1. Introduction
rimary paraovarian malignancy is an extremely rare condition, so much so that very little is known about their epidemiology, biological behaviour, prognosis, protocols for diagnosis and management. The incidence of paraovarian malignancy is also not known 16 . Very few cases have been reported in literature till date. We hereby present, to the best of our knowledge, the oldest patient in literature with pain in lower abdomen for last one and a half year and vaginal spotting for last 4 days. Patient was menopausal for last 30 years. On pelvic examination, cervix and vagina were assessed to be normal, uterus was normal and anteverted, a cystic mass of approximately 6x6 cm in size was felt close to uterus, and POD was free. USG was suggestive of thin walled anechoic cystic mass on right side, 8x6x6 cm with few internal septae. MRI pelvis showed large midpelvic right adnexal complex predominantly cystic lesion of size 8.7 x 7.1 x5.9 cm with small exophytic solid component (3.1x2.8x2.6 cm). The exophytic solid component was focally indenting anterior rectal wall with no apparent infiltration. Endometrial thickness was 1.7 mm, smooth regular margins and fluid -fluid levels were seen. Endometrial curettage was done and histopathology report showed senile endometrium. Her serum CA125 level was normal.
Patient underwent exploratory laparotomy. No ascites or peritoneal implants were seen. Peritoneal wash was sent for cytological examination. Both the ovaries, fallopian tubes and the uterus were normal in appearance. A large paraovarian cystic mass measuring 8x6x4cm was seen on right side with right fallopian tube stretched over it. TAH with BSO with cystectomy was done. Full biochemical and radiological examinations showed no evidence of metastasis or any other disease process. We staged the primary paraovarian tumour as T1aN0M0. Five weeks later, patient underwent 3 cycles of adjuvant chemotherapy with carboplatin and docetaxel. Patient is doing well in follow up visits till date (20 months post treatment).
2. III.
3. Pathology
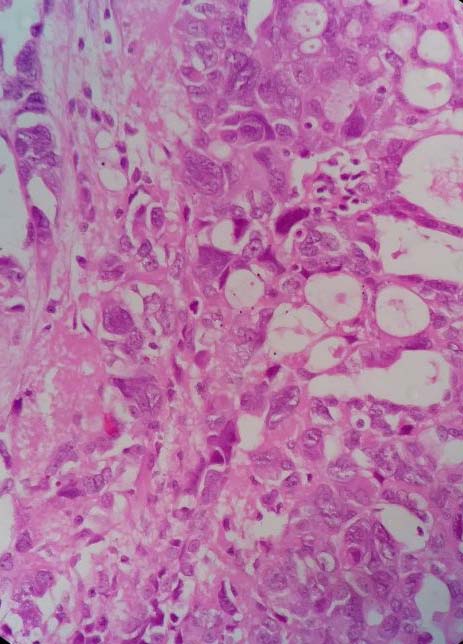
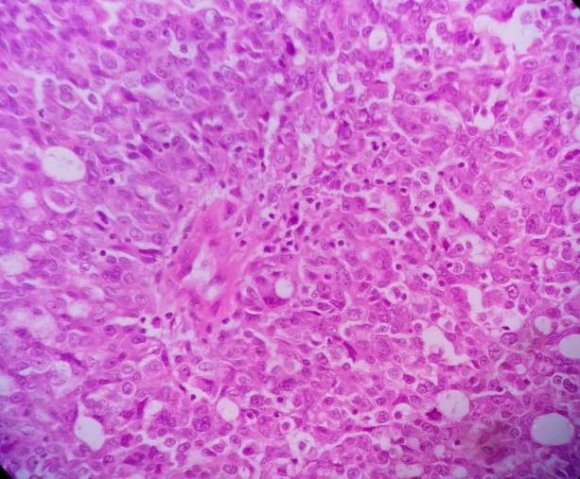
On postsurgical examination, peritoneal fluid cytology showed no evidence of malignancy. On macroscopic examination, paraovarian cyst was found to be uniloculated, filled with thin hemorrhagic fluid and a firm, greyish white nodule measuring 3x2.5x2 cm was seen in the wall of the cyst, which on cut surface was grey white, granular with large areas of necrosis. Rest of the cyst wall had smooth inner surface with foci of hemorrhages. No tumour was found in the bilateral ovaries and fallopian tubes. Microscopic examination of the right adnexal mass revealed malignant tumour with solid and tubulocystic pattern with cells lining the tubules having hobnail appearance. There was marked pleomorphism in the neoplastic cells in the solid area suggestive of high grade serous adenocarcinoma from paraovarian cyst (Fig. 1 and 2). Large areas of necrosis and stromal lymphocytic infiltration were seen. Sections of the cyst wall showed columnar to cuboidal to flattened cell lining with underlying fibrosis and infiltration by hemosiderin laden macrophages. There was no lymphovascular space invasion. Endomyometrium showed senile cystic atrophy with atrophic myometrium. Bilateral fallopian tubes and ovaries were unremarkable.
4. Discussion
Secondary tumours in broad ligament are not uncommon but primary tumours are rare. Commonly seen primary tumours are leiomyomata, serous and papillary cystadenoma of borderline malignancy but primary malignant tumours are very rare 9 . Primary broad ligament carcinoma as mesonephroma was first reported by Schiller in 1939 1 .
In our case primary tumour was located in or on the broad ligament and completely separated from ipsilateral ovary, fallopian tube, and uterus. This satisfies the criteria given by Gardner et al in 1957 to diagnose primary carcinoma of broad ligament origin 4 .
