1. Introduction
remature rupture of membranes (PROM) can happen at term or subsequently before labor, otherwise can be an unanticipated difficulty through the preterm phase. PROM can be classified as term PROM (TPROM is PROM following gestation of 37 weeks), and preterm PROM (PPROM, that is PROM before gestation at 37 weeks). The pathophysiology directing to TPROM and PPROM are dissimilar. At TPROM, flagging of the membranes can happen due to physiological modifications merged including shear force stimulated by shrinkages. [1][2][3][4] Widespread flaw of the membranes are problematic for identification having PROM. [5] PPROM can occur due to a focal deficit instead by the membrane weakness. [6] TPROM difficulty occurs around 8% of all pregnancies. [7] Women who starts labor naturally about 50% of them by 12, 70% by 24, 85% by 48, and 95% by 72 hours. [7][8][9] TPROM linked to fetal illnesses consist of soaring infection and in utero cord compression. [7] Maternal hazards of TPROM are chorioamnionitis and postpartum febrile illness. [7,9] PPROM, is a difficulty from 2% -20% of entire deliveries, [10] is a recognized vital sponsor to maternal and perinatal illness and perinatal death. Dormancy in PPROM which is the time from PROM to birth, [7] is inversely linked to gestational age at rupture, related to fetus numbers, [11] oligohydramnios difficulty, [12] myometrial thickness, [13] and the presence of child birth or maternal difficulties. The vital reason of perinatal illness and death related to PPROM is prematurity. [7] Illnesses due to prematurity are interventricular hemorrhage, respiratory suffering symptoms, cerebral palsy, sepsis, and necrotizing enterocolitis. [7] Additional difficulties are inutero umbilical cord compression, fetal distress, cord prolapse, placental abruption, fetalunusual position at delivery time, chorioamnionitis following endometritis, and hazards of delivery by operation. [7] For over seven decades, there has been debate amid healthcare experts regarding the ideal method to clinical examination and identification of PROM. Mostly membrane rupture may be established by documenting amniotic fluid leak from the cervical os in the posterior vaginal fornix assembly. [14] PPROM happens in about 3% of entire pregnancies and is accountable for 33% of entire preterm births. PPROM influences 120 thousand pregnancies in the USA every year. The identification of PPROM is obtained through a blend of experimental doubt, history of patient and couple of examinations. PPROM is linked to substantial maternal and neonatal illness and death by infection, placental abruption, preterm birth, and umbilical cord compression. The positive cultures rate provided by trans-abdominal amniocentesis with PPROM without labor is 25% to 40%.The best duration for delivery happens in PPROM when the dangers of immaturity are offset due to the hazards of pregnancy preservation. Age at gestation related to cure is vital and ought to be regulated by neonatal intensive care unit (NICU) in every hospital. Antenatal antibiotics and corticosteroid therapies have pure advantages to women exclusive of condition making the treatment risky. Women are supervised carefully for labor, infection, placental abruption, as well as anun-encouraging fetal condition in conservative management. Women having PPROM after gestation at 32 weeks must be considered for delivery, and the advantages of delivery obviously compensate the dangers after 34 weeks.
PROM identification is problematic if there is a sluggish liquid leakage or bleeding, or if the normal liquid flow does not happen. [15] Also, the comparatively small quantity of amniotic fluid found in initial in gestation tests the identification of ruptured membranes. [16] It is seen that even proceeding 34 weeks in pregnancy, speculum exam for conception of amniotic fluid gives a12% false negative without presence of fluid. [17] A "two sac" theory of membrane rupture was given in 1951. [18] Rupture of membranes is not totally clear in around 20% to 25% of cases. [19] Early and precise identification of membrane rupture could permit forage at gestation particular interference to enhance perinatal result as well as minimizing severe difficulties. [20] A precise biochemical marker intended for membrane rupture must possess a low maternal blood concentration, a high amniotic fluid concentration, also a short background cervicovaginal discharge concentration having intact membranes. [21] There are not many documents reported for preterm rupture of membrane in Bangladesh. As it has been an important issue to understand and the urgency to detect PPROM at an early stage and also its proper diagnosis, cases must be reported to overcome the limitations of early successful detection and treatment. The objective of this study was to diagnose a PROM case and to provide proper treatment as well as prevention of subsequent complications. The reason for this study was to review the consequence of infant delivered after spontaneous rupture of membrane at 28 weeks' gestation.
