1. Spontaneous Vertebral Artery Dissection Presenting with Crescendo TIAs and Headache
Dr. Nosakhare I Idehen ? & Dr. Mohammed Awad ? Summary-We present the case of a man in his thirties who had attended the emergency department with complaint of a distressing headache and associated intermittent facial droop with occasional slurred speech. The patient's symptoms were bizarre in their nature as they were random, not sustained and he had long intervals when he was asymptomatic and was his normal self. During the course of admission his symptoms evolved resulting in neurological deficits which were more sustained, prompting the need for further imaging beyond the initial plain CT brain which showed no abnormality.
This led to the diagnosis of vertebral artery dissection (VAD) complicated with an ischaemic stroke in the posterior inferior cerebellar artery distribution (PICA) on MRI/MRA. Dual anti-platelet treatment was commenced with the patient attaining gradual symptomatic improvement prior to discharge. He has reported some degree of neurological sequelae which he described as intermittent poor coordination on follow up visit in clinic after discharge.
2. I. Background
pontaneous vertebral artery dissection has an estimated incidence of 1-1.5 per 100,000 classing it as a rare condition. [1] The wide symptom spectrum that mimics other seemingly more common pathologies can mean it is easily missed or leads to wrong diagnosis.
As a major cause of stroke in young adults with patients presenting at times with symptoms that may not manifest as full blown neurological deficit in the first instance, we have considered it important to report on this case to increase awareness on this pathology and improve understanding on how patients may present and lay emphasis on the need to consider vertebral artery dissection in the differentials for relevant patients, cause prompt diagnosis and early treatment is important for good prognosis and recovery. Making a diagnosis of vertebral artery dissection can prove to be difficult as the presenting symptoms overlap with other pathologies. It can be challenging to convince overworked, under resourced radiologists of the importance of conducting an urgent MRI. With greater familiarity of the possible clinical features this could be eased.
There has been an increase in recent decades in the number of cases reported and the accessibility to better diagnostic imaging modalities has been attributed as one of the factors rather than an actual rise in incidence. [2] With clinicians having higher index of suspicion and utilising this improved diagnostic techniques this numbers may well continue to rise.
With absence of risk factors and atypical presentation, diagnosing VAD and posterior circulation events in an acute sitting can be challenging as it heavily reliant on imaging services, thus admitting patients who have symptoms suggestive of VAD for further imaging in normal hours if the resources for urgent imaging are unavailable, would be a better outcome and improve patient experience than dismissing them just because they don't fit any clear clinical pattern.
3. II. Case Presentation
A 36-years old gentleman self-presented to the emergency department with complaints of sudden onset, intermittent, severe headache, shooting right sided facial pain with associated right sided weakness, slurred speech, dizziness and leaning to the right side when walking. The patient also described mild neck stiffness, mild photophobia, and jaw claudication. There was no history of trauma nor past medical history of concern.
The characteristic of note was the sporadic nature of this symptoms as they seemed to occur only when patient was being assessed, with well-spaced symptom free intervals. His vital signs recorded were all within the reference limits. Clinical examination in the emergency department did not yield any useful information as his symptoms were not reproducible besides his intermittent calling out in pain, this was not convincing for emergent imaging and on account of patient's distress and poorly controlled symptoms he was referred to the medical team for review and further management. He was admitted under the neurology team and on assessment the following day symptoms had evolved and there was demonstrable neurological deficit.
On examination there was altered sensation in the distribution of the 5 th cranial nerve on the right side of the face, dysmetria and dysdiadochokinesia in the right upper limb. There was also some impairment of coordination of the right lower limb. There were no power, tone or reflex deficits observed. His headaches had resolved to burning episodic facial pain by this time.
4. S
This was approximately 32 hours from initial presentation with earlier symptoms which in retrospect were caused by the dissecting vertebral artery and transient ischemic attacks involving the inferior cerebellar peduncle including parts of the area of supply of the right posterior inferior cerebellar artery (PICA).
