1.
Result: Nineteen patients of distal humerus extra-articular fractures treated with distal humerus extra-articular plating were followed periodically from 6 weeks upto one year. Flexion movement was good throughout follow-up, and was statistically significant from 6 week to 3 months; 6 week to 6 months, 6 week to 1 year, 3 month to 6 months, 3 month, 1 year respectively, and was not significant at 6 month -1 year. That means the patient had almost recovered by 6 weeks follow-up; little improvement was there up to 1 year from the initial time of the follow-up. When compared with the last 6 month of follow-up, there was no further improvement possible as the patient had already achieved there anatomical range of movement. The extension was significantly improved when the patient came for follow-up at 6 weeks, and mean extension was 3.68 ± 6 degrees. Later at 3, 6 months, and 1 year where an almost normal extension was possible in all cases except complicated cases; thus there was no scope of further extension at latter visits, and test were insignificant statistically. Supination was not statistically significant at any follow-ups. That means the patient had recovered to an anatomical range of movement by 6 weeks of follow-up, and there was no further improvement possible. Pronation was not statistically significant at any follow-ups. That means the patient had recovered to an anatomical range of movement by 6 week follow-up, and there was no further improvement possible. Dash score was decreasing over one year. The score was compared at 6 weeks to 3 month, 6 month, and 1 year respectively; at 3 month to 6 month, 1 year respectively, and at 6 month to 1 year. All intervals were statistically significant (p <0.05) indicating improvement in patients daily activities to normal over 1 year. Mayo score was increasing over the period of one year. The score was compared; At 6 weeks to 3 month, 6 month, 1 year respectively; 3 month to1 year; and at 6 month to 1 year. All intervals were statistically significant (p <0.05) except at 3 month -6 month period where it was statistically insignificant due to one case of malunion, and implant failure. Otherwise, all patients recovered to almost normal over 1 year. VAS score was minimal at 6 weeks, and was decreasing at later follow-ups. It was found to be significant at 6 weeks i.e. patient were relived of pain by 6 weeks to 3 months. Later it Conclusion: Extra-articular distal humerus fractures fixed with lateral column plate resulted in good immediate stability, and fracture union with quick recovery, and improved satisfaction to the patient.
2. Introduction
istal humerus extra-articular fractures comprise 16% of humerus fractures, and 10% of distal humerus fractures (1) (2). Conventionally all distal humerus fractures are stabilized with bi-columnar plating. It is a stable fixation but requires extensive soft tissue stripping leading to delayed recovery, and Olecranon impingement as a frequent complication hampering elbow extension; without considering the damage caused by excessive soft tissue stripping, both intra-articular and extra-articular fractures are managed D was marginally significant at 6 months, but it was due to a case of implant failure that came up with aggrieved pain complaints. Otherwise; in other patient's it was insignificant after 3 months as patients were relived of pain, and there was no scope for any further pain relief. The mean metaphysealdiaphyseal angle was 86.21° (SD3.441°, normal 82-84°), the mean humeral-ulnarangle was 14.63° (SD 2.338°, normal 17.8° valgus), and the mean shaft-condylar angle was 39.84° (SD 1.500°, normal 40°). The anterior humeral line passed through 50.00 % (SD 1.491 %) of the capitellar width (normal, middle third). One patient had implant failure, which was treated by implant exit, and revision lateral column distal humerus plating.
in the same way. In extra-articular distal humerus fractures it's not needed, and additional soft tissue stripping, olecranon impingement or need of olecranon osteotomy is eliminated by using single lateral column plate (1) (3) (4) (5) (6). With recent advances in the field of implant manufacturing, and their availability: single column plate with better strength and designs are promising enough to provide equivalent fracture stabilization (7) (8), avoids olecranon impingement/ osteotomy; with less surgical exposure, thereby helping in quicker recovery, and reduced rehabilitation time. Lateral column plating in extra-articular distal humerus fractures, is a surgical procedure in which fracture is reduced by open anatomical reduction, and fixed with single lateral plate to posterior surface of humerus to restore mechanical axis, stability of the bone and restore joint configuration (3) which will further enhance the function of the muscles, ligaments , and other soft tissue structures of the elbow joint with minimal soft tissue stripping, completely eliminating olecranon impingement, and thus aid in early mobilisation.