2. II.
3. Case Report
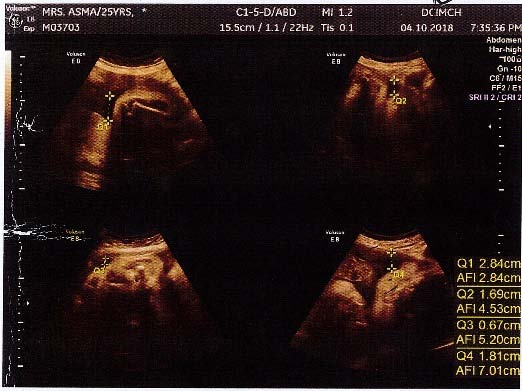
This is a case study which was carried out at a modern tertiary care hospital, Dhaka Central International Medical College and Hospital, Dhaka, after taking approval of the institutional ethical committee. The patient was selected for this study after reporting liquor escaping from her vagina and went through proper treatment and recovery. Routine examinations were performed as well as regular monitoring was done by the surgeon on the patient. Mrs. A, a primigravida patient having 28 weeks of pregnancy have a history of per vaginal watery discharge for 2 weeks. She conceived after 7 years of married life by ovulation induction drug. She had history of hypothyroidism and Gestational diabetes mellitus, and was on Insulin. She had no history of fever and abdominal pain. Perspeculum examination shows the liquor escaping out through the cervix, but the cervix was closed. Then she was shifted from a hospital from district Comilla to a tertiary care center Dhaka Central International Medical College and Hospital, Dhaka immediately for better management. Some investigations were send like CBC, C-reactive protein (CRP), Blood sugar, HbA1c, Urine R/M/E and USG of pregnancy profile then started injectable antibiotics and other hormonal supports. Her Hb% was 10.2 g/dl, CRP 12 mg/L (which was within normal limit), urine R/M/E was normal, but her HbA1C level was 9.6%, FBS 8.1 mmol/L, 2 HABF 11.3 mmol/L. Then gradually increasing her insulin dose USG of pregnancy profile showed viable single pregnancy of about 31+ weeks with moderate oligohydramions. Her Amniotic fluid index (AFI) was 5.95 cm and foetal weight 1656 gm (± 24 grams). High vaginal swab (HVS) was sent for culture, which reported nothing significant. After admission her blood sugar level was controlled day by day by increasing insulin. But she still complained of per vaginal watery discharge, which continuously happened. So, CRP was repeated and USG of pregnancy profile was done to see foetal weight and AFI level. But her CRP was always normal limit. On USG, AFI level was also within normal level. She never complained of lower abdominal pain. So, conservative treatment was continued and in the meantime Oradexon dose was completed for lung maturation of the baby. At 32 weeks of pregnancy she complaint of severe lower abdominal pain, which was increasing in nature. After per vaginal examination, cervix was 6 cm dilated. Then patient was taken to operation theatre for emergency caesarean section. A healthy female baby was delivered, the baby cried immediately, and baby weight was 2.7 kg. After operation both mother and baby were in good health. After post operation, the newborn was kept in NICU support for 7 days. The baby did not have infection. On the third day bilirubin level of baby was increased, phototherapy was given. The patient and the baby were discharged at fifth post-operative day (POD).