5. III. Investigations
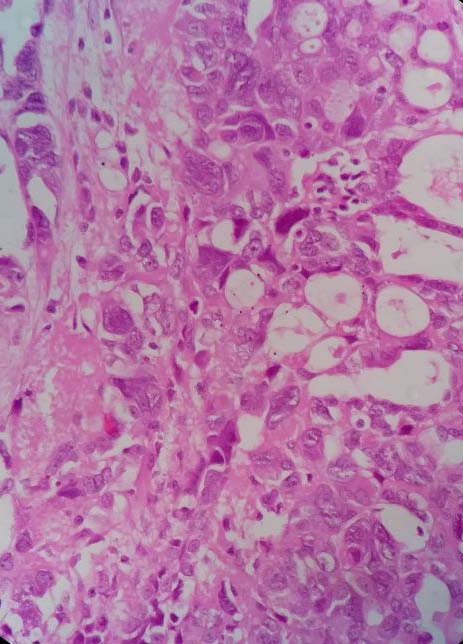
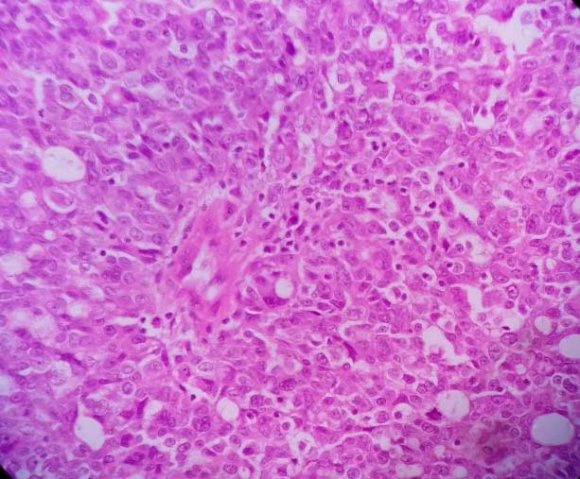
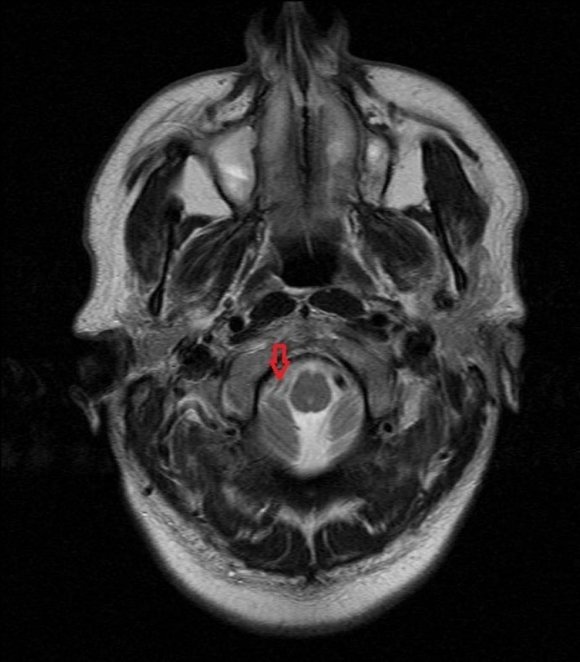
CT-brain done on the day of admission showed no abnormalities and MRI with contrast conducted the following day showed right vertebral artery dissection with small infarct involving the right inferior cerebellar peduncle and part of the cervicomedullary junction which suggested involvement of part of the right posterior inferior cerebellar artery.
Other routine investigations conducted include FBC, U & E, Coagulation profile, ESR and CRP were also all within reference limits as well as a normal ECG tracing.
MRI/MRA Images shown below:
6. IV. Differential Diagnosis
The none specific and sporadic nature of the symptoms gave rise to a broad list of differentials listed below: Trigeminal neuralgia Migraines Internal carotid artery dissection Sub-arachnoid haemorrhage Cluster headaches Focal seizure disorder (patient appeared to have myoclonic jerks on some occasions) Conversion disorder
7. V. Treatment
With diagnosis now confirmed as vertebral artery dissection complicated with a stroke patient was commenced on Aspirin and Clopidogrel with Dalteparin included only during admission period. He was treated with regular analgesia for pain control.
