1.
clinical problem for implant placement. Implants must be placed with at least 1mm of bone on the buccal and lingual aspects in order to maintain crestal bone levels. [1]The pattern and degree of dimensional changes that occur in the alveolar ridge after tooth extraction has been documented in the literature for more than 50 years. [2, 3 & 4] There is a disproportionate resorption of the buccal plate as compared to the palatal/lingual plate of the ridge with the buccal plate undergoing significantly more resorption. [6] The final outcome of this is not only narrowing of the ridge but a palatal/lingual shift of the mid-line of the ridge. Lekovic et al reported that loss of width was three times greater than the loss of height. [5] Substantial tissue loss leads to increased difficulty in placing the implant fixture in a prosthodontically suitable position.
The lateral ridge expansion technique is usually performed simultaneously with implant placement and significantly shortens the treatment time. This technique is aimed at creating new implant bed by performing longitudinal osteotomy. This technique is usually recommended for atrophic maxillary ridge. Studies related to the posterior mandibular segment are limited. Though the literature recommends immediate and delayed ridge expansion techniques, it is not clear which technique is superior and comparative studies are not available. In view of the above, the present study was undertaken to comparatively analyse the immediate and delayed ridge expansion technique in posterior edentulous mandibular region in armed forces personnel and their dependents for early prosthetic rehabilitation.
2. II.
3. Material and Methods
4. Patients
reporting for replacement of mandibular posterior teeth were included in the study. The total sample size was 40. The patients were randomlyselected and divided into two groups of twenty each: Group-I patients undergoing immediate ridge expansion along with placement of implants and Group-II patients undergoing delayed(staged) ridge expansion with placement of implants. Implants were loaded in a conventional manner after six months. Crestal bone loss(six and twelve months post implant placement) and bone width gain(base line and post operative) was Introduction ental implants provide a novel method of successful and predictable treatment of partial or complete edentulism. The resorption of alveolar bone is a common sequel of tooth loss and presents a D assessed. Crestal bone loss was evaluated using standardised radiographs using radiovisiograph (RVG). Bone width was evaluated using Cone Beam CT.
5. a) Inclusion criteria
? Patients with missing teeth in the mandibular posterior region with atrophic ridges with width <5mm and adequate height.
? Patients with at least 18 years of age and should be systematically healthy. ? A period of bone healing of at least one year after tooth extraction. ? Able to understand the study procedure and provide signed informed consent.
6. b) Exclusion criteria
? Systemic disorders tending to affect the surgical intervention and outcome. ? Irradiation in the head and neck area.
? Patients with bruxism and untreated chronic periodontitis. ? Patients with poor oral hygiene and smokers.
? Exhibiting excessive vertical ridge resorption that requires vertical augmentation. ? Presently on IV bisphosphonates or having taken long term oral bisphosphonates for more than three years.
Before starting with the treatment, preliminary diagnosis and treatment planning procedures were carried out.
7. c) Group 1 (Lateral ridge expansion technique)
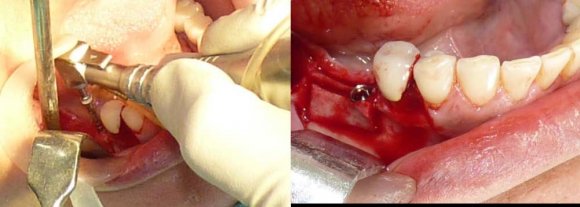
Detailed medical and dental history was recorded and cone beam computed tomography was performed to gauge the bone quality and estimate the amount of available bone. Preoperatively the bone width was also evaluated using calipers and bone mapping. Routine blood and urine investigations were carried out before the surgical procedures. The procedures were explained in detail to the patient after diagnosis and treatment planning and informed consent was obtained. Surgery was performed under local anaesthesia under strict aseptic conditions. The first surgical procedure involved a simple corticotomy at the crestal and buccal aspect of the edentulous ridge. A full thickness mucoperiosteal flap was raised exposing the buccal aspect of the mandibular alveolar ridge. Crestal osteotomy was done using Piezo surgical device (Piezon Master Surgery ® , Nyon, Switzerland). The horizontal osteotomy was started 2 mm away from the adjacent tooth. The caudal ends of the vertical cuts were connected with a horizontal corticotomy. All osteotomies were 3 to 4mm in depth, thereby only the cortical bone was dissected, and the cancellous bone was not significantly affected. Subsequent to this, further bone split and expansion was carried out using MCT ridge splitting and bone expander kit (MCT, Korea) (Figure 1). Approximately 3 to 4mm of expansion was achieved which was measured intra-operatively using surgical caliper which was also later confirmed using post operative cone beam tomography. AB TM (A.B. Dental, Israel) implants were placed following manufacturer's instructions (Figure 2). Interpositional graft used was synthetic bone graft, NovaBone ® (Novabone Dental, Atlantic Blvd, USA).
Tension free soft tissue closure was achieved using 4-0 non resorbable sutures. Sutures were removed after seven days and loading protocols was done in the convnetional manner. After six months, the surgical site was evaluated both clinically and radiographically for osseointegration. Second stage surgery was performed and rotine laboratory procedures were carried out for porcelain fused to metal crown following manufacturers instructions and crown cemented using Type 1 glass ionmer cement (GC Fuji, Japan).
8. d) Group II (Delayed/Staged ridge expansion with placement of implants)
The first step involved a simple corticotomy at the crestal, buccal aspect of the edentulous segment performed under local anaesthesia. After crestal and intracrevicular incisions had been made around the buccal aspects of the adjacent teeth, a mucoperiosteal flap was elevated to expose the buccal aspect of the mandible. Crestal corticotomy line cut into the alveolar ridge was done by using piezosurgical device (Piezon Master Surgery ® , Nyon, Switzerland). On the proximal and distal ends of the crestal corticotomy,vertical cuts were made on the buccal cortical plate. The caudal ends of the vertical cuts were connected with horizontal corticotomy (Figure 3). All osteotomies were 3 to 4 mm in depth, thereby only the cortical bone was dissected, and the cancellous bone was not significantly affected. The mucoperiosteal flap was repositioned and fixed with 4-0 nonresorbable sutures.
The second step included splitting and lateralisation of the pedicled buccal bone segment 40 days after the primary step. A crestal and intracrevicular incision around the lingual aspect of the adjacent teeth was performed to expose the area of the crestal osteotomy and to elevate a lingual full thickness flap. A microscalpel was used as a chisel to separate the cortical plates from one another. Care was taken to leave the buccal periosteum attached to the buccal cortical plate. Gradual lateralisation of the buccal segment was performed with a series of bone expanders (Figure 4a) after green stick fracture at the base of the cortical segment untill a 3 to 5mm gap was established between the bone plates. Implant beds were prepared conventionally but without damage to the crestal bone, and dental implants AB TM (A. B. Dental, Israel) were placed in the preplanned positions (Figure 4b). The gap between the implants and cortical plates was filled with NovaBone ® . The submerged implants were allowed to heal for six months before uncovering and prosthetic loading. Prosthetic loading was done in the similar manner described for Group I.
CBCT was done before and after surgical procedure to evaluate bone width gain (Figure 5). Data generated were subjected to statistical analysis. RVG was taken using the long cone paralleling technique and assessed at the time of implant placement, 6 months and 12 months post implant placement. Radiographs were taken following manufacturers recommendations with the grid. The bone level and amount of bone resorption was measured from the crestal bone level to the implant crest module at mesial and distal sites. This was done at the time of implant placement, six months and 12 months (Figure 6) post implant placement. Data collected were subjected to statistical analysis.
9. III.
10. Results
Table 4 and Graph 2 reflects mean and standard deviation for crestalbone loss for the two groups by sites t. e. (Mesial and Distal) and periods i.e. 6 months and 12 months respectively. Between the treatment groups mean bone losses appear to be practically equal within sites and also within periods. Between periods mean bone losses are higher in 12 months period compared to the 6 month period for each site numerically.
The descriptive statistics for bone width for the groups ignoring treatment points (pre and post) based on 40 observations each. For IRE bone width varies from a minimum of 3.7 to a maximum of 7.80 with mean ± standard deviation as 5.66 ± 1.62. For DRE bone width varies from a minimum of 3.8 to a maximum of 7.80 with mean ± standard deviation as 5.74 ± 1.59. The descriptive statistics for bone width for the treatment points ignoring the groups based on 40 observations each. For pretreatment time point bone width varies from a minimum of 3.70 to a maximum of 4.76 with mean ± standard deviation as 4.14 ± 10.2530. For post treatment time bone width varies from a minimum of 6.80 to a maximum of 7.80 with mean ± standard deviation as 7.27 ±0.2832 there is a mean increase of 3.13 from pre to post numerically.
Table 5 and Graph 3 presents descriptive statistics regarding groups ignoring sites and periods based on 80 observations each. For IRE the bone loss varies from a minimum of 0.10 to a maximum of 1.00 whereas for DRE the values vary from a minimum of 0.20 to a maximum of 0.80. Mean bone losses are 0.5063 and 0.4950 respectively. The descriptive statistics regarding periods ignoring sites and groups based on 80 observations each. For the period of 12 months bone loss varies from a minimum of 0.10 to a maximum of 1.00 whereas for that of 6 months the values vary from a minimum of 0.20 to a maximum of 0.80. Mean bone losses are 0.6350 and 0.3663 respectively. The descriptive statistics regarding sites ignoring periods and groups based on 80 observations each. For Distal bone loss varies from a minimum of 0.10 to a maximum of 0.90 whereas for mesial the values vary from a minimum of 0.20 to a maximum of 1.00. Mean bone losses are 0.5313 and 0.4700 respectively.
Table-6 presents Two Factor Analysis of Variance (ANOVA) for bone width. Factors are treatment group at two levels i.e. IRE and DRE) and treatment time also at two levels: Pre and Post. From the ANOVA table we find that there is no interaction between the two factors namely Group and Times (F= 0.29, P = 0.5890). There is also no statistically significant difference in mean bone width between the two groups (F= 1.67, P = 0.2000). However difference in mean bone width between the pre and post treatment times is very highly significant (F= 2721.74, P = practically zero). The Post treatment Mean bone width higher than that of pretreatment time by 3.73. Table-7 presents Three Factor Analysis of Variance (ANOVA) for bone loss. Factors are treatment group at two levels i.e. IRE and DRE, sites at two levels: Distal and Mesial and Period also at two levels: 6 months and 12 months. From the ANOVA table we find all interactions were not significant. The interactions and related F and P values are as follows: Group X Period: F= 0.090, P = 0.765; Group X Site: F= 0.030, P = 0.857; Period X Site: F= 0.180, P = 0.675 and Group X Period X Site -F= 0.001, P = 0.952. Here also There is no statistically significant difference in mean bone loss between the two groups: (F= 0.290, P = 0.0569). However difference in mean bone loss between the two sites as well as the difference between two periods for the same are statistically highly significant: (F= 8.640, P = 0.004 and F=166.31, P = 0.00001 respectively). Mean bone loss for Distal = 0.5313 and for Mesial it is equal to 0.4700. For 12 Months period mean bone loss = 0.6350 and for 6 month it is = 0.3663.
11. IV.
12. Discussion
Rehabilitation of partial or total edentulism with dental implants has been established as a predictable treatment modality with high success rates. [6][7][8][9][10][11] However, insufficient width of the alveolar ridge due to atrophy, periodontal disease or trauma may render implant placement impossible. In such cases, bone grafting, guided bone regeneration, alveolar ridge splitting and combinations of these techniques have been suggested for lateral augmentation of the alveolar ridge prior to implant insertion. In some patients, the use of narrow implants can solve some cases, but when the bone width is 3 mm or less it is not feasible to contemplate the safe and stable installation of dental implants.
Ridge splitting technique is well documented treatment option for augmentation of the bucco-lingual dimension of the alveolar ridge which was first described by Tatum [12]. Compared with guided bone regeneration or bone grafting, the ridge splitting technique enables simultaneous implant placement, eliminates the need for bone harvesting and reduces a risk of graft or membrane exposure. Therefore, the overall treatment time is shortened and morbidity is reduced. [13,14]. This technique has turn out to be a rational procedure and a 98% to 100% survival rate was reported following the contextual insertion of implants [15].
On the other hand, this technique can be used for horizontal deficiencies, but not for vertical augmentation. Thus, it can be applied for augmentation of alveolar ridges with adequate height. Moreover, the ridge splitting technique necessitates a minimum of 3mm of bucco-lingual width with at least 1 mm of cancellous bone between the 2 cortical plates, which would allow introduction of instruments and the maintenance of good blood supply to the split parts. [16]. Scarano et al. recommended the two-stage technique with conventional loading of the implants, since this might prevent unplanned fracturing of the vestibular wall, reducing complications and obstacles to treatment [17]. In contrast, Shibuya et al. stated that even if a malfracture occurs, a sufficient volume of alveolar bone can be obtained using a free bone segment without rigid fixation and dental implants placed within the malfracture area show a good prognosis [18].