4. III.
5. Discussion a) Examination and assessment
PPROM analysis is formulated through clinical doubt, history of patient and examination. History of patient has a 90% precision for the identification of PPROM. [23] Two examinations have been endorsed for the analysis of PPROM: Nitrazine paper testing and also ferning testing on the vaginal pool. It was concluded that if a blend of history of patient, ferning, and nitrazine testing are utilized to examine a patient diagnosing for PROM, the precision of minimum 2 affirmative examinations was 93.1%. [23] The ferning test ought to be done on mid-vaginal or rear-end fornix fluid; pollution with mucus from cervix may trigger an erroreous positive outcome. [24] The existence of bacterial vaginosis, alkaline urine, cervicitis, semen, soap, antiseptic liquids, and blood was discovered to modify the nitrazine test, mostly giving false positive outcomes. [24,25] A digital cervical inspection must be shunned during examination and assessment of PPROM. Digital cervical examination has been linked to the sterile speculum test and concluded that inactivity was decreased substantially utilizing cervical exam for all ages at gestation. [
6. 26] b) Infection
There are various risk factors that can be linked to PPROM. They are: excessive collagen degradation and membrane stretch, placental abruption, localized membrane flaws, advanced automated death of amniotic cell, and choriodecidual infection. [22,23,28,29] Prior to 32 weeks of gestation, expectant management is chosen whenever probable to reduce the dangers of premature delivery. Proceeding gestational age of 32 weeks, the occurrence of substantial neonatal illness as well as death reduces drastically. A project showed the rate for survival of children delivered proceeding gestational age of 32 weeks surpassed 96% while rates for survival enhanced by less than 1% weekly afterwards. [30] The resultant assessment of perinatal illness for this same patient group shown that the occurrence and gravity of respiratory suffering pattern gradually reduced by means of rising gestational age past 36 weeks of gestation. [31] Neonatal problems having possibility of prolonged condition are infrequent after gestation at 34 weeks. These studies reveal the dangers of harmful neonatal consequence linked to preterm deliveries from all reasons. [32] PPROM is capable of upsetting 4.5% of total pregnancies. [33,34] From 60% to 80% women that have their membrane ruptured before term would deliver by 7 days. [33,34] PPROM explains for 40% to 50% of preterm births [35,36] and is related to an elevated proportion of neonatal illness than gestational age related idiopathic preterm labor. [37]
7. c) Risk factors
Multiple etiologic danger features for PPROM are proposed, e.g. socioeconomic status, ethnicity, nutrition, and smoking. [34,38] Epidemiological data have shown that cervical issue, vaginal bleeding, multifetal pregnancies, poor obstetric history, preexisting medical conditions, and genital tract infections [34] are linked to PPROM. Trouble-free uterine action that creates modification and dilation of the cervix, having secondary PPROM is a frequently neglected possible reason. [36] Having a PPROM history substantially elevates the danger in a succeeding pregnancy, [39] and chorioamnionitis has been found for 24% to 30% patients having PPROM during rupture. [36,40] The membranes rupture mechanism is not known, said to be directly linked to the membrane collagen. [35,38] An elevation in the ratio of matrix metalloproteinase to tissue inhibitors of matrix metalloproteinase due to disorders in connective tissue or poor nutrition has been stated to be the reason . [35,[41][42][43]
( D D D D ) d) SupervisionPPROM happening before gestation ought to be expectant supervision [44,45] due to the substantial neonatal morbidity linked to prematurity upto 34 weeks of gestation. The best supervision of women that stay undelivered one week after membrane rupture, who attain gestation at 34 weeks, and who have membrane ruptures after 34 weeks is still debatable. [46][47][48][49][50] Supervision of women having PPROM prior to gestation at 34 weeks normally consists of reference to a tertiary care hospital owing to the preterm birth risk, one course of corticosteroid administration, [51] tocolysis for transfer or'corticosteroid administration, [52] broad spectrum antibiotic therapy, [53,54] and probable outpatient supervision. [55] Clinical supervision of women from 34 to 37 weeks' gestation remains debatable. [55,56] Active supervision in this interval involves instant initiation of labor, with the possible hazard of prematurity necessitating NICU supervision. Expectant management can extend pregnancy but can elevate the risk of chorioamnionitis [57] having related maternal, fetal, and neonatal consequences. [58] e) Therapeutic involvement Therapy has been endeavored after PPROM using cryoprecipitate injected into the amniotic cavity and autologous platelets, having changeable outcomes in minor analyses; additionally amniotic membranes "Laser welding" throughout fetoscopy is in the investigational phase. [60] Given the insensitivity and questionable usefulness of involvements proceeding PPROM, more effort is needed into primary prevention and research intended to improve neonatal outcomes. Current epidemiological results, [61,62] which are reinforced by animal experiments, [63] suggest in utero infection to be a key danger feature in case of the growth of perinatal brain injury. More research for PPROM and the related danger of perinatal brain injury are needed. [64] IV.
8. Conclusion
PPROM is linked to considerable maternal illness and neonatal illness and death. Healthcare prices are drastically increased due to long term stay at hospital, the requirement of recurrent analysis and the subsequent neonatal price for newborn due to long lasting neonatal intensive care. Management necessitates a precise examination and age at gestation finding. A gestational age method to cure is vital which ought to be regulated for each case. Corticosteroid treatments and antenatal antibiotics have well-defined advantages and must be accessible for all women not having contraindications. Women ought to be supervised carefully in conservative management for labor, infection, a non-reassuring fetal stage, and placental abruption. PPROM patients must be deliberated for delivery of gestation after 32 weeks, and the advantages of optional delivery seem to compensate the dangers after 34 weeks.
9. Source of Support None
Conflict of interest There is none.
10. Global