There was progressive improvement of symptoms with treatment. After review by the physiotherapy team on the 8 th day of admission he was discharged home to continue with dual anti-platelets and planned reviews in the outpatient clinic
8. VI. Outcome and Follow-up
On review at the follow up cerebrovascular clinic after discharge he reported resolution of symptoms to a large extent and described mild unsteadiness on his right side, this is said to occur intermittently.
9. VII. Discussion
Vertebral artery dissection (VAD) is one of the most common causes of stroke in young people. It is broadly classified under cervical artery dissections which include Internal carotid artery dissection (ICAD) and Vertebral artery dissection. ICAD occurs 5 times more frequently than VAD and together they account for 20% of stroke in the young. [3] The pathophysiology of VAD is not well understood, multiple factors are postulated to contribute to its occurrence which include environmental risk factors (cervical trauma, recent infection, sudden movement of the head, and migraine) and protective factors (hypercholesterolemia, overweight) have been described. [4] Genetic predisposition has also been documented to be an intrinsic factor in the development of a VAD. [2] Other contributory factors mentioned in case reports on VAD include high blood pressure surges [5] and neck manipulation. [6] However fewer cases were deemed to be spontaneous [7,8] with some authors suggesting there may have been minor or trivial injury around the neck preceding spontaneous cases.
The diagnosis of traumatic vertebral artery dissection is reserved for those with significant trauma including road traffic accidents or penetrating neck injuries.
The dissection could be intracranial or could be located outside the cranial vault. Despite their similarity in size the extracranial portion of the vertebral artery is more prone to dissection than the intracranial portion. [9] Dissection occurs when blood accumulates in the wall of the blood vessel. A tear in the tunica intima (the inner layer), allows blood to enter the tunica media.
The reduced rate in blood flow and endothelial injury encourages thrombus formation, with the inevitable emboli causing brain stem and cerebellar infarctions, as was the case with the patient in this report. Dissections involving the tunica adventitia could form a pseudo aneurysm, which can rupture causing a sub-arachnoid haemorrhage. [3] Headache, vertigo, vomiting and unilateral extremity weakness are well recognized presentations of VAD and cerebrovascular accidents. [10,11] The clinical versatility of this pathology includes symptoms which besides headache and neck pain (most common symptoms) could include postural imbalance, facial numbness, dysphagia, dysphonia, unilateral facial paraesthesia as well as unilateral deafness. [12] Since headache and the above listed symptoms could precede ischemic symptoms to the brain by minutes or days, these red flags could be considered as warning signs to provide a chance for diagnosis before ischemia sets in. Putting these into account patients who present with unexplained or unusual neurological symptoms that could be suspicious for vertebral artery dissection would benefit from detailed and thorough neurological examination as well as appropriate imaging studies.
Current evidence shows no change in incidence but rather more accurate diagnosis with the advancement in imaging techniques and increased availability of the study modalities required in reaching a conclusion. [2] A review of the literature from 2008 till 2018 shows 44 documented cases on MEDLINE (with 5 cases from the UK) of various presentations of vertebral artery dissection and in not a few of the cases diagnosis was reached when these patients were admitted for other reasons, as VAD was not considered a likely priority for investigation on the list of differentials and it was not uncommon for the patients to develop further neurological deficits while on admission, which prompted more detailed imaging studies.
The American Heart Association (AHA), American Stroke Association (ASA), and the International Headache Society all recommend MRI/MRA with fat suppression as the best initial screening test. [13,14] However, they also indicate that CTA and angiography scans can be obtained, especially if there is doubt in the diagnosis or the dissection is very early. [13,14] Management is targeted towards preventing stroke and also improving neurological outcomes. Most dissections will heal spontaneously, but each patient should receive treatment to prevent the possible thromboembolic and hemodynamic complications of dissection. This typically includes anticoagulation or antiplatelet agents, but some patients may require endovascular or surgical therapy. [15] There is no known superiority between antiplatelet or anticoagulant therapy, so either of both can be safely given to patients.
Prognosis is excellent with overall good functional recovery and low rates of recurrence of bleeding, dissection or ischemia.
10. VIII. Learning Points