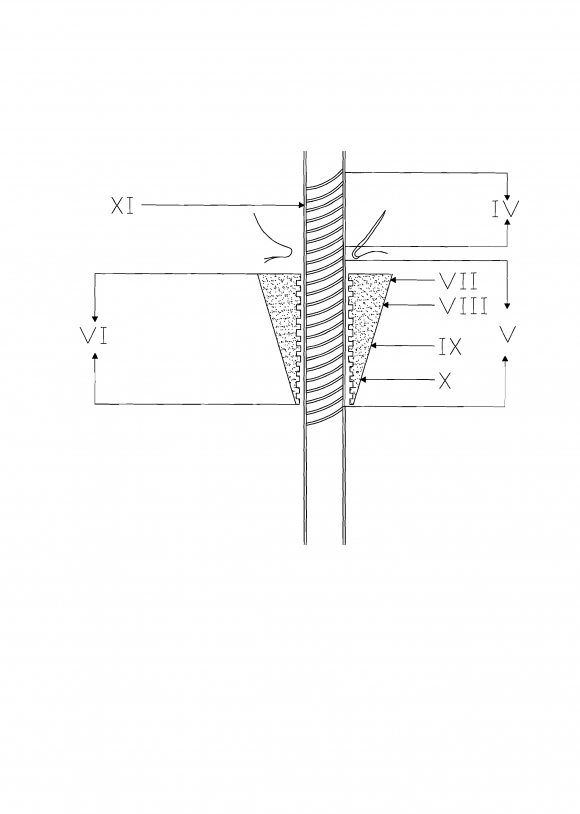
The clinical picture can vary greatly. Fetomaternal hemorrhage can manifest as decreased fetal movements without an association with abdominal injury, pain or bleeding (17) . Abnormal CTG tracings can be discovered accidentally with decreased variability, variable or late decelerations (18,19) . Ultrasound findings include intraventricular hemorrhage, pleural and pericardial effusion and ascites (20,21) (Fig. 1
2. , 2 & 3).
The child can suffer from severe respiratory depression and hepatomegaly or subcutaneous edema as a consequence of congestive heart failure (22,23,24) . Additionally, possible complications include neurological sequelae, for example spastic cerebral palsy and stillbirth (25,26) . The laboratory results at delivery may include increased reticulocyte number suggestive of chronic blood loss, deranged coagulation and liver enzymes and hematuria (27) (Table 1). The management of fetomaternal hemorrhage can also be complicated. In early pregnancy intrauterine transfusion may be attempted to correct the anemia but in cases of continuous bleeding, repeat transfusions or delivery may be indicated (28) .
Although massive fetomaternal hemorrhage is a rare condition, it is possibly under diagnosed because of the lack of clinical suspicion (10) . With fetomaternal hemorrhage being an etiology of serious fetal morbidity and mortality, further research is essential for avoiding significant complications.
| Year 2018 |
| 1 |