Of the techniques described for SCT, there is no consensus regarding the preferred technique for ridge expansion. But the most commonly employed technique includes immediate lateral ridge expansion along with placement of implants. Delayed (staged) ridge expansion was preferred by only few researchers. Second issue is it is applicability to mandibular ridge. Ridge splitting with bone expansion is a technique of shuffle of bone to form receptor site for implant without removing any bone from the implant site. Maxillary bone has inherent quality of flexibility which can bemolded to desire location by using series of instrument namely chisels and osteotome. But in mandible, the procedure is questionable. Maximum studies are related to maxilla and there are few studies related to mandible.Therefore this study was designed to compare these two techniques in mandibular ridge.
We used NovaBone ® (Novabone Dental, Atlantic Blvd, USA) to fill the gaps. NovaBone Putty is a bioactive synthetic graft with osteostimulative and osteocon-ductive property. Spaces between particles of novabone putty permit rapid vascularization and bone ingrowth. This material has been extensively researched and proven material [19]. In our study also this material proved to be effective. Few studies used only resorbable membranes [20]. Some studies did not use any graft or membrane, but nonetheless achieved a high success rate [21]. We preferred to place a resorbable collagen membrane in conjunction with ridge split procedure after bone grafting and found favourable results without any complications.
Alveolar ridge splitting is classically performed by means of chisels and hammer, rotary burs, diamond disk, reciprocal saw and piezoelectric device [22]. The use of bone chisels is time consuming and requires technical skills and a long learning curve. The alveolar ridge split procedure performed with rotating saws orbursis more rapid, but soft tissues and delicate anatomical structures can be damaged; close access to adjacent teeth can be difficult, and there is a high risk of losing control over the cutting device. However, Vercellotti et al. introduced piezo surgery in the treatment of the atrophic jaw. Piezo surgery made split technique safer, effortless and also reduced the risk of complications in the treatment of extreme atrophic crests [23]. Piezosurgery is a reliable procedure with adequate scientific evidence [24] and our study also supports the use of Piezosurgical unit for precise and efficient osteotomy in ridge split and expansion techniques.
One of the main parameters which was evaluated in our study was the bone width gain after ridge split and expansion in relation to both the procedures. There was considerable bone gain after the ridge expansion procedures in our study as reflected in Table1-3 and Chart 1. Both the techniques produced equally good results. In IRE group, the mean bone width has increased by 3.16 units. In DRE group, the mean bone width has increased by nearly the same magnitude i.e. 3.095. This is in agreement with previous studies. Chiapasco M [25] reported an increase in ridge thickness by 2 to 5mm right after the procedure.
The second parameter was the crestal bone changes in relation to both the procedures. Yoon J M et al [26] reported mean marginal bone loss of implants of 1.57±1.44 mm at the mesial side and 1.42±1.48 mm at the distal side. Evaluation of crestal bone levels reflected bone resorption with acceptable limits and in accordance with previous studies. For IRE the bone loss varied from a minimum of 0.10 to a maximum of 1.00 whereas for DRE the values varied from a minimum of 0.20 to a maximum of 0.80. Mean bone losses are 0.5063 and 0.4950.
Clinical trials have reported success rates ranging from 98 to 100%. [27,28]. The survival rates of implants immediately placed in expanded sites ranged from 91% to 97.3%, while the success rates varied from 86.2% to 98.8%. Whereas in our study the success rate was 100%. One major drawback of alveolar bone splitting is the requirement of a cancellous bone compartment between the buccal and lingual plates to allow separation.
V.
13. Conclusion
The ridge splitting technique seems to be a minimally invasive option for horizontal augmentation of narrow alveolar ridges. Predictable clinical results can be achieved as long as a proper preoperative evaluation is performed and a precise surgical and laboratory protocols are followed. Within the limitations of the current study, the following conclusions were drawn:
1. Use of ridge splitting technique offers great advantage of placing dental implant at same surgical appointment in ?3 mm of bone width.
2. Based on the parameters evaluated, the techniques be successful and comparable without any complications. The present study demonstrated that none of the implants placed in the bone gap created by ridge expansion was lost and all were successfully Osseo integrated. Hard as well as soft tissue structures revealed favourable and stable results with a follow-up period of one year.
3. The lateral ridge expansion technique is effective for horizontal augmentation in the severely atrophic posterior mandibular ridge. The delayed lateral ridge expansion technique can be used more safely and predictably in patients with high bone quality and thick cortex and a narrower ridge in the mandible.
4. Future clinical studies with carefully selected patient populations, control groups, and well-documented methodologies are required to adequately assess the performance of the SCT, since the high implant success rates may represent a bias related to patient pre-screening.
5. More well-designed, long-term randomized control trials are required to understand the effect of flap design and immediate implant placement on marginal bone resorption in ridge split done in mandible.

| Case No. | Pre treatment | Post treatment |
| 1 | 4.2 | 7.5 |
| 2 | 3.9 | 7.4 |
| 3 | 4.1 | 7.2 |
| 4 | ||
| 5 | 3.8 | 7.1 |
| 6 | 4.3 | 7.3 |
| 7 | 4.4 | 7.5 |
| 8 | 4.7 | 7.0 |
| 9 | 4.1 | 7.5 |
| 10 | 4.0 | 7.8 |
| 11 | 4.5 | 7.4 |
| 12 | 3.9 | 7.1 |
| 13 | 4.2 | 7.6 |
| 14 | 4.2 | 7.1 |
| 15 | 4.4 | 7.8 |
| 16 | 4.0 | 6.8 |
| 17 | 4.6 | 7.3 |
| 18 | 3.9 | 6.9 |
| 19 | 4.1 | 7.0 |
| 20 | 4.4 | 7.5 |
| GROUP-I (IRE) | GROUP-II (DRE) | |||
| PRE TREAT | POST TREAT | PRE TREAT | POST TREAT | |
| MEAN | 4.085 | 7.245 | 4.195 | 7.29 |
| SD | 0.24978 | 0.28373 | 0.24809 | 0.28818 |
| PERIOD | 6 MONTH | 12 MONTH | |||
| SITE | MESIAL | DISTAL | MESIAL | DISTAL | |
| GROUP-I | MEAN SD | 0.35 0.16059 | 0.4 0.15559 | 0.605 0.17313 | 0.67 0.13416 |
| GROUP-II | MEAN SD | 0.33 0.10311 | 0.385 0.10399 | 0.595 0.10501 | 0.67 0.09234 |
| GROUP | N | MEAN | S.D. | MINIMUM | MAXMUM |
| GROUP-I | 80 | 0.5063 | 0.2046 | 0.10 | 1.00 |
| GROUP-II | 80 | 0.4950 | 0.1735 | 0.20 | 0.80 |
| Factor | Type | Levels | Values | ||
| Groups | Fixed | 2 | Group-I, Group-Ii | ||
| Pre/Post | Fixed | 2 | Pre Treatment, Post Tretment | ||
| ANOVA | |||||
| SOURCE | DF | SS | MS | F | P |
| Group | 1 | 0.102 | 0.102 | 1.67 | 0.2000 |
| Pre / Post Treatment # | 1 | 195.625 | 195.625 | 2721.74 | 0.0000 |
| Group* Pre/Post | 1 | 0.021 | 0.021 | 0.29 | 0.5890 |
| Error | 76 | 05.462 | 0.072 | ||
| Total | 79 | 201.229 | |||
| Factor | Type | Levels | Values | |||
| Group | Fixed | 2 | Group-I Group-Ii | |||
| Period | Fixed | 26 | Month 12 Month | |||
| Site | Fixed | 2 | Distal Mesial | |||
| ANOVA | ||||||
| SOURCE | DF | SS | MS | F | P | |
| Group | 1 | 0.00506 | 0.00506 | 0.290 | 0.590 | |
| Period | 1 | 2.88906 | 2.88906 | 166.310 | 0.00001 | |
| Site | 1 | 0.15006 | 0.15006 | 8.640 | 0.004 | |
| Group*Period | 1 | 0.00156 | 0.00156 | 0.090 | 0.765 | |
| Group*Site | 1 | 0.00056 | 0.00056 | 0.030 | 0.857 | |
| Period*Site | 1 | 0.00306 | 0.00306 | 0.180 | 0.675 | |
| Group*Period*Site | 1 | 0.00006 | 0.00006 | 0.001 | 0.952 | |
| Error | 152 | 2.64050 | 0.01737 | |||
| Total | 159 | 5.68994 | ||||