1. Introduction
otal anomalous pulmonary venous connection is a rare heterogeneous anomaly, accounts for 1.5-3% of congenital heart diseases (1). It is characterized by abnormal return of whole pulmonary venous blood flow to the right atrium orsystemic venous tributaries due to its persistent splanchnic connection (2). A concomitant right to left shunt, commonly via an Interatrial communication, is required for survival after birth. Darling
2. classified it in four
Author ?: MD, Resident of Cardiovascular Surgery in Cardiac Surgery Hospital of Damascus University, Mouasat Square, Omar ben Abdulaziz Street, Damascus, Syria. e-mail: [email protected] Author ?: MD, Full Professor and Chief of Cardiac Surgery Department in Cardiac Surgery Hospital of Damascus University. e-mail: [email protected] categories: Supra-cardiac 45%, cardiac 25%, Infracardiac 25% and mixed type 5-10% (3). At one end of the spectrum, there are completely unobstructed circulation, these neonates present with a large left to right shunt manifestations. At the other end there are severe PVO. Neonates born with TAPVC have poor prognosis with approximately 80% mortality in the first year of life. Both obstructed and nonobstructed types of TAPV pose an absolute indication for surgical repair (4). In PVO type without intervention the median survival is two months, with the shortest survival being 1 day. Despite greatly improved neonatal care and surgical techniques over the last decade, TAPVC operation is still associated with high hospital mortality, up to 20% (5)(6).
3. II.
4. Case Presentation
A 4 -day old, low birth weight boy (w = 1950 gr) was presented to our department with discrete but increasing cyanosis, tachypnea, respiratory distress, hepatomegaly, hypoxia (SaO 2 =70%), gasping, poor feeding and severe metabolic acidosis. The prenatal course was uneventful and he was born by normal vaginal delivery on gestational age=38.5 w.
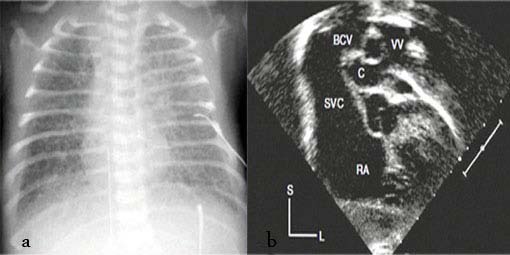
The patient didn't carry any congenital heart disease (CHD) history in his genetically close relatives (first, second and third degree). Immediate and brief work up was carried out. Chest X Ray (CXR) showed normal heart size with ground glass appearance in all the lung fields (fig. 1. a). Color Doppler and 2D-echocardiography revealed the total anomalous pulmonary venous connection (TAPVC -supra cardiac type), accompanied by significant gradient between the drainage point of vertical vein to the left brachiocephalic vein and the pulmonary veins with flow acceleration > 3.0 m/sec (pulmonary venous obstruction). It was also uncovered presence of the ASD secundum, as the natural last resort for being alive. The vertical vein was noted to be compressed as it coursed posterior the left pulmonary artery and anterior the left main bronchus (fig. 1.b). According to the aforementioned findings, the boy had almost met most of incremental risk factors leading to mortality after conventional operations.
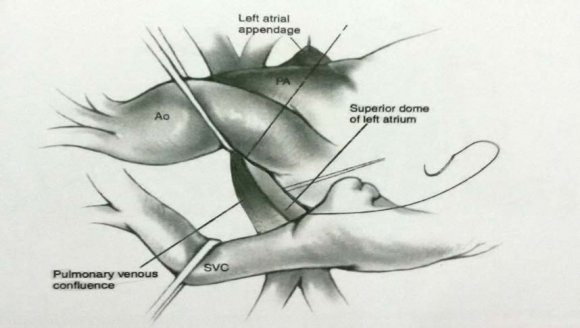
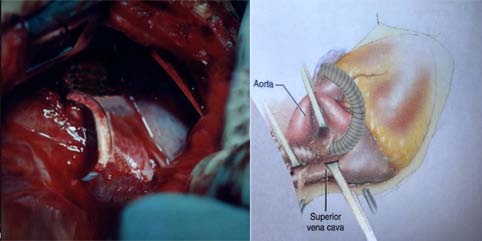
Therefore the decision was made to a new palliative surgical procedure for the first time. In order to preoperative medical stabilizing we administere 100% O 2 with the aim of promoting respiratory alkalosis as well as nitric oxide as a pulmonary vascular dilator, since the patient had severe metabolic acidosis besides Pulmonary hypertension (PHT). Under general anesthesia, median sternotomy and partial thymectomy were carried out. The pericardium was opened in vertical fashion then prudent purse-string sutures as standby were placed on ascending aorta and right atrial appendage (without using CPB). After intravenous heparinization (100 U/kg), at first some dissections were done from left lateral side between heart and pulmonary venous confluence then the dome of the left atrium was exposed. The posterior pericardium just superior the dome of LA was incised and PVC was appeared (fig. 2). Using a side -biting clamp on the PVC, a longitudinal incision was made. The proximal head of a Gore-Tex (ePTFE) with appropriate size (diameter= 6 mm) that had been prepared and beveled, was anastomosed to PVC using continuous 6-0 polypropylene suture. Under topical cooling of heart and using a side-biting clamp on left atrial appendage (LAA), the distal end of Gore-Tex was anastomosed to LAA. After deairing with heparinized saline as routine, the clamp was removed. The Sarmast-Takriti Shunt (STS) between PVC and LA was established (fig. 3). Immediately after completion of the procedure, cyanosis began to decrease. We performed the main operation 7-months later with excellent outcome when he had already sustained satisfactory weight (w= 7030 gr), as follows: After the establishment of CPB, the shunt was removed. To reduce the risk of residual obstruction of PVC due to pocket-like contraction our team preferred modified septosuperior approach (komarakshi technique). A direct anastomosis between PVC and L. A, ligation of the VV and closure of ASD with autopericardial patch were achieved in one stage repair.