The age range in reported cases of broad ligament malignant tumours is 13 to 80 years (median 43 years) and the age range of borderline below the age of 40 years. To the best of our knowledge, ours (80 years) is the oldest case reported in the literature. In contrast, mean age of ovarian cancer is 63 years, being rare in women below 40 years 18 and mean age of borderline ovarian tumours is 10 years lower 19 .
Five were clear cell carcinoma (20.8%), two were papillary adenocarcinoma (8.3%), four were endometroid (16.6%), five including ours were serous adenocarcinoma (20.8%), one was mucinous carcinoma (4.1%), and one was well differentiated adenocarcinoma (4.1%) and five were borderline serous cystadenoma (20.8%) (Table 1).
Most common presenting symptoms reported are lower abdominal pain and pelvic discomfort 15 like in our case. Moreover, our patient also presented with vaginal spotting. Although most common cause for vaginal spotting in post-menopausal age group is senile endometritis 20 , there is a possibility of associated Hence it is important to rule out endometrial cancer in scenarios of vaginal spotting for postmenopausal women. In our case endometrial cancer was ruled out by endometrial curettage. It is to be noted that presentation of broad ligament tumour can be an incidental finding as well 9 . There is a 1.4 % to 3.8% chance of synchronous tumour of ovary and endometrium 20 but similar data about broad ligament tumour is not known due to rarity of cases. All the reported cases of broad ligament tumour (Table 1) including borderline variety were unilateral, in contrast to ovarian tumour which are 25% bilateral 21 .
For fourteen cases (58%) including ours, patients were diagnosed in stage 1 of broad ligament tumour. Two cases (8.3%) were diagnosed in stage 2, while three cases (12.5%) were diagnosed in stage 3. Staging was not known for the remaining five cases (20.8%). It is to be noted that majority of the cases, including our case, were diagnosed in stage 1. Possible reason for the same is that tumours are encapsulated between the sheets of broad ligament. Thus rupture as well as aggressive progression is prevented due to lack of vasculature 22 .
Management of broad ligament tumour is often done in a similar way as that of ovarian cancer because of similarities in histology and histogenesis, i.e. commonality in coelomic epithelium 10 . Post-surgical adjuvant treatment is not established as the standard procedure due to lack of evidence. It is recommended to use same principles as followed in the management of ovarian cancer 15 . Of the 24 cases, surgery was the singular mode of treatment in eleven cases (46%), surgery followed by chemotherapy in eight cases including our case (33%), surgery followed by radiotherapy in four cases (17%) while only radiotherapy was used in one case (4%).
5. Conclusion
Survival rates and prognostic factors are inconclusive due to rarity of the tumour, lack of uniformity in treatment modalities and improper reporting. Similar to cases of ovarian cancer, follow up is important to look for relapse or any residual disease left after adjuvant therapy.
We recommend that such rare cases be reported in literature so that consensus on diagnosis and management can be evolved and established.
| S. No. Author (year) | Age (years ) | Size (cm) | Pathological diagnosis | Treatment | Follow up | stage | |
| 1 | Schiller 1 (1939) | 43 | Child's head | Clear cell | TAH+BSO, Radiotherapy | Live, 24 months | 1 |
| 2 | Lennox 2 (1952) | 45 | 7x6.5x6 | Papillary adenocarcinoma | TAH+BSO, Radiotherapy | Live, 10 months | 1 |
| 3 | Telium 3 (1954) | 62 | Fist size | Clear cell | Enucleation | Not known | 2 |
| 4 | Telium 3 (1954) | 32 | 10x8x8 | Clear cell | Enucleation | Not known | 1 |
| 5 | Gardner 4 (1957) | 50 | - | Well differentiated adenocarcinoma | Radiotherapy | Live,27 months | -- |
| 6 | Merril 5 (1959) | 70 | 13 | Papillary adenocarcinoma | TAH+BSO, Radiotherapy | Live,12 months | 2 |
| 7 | Czernobilsky 6 (1972) | 29 | 5x4x4 | LMP Serous | TAH+BSO | Not known | 1 |
| 8 | Genadry 7 (1977) | 13 | 9x6 | Serous adenocarcinoma | Adnexectomy | Live, 60 months | -- |
| 9 | Genadry 7 (1977) | 38 | 9x6 | LMP Serous | Adnexectomy | Live, 60 months | -- |
| 10 | Genadry 7 (1977) | 36 | 9x6 | LMP Serous | Adnexectomy | Live, 60 months | -- |
| 11 | Genadry 7 (1977) | 28 | 9x6 | LMP Serous | Adnexectomy | Not known | -- |
| 12 | Clark 8 (1979) | 29 | 8x7x2 | Mucinous adenocarcinoma | TAH+BSO+ omentectomy | Not known | 1 |
| 13 Aslani 9 (1989) | 51 | 10x6x6 | Clear cell | Excision+BSO+ omentectomy, Radiotherapy | Live, 7 months | 1 | |
| Excision+TAH+BSO, | |||||||
| 14 Aslani 9 (1989) | 29 | 6x6x5 | Endometroid | inguinal and paraaortic lymph node sampling, | Live, 18 months | 1 | |
| Chemotherapy | |||||||
| 15 | Aslani 9 (1989) | 69 | 11x8 | Endometroid | Excision of tumor + TAH+BSO, Chemotherapy | Live, 12 months | 1 |
| TAH+BSO+ plevic | |||||||
| 16 | Aslani 9 (1989) | 34 | 4.5x4x3.5 | Endometroid | and paraaortic lymph node dissection+ omentectomy, | Live, 6 months | 1 |
| Chemotherapy | |||||||
| 17 | Altaras 11 (1990) | 76 | 12x9x8 | Serous | TAH+BSO | Live, 53 months | 1 |