3. II.
4. Material & Methods
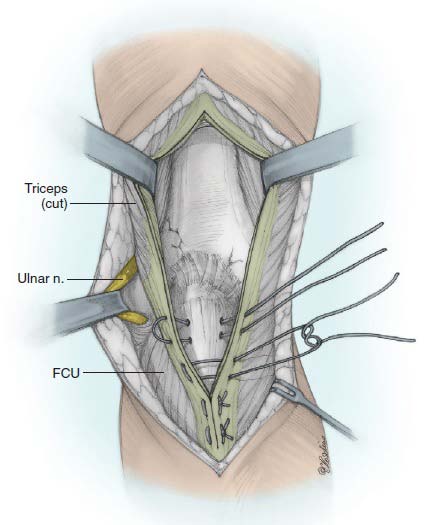
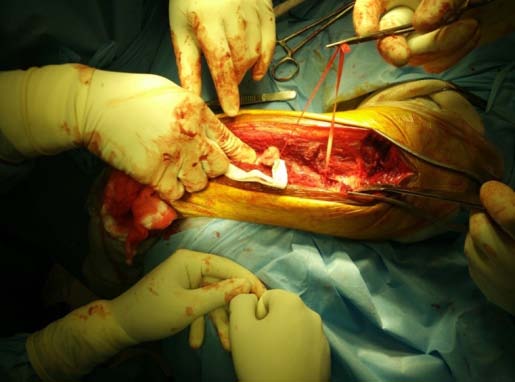
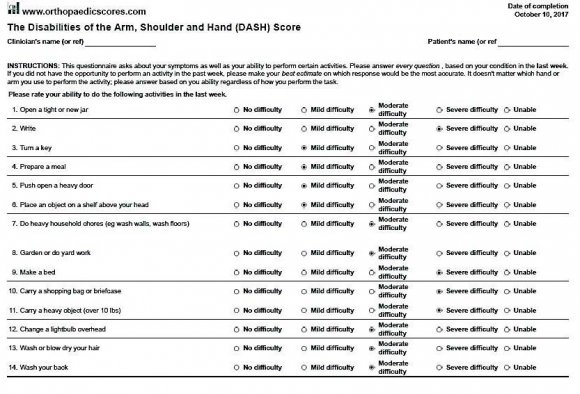
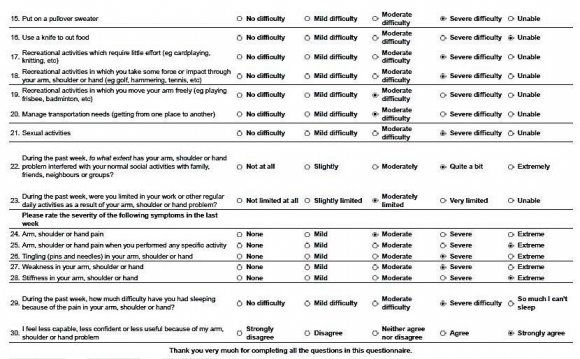
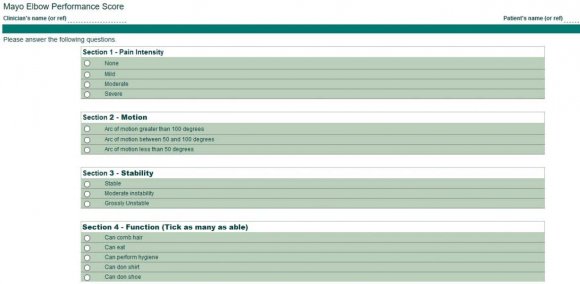
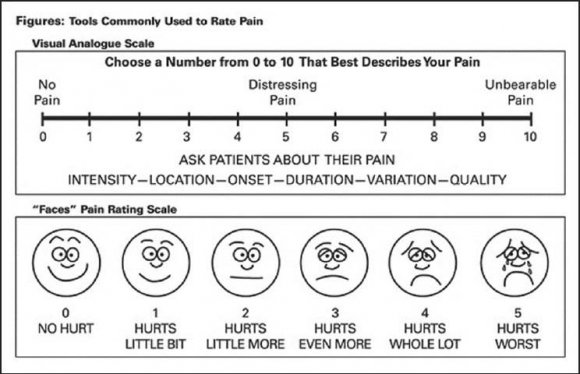
It was a Prospective study conducted at Sri Ramachandra Medical College & Research Institute, Chennai during April 2015 and August 2017. The study consisted patients of closed injury with distal humerus extra-articular fractures in skeletally mature patients, and excluded intra-articular fractures of elbow, paediatric age group, proximal humerus fractures, previouslytreated or operated with other internal fixation methods/devices but failed, open injuries, and patients having a pre-operative neuro-vascular deficit. Preoperatively patients were evaluated clinically, radiologically and the diagnosis was established and classified using the AO/ASIF Classification. Twenty (20) patients of distal humerus extra-articular fractures were at hand of which Nineteen (19) were available for final assessment. Our follow-up period ranges from 6 weeks to 1 year. The Implant used was LCP Extra-articular Distal Humerus Plate, which is anatomically shaped, and angular stable fixation system for extra-articular fractures fixation of the distal humerus. The LCP head is tapered to minimize soft tissue irritation; five distal locking holes accept 3.5 mm locking screws, all head holes are angled medially to maximize screw purchase in bone, two most distal holes are angled toward the capitulum, and trochlea. whereas in the Plate shaft Combi holes combine a dynamic compression unit (DCU) hole with a locking screw hole, providing the flexibility of axial compression, and locking capability throughout the plate shaft, Limited-contact design, Available with 4, 6, 8, 10, 12 or 14 elongated Combi holes to accommodate distal humerus fractures with shaft involvement (figure 1) The patient is nursed in absolute aseptic conditions in the postoperative ward with the limb in hanging position by pillow cover elevation. Parental antibiotics were continued for the first two days followed by oral antibiotics for the next three days. Pain management was done with intra-venous analgesic, and was removed on the 2 nd post-operative day. There after oral