5. III.
6. Results and Discussion
Evaluation of pressures before intervention in the operation room and after correction are illustrated in the (table .). Immediately after completion of surgery (STS), the pressure of PVC decreased to the point where its pressure gradient became zero. Blood oxygenation improved up to 84% (preoperative SaO 2 was 70% on 100% oxygen) and cyanosis, agitation, feeding Problem subsided. Three days later, when he was discharged, arterial oxygen saturation had reached as high as 91%. Despite good advances in treating of TAPVC in recent decades, this severe malformation in its various anatomical forms remains a challengeable entity during early infancy. Significant obstruction to pulmonary venous drainage results in pulmonary edema in the presence of a normal size and shape of the heart and cardiogenic shock which is rapidly lethal if untreated. Almost all reports have declared that perioperative high mortality associates with PVO, low weight (W<2.5-3 kg), early age (A<2m), severe preoperative acidosis, long time of Aortic Cross Clamp (ACC) and cardiac arrest. The second frontier in the treatment of TAPVC is represented by postoperative PVO. In such a difficult situations, if patients survive from operation, most of them will require multiple postoperative surgical interventions due to recurrent PVO with an increasingly poor outcomeat each representation (7). Medical efforts are minimally effective in managing the ensuing hemodynamic and metabolic problems so their use is limited to provide some short lived conservative therapy until definitive surgical treatment is carried out. PVO is usually lethal, even with reoperation and extensive attempts at revision or repair (8). This lack of success has led to alternative treatments such as balloon dilatation and stenting. The Rashkind Operation or Balloon Atrial Septostomy (BAS) has been used with some success to decompress the pulmonary venous pressure and improve C/O in the restricted ASD, but these don't appear to provide additional benefit. Moreover several reportshave proposed the use of percutaneous angioplasty and stenting of the obstructed vein to palliate shock and improve preoperative metabolic state. Research showed during the median cross -sectional follow up of 3.1 years estimated mortality was 38+/-8% at 1 year and 50+/-8% at 5-years after stent implantation.
Necessity for reintervention (owing to occlusion of stent), was 58+/-7% at 1-year. In 1996 sutureless repair technique was described, using in situ autologous pericardium for recurrent pulmonary vein stenosis following main TAPVC surgery (9). Subsequent reports emphasize the utility of this technique in selected patients as main procedure. Despite interest in the sutureless technique, there is little firm evidence that it provides a benefit over conventional techniques used a retrospective analysis to compare the outcomes of death and restenosis after conventional and sutureless techniques. By multivariable analysis, there was no statistically significant difference between the conventional and sutureless techniques. We encountered with a patient, who had almost encompassed all critical risk factors that were sufficient to make the operative prognosis very poor. We believed that Sarmast-Takriti Shunt (STS) would ensure adequate postoperative hemodynamics for symptomatic neonate and prompt left cardiac side rehabilitation. The STS with confined heparin (100U/kg), was carried out without using CPB with an intention to reduce the morbidity associated with extra corporeal circulation. Eliminating CPB reduced the cost of the procedure substantially and saved the patient from its inherent complications. (10) After procedure the enough time was prepared on behalf of the heart to compensate its chambers especially the right ventricle and left atrium and ensure endurable state for the main surgery. Although our experience was limited to STS in supracardiac type, we are optimistic and hopeful to its feasibility and usefulness in other types of TAPVC. Now, we are so satisfied owing to be able to help such a complicated neonate. Table 1: Preoperation and postoperative cardiac pressures of 4-days old male with total anomalous pulmonary venous connection accompanied by pulmonary venous obstruction.