1. Introduction
roximal femur fractures include fracture neck of femur, inter and Subtrochanteric fractures. These result in mortality and morbidity in the elderly population aged above 50 years. 14-36% of patients expire within one year of proximal femur fractures. 1 This increases to 50% in nonoperative patients. The incidence of these fractures is increasing in India with the aging population, which can soon or later become an epidemic in orthopedic surgery. These fractures have added stress to limitedly available health resources of country. 2 Patients who sustain second hip fracture is about 10-13%, which further adds to decreased mobility status and increased social dependence. 2 70% of women (>80 years) have osteoporosis, with 60% experience one or other fractures (hip fractures, vertebral compression fractures, distal end radius fractures, shoulder fractures, pelvic fractures mainly pubic rami fractures). 3 Minimal trauma and domestic falls can result in these fractures. Many factors influence post-operative mobility in patients with proximal femur fractures, such as osteoporosis, age of patient, time of presentation to hospital after injury or fall, presence of co-morbidities, surgery (surgeon, reduction, surgery time), post-surgery mobilization, social help for recovery, mental status of patients before the surgery. 4 Osteoporosis (senile, secondary) causes of proximal femur fractures in the elderly. We do want to find, whether there exists a correlation between osteoporosis and post-operative mobility of the patient, time required for returning to daily activities of living. Hence we propose a Null Hypothesis that there exists no correlation between these variables in proximal femur fracture patients.
2. II.
3. Materials and Methods
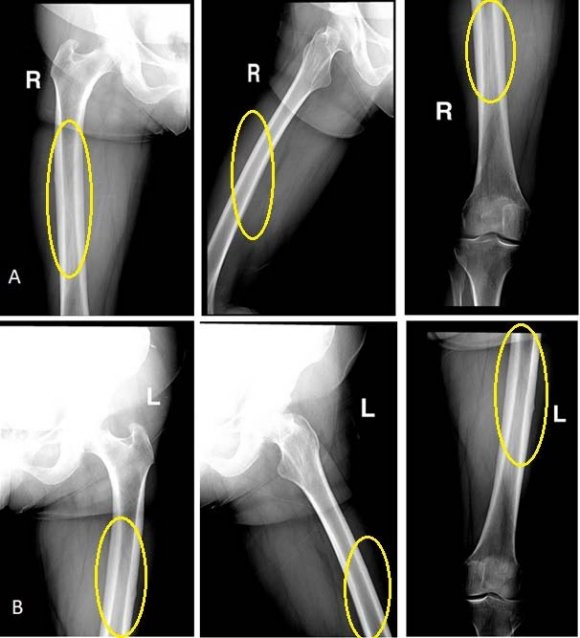
A retrospective study conducted from 1 st March 2017 to 1 st March 2018. All proximal femur fracture admitted into BIRRD (T) hospital and those underwent surgery, included in the study after satisfying inclusion and exclusion criteria. Post-operative follow-up limited to an year. Patient admitted into our hospital are mostly from a rural background, with farming as occupation. Observing X-Ray, osteoporosis grading done with Singh's Index. Patients grouped into fracture neck of femur, Intertrochanteric, and Subtrochanteric fractures. Their pre-operative (mobility status before fracture), and post-operative mobility recorded. Abbreviated mental score test before surgery recorded. 4,9 Mobility assessed with New Mobility Score by M J Parker, 1995.
Table 1: Shows Assessment of New Mobility Score before Fracture. 5 Score is total 0-9
4. Mobility
No difficulty With an Aid With help of another person Not at all Able to get about the house
5. Observation and Results
The retrospective study included 50 patients treated in our hospital for proximal femur fractures, but ten people could not present for follow-up. We had complete data of 40 patients. One patient expired, during the procedure on the fracture table, during fixation. Other three patients expired during various periods of study, i.e. ; one expired due to stroke in the local hospital four months later, the other two patients expired due to post-operative complications.
In all, 20 female and 20 male patients, with an average age of 67.6 years (male-65 years and female-70.
6. H
We in our study intend to find out whether there exists any correlation between osteoporosis and pre and post-operative mobility through correlation test (Pearson test). We proposed a Null Hypothesis that there is no co-relation between these variables. On analysis, we found that these variables were related to each other. There is a positive correlation between the variables, but the intensity of the relationship between them varies as shown in table . IV.
7. Discussion
Osteoporosis, a condition which can cause disability and present a burden to already constrained health budget in developing countries, through fractures. Forget about the disability in old age due to constant osteoporotic pain; it can influence the type, and comminution of fracture, reduction and fixation during surgery, the healing time and mobilization of patients' post-operatively. 7 In the study we intend to find out whether there exists a correlation between the osteoporosis and prefracture mobility and post-operative fracture mobility of patients. We used Singh's index in the grading of osteoporosis. We used the new mobility score to determine the mobility status of patients before the fracture and post-operatively. We found there exists the correlation between these variables which is positive i.e.; those patients with good bone strength will have a better pre-operative mobility, post-operative mobility, and early return to daily activities of living.
The reasons we project or infer towards this positive co-relation are:
1. Osteoporosis will impact the fracture type (the more the osteoporotic it will be Intertrochanteric). 2. Osteoporosis will result in more comminution of fracture (more comminution of fracture fragment will result in difficulty in reduction, increase surgery time, these fragments devoid of blood supply can influence union process at a later date) 3. Osteoporosis will influence the post op mobility (comminution increases post-operative recovery, time for mobilization) 4. Fracture neck of femur operated with bipolar and THR will have good post-operative mobility than Intertrochanteric fractures.
8. Intertrochanteric fractures operated with Proximal
Femur nailing have good post-operative mobility than operated with DHS.
There is positive correlation between these variables, but intensity varies. There appears a strong relation between the pre-fracture mobility and postoperative fracture mobility followed by osteoporosis and its influence in return to daily activities of living. Per se we know the constraints of the study, a small sample size. Perhaps, an increase in the sample size can reveal the correlation in a better way. Osteoporosis influences One year mortality rate in hip fractures is about 10%-25% in various studies. 1,8 In the study we have 10% mortality i.e. ;one patient expired during the surgery and remaining three due to post-operative complications (four out of 40 patients). In our study Picture, No.4 shows that the stronger the bone, the less number of fractures can be expected i.e.
; As osteoporosis decreases the fractures also decreases.
V.
9. Conclusion
We infer that there exists a positive correlation between the osteoporosis and post-operative mobility of patients in proximal femur fractures, but also it influences the early return of daily activities of living after the surgery. Hence prevention of osteoporosis in the aging population decreases the incidence of proximal femur fractures, economic burden and disability in that particular population.
10. Bibliography

| Intensity of co-relationship | Variables | |
| Stronger | ? | Pre-operative Versus Post-operative mobility status |
| Moderate | ? | Osteoporosis Versus Time taken to return to daily activities of living |
| Weak | ? | Osteoporosis Versus Post-operative mobility |
| ? | Osteoporosis Versus Pre operative mobility | |
| Hence the null hypothesis remains rejected. | ||
| Variables | Total no: of fractures | Intertrochanteric fractures | Fracture neck of fractures |
| Osteoporosis versus pre-operative | |||
| mobility status | 0.0423 | 0.1330 | 0.0839 |
| Osteoporosis versus post-operative | |||
| mobility status | 0.1083 | 0.0193 | 0.2855 |
| Pre operative and post-operative | |||
| mobility status | 0.5107 | 0.5914 | 0.4472 |
| Osteoporosis versus time taken for | |||
| return to activities of daily living | 0.3399 | 0.4315 | 0.0238 |
| (P<0.05) |