analgesics were given. Drain is removed at the end of 48 hrs. As soon as pain subsides, Rehabilitation Protocol is started with physiotherapy. The Active elbow flexion-extension and supination-pronation exercises with the aim of maximum ranges of motion; as soon as possible but as tolerated by the patients. The patient was advised to continue exercises here or any other convenient centre. Sutures were removed during 12 th to 14 th post-operative day. After the surgery, functional evaluation was done with DASH, MAYO and VAS score (figure 3, 4, and 5) at six weeks, three months, six months, and one year.
5. Results
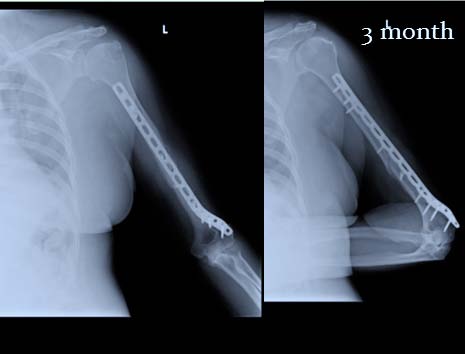
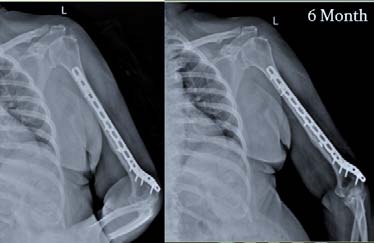
6. Figure 7
Road traffic accident was the major cause of injury 63.2%; followed by slip and fall 26.3%, one case of pathological (5.3%), and sports injury (5.3%) each. The mean metaphyseal-diaphyseal angle was 86.21° (SD3.441°, normal 82-84°), the mean humeralulnar angle was 14.63° (SD 2.338°, normal 17.8° valgus), and the mean shaft-condylar angle was 39.84° (SD 1.500°, normal 40°). The anterior humeral line passed through 50.00 % (SD 1.491 %) of the capitellar width (normal, middle third). Flexion movement was good throughout followup, and was statistically significant from 6 weeks to 3 month; 6 week to 6 month, 6 week to 1 year, 3 month to 6 month, 3 month, 1 year respectively, and was not significant at 6 month -1 year. That means patient had almost recovered by 6 week follow-up, little improvement was there up to 1 year from initial time of follow-up. When compared with last 6 month of followup there was no further improvement possible as patient had already achieved there anatomical range of movement (Figure 10). The extension was significantly improved when the patient came for follow-up at 6 weeks, and mean extension was 3.68 ± 6 degrees. Later at 3, 6 months and 1 year where almost normal extension was possible in all cases except complicated cases; thus there was no scope of further extension at latter visits, and test were insignificant statistically (Figure 11). Supination was not statistically significant at any follow-ups. That means the patient had recovered to an anatomical range of movement by 6 week of followup, and there was no further improvement possible (Figure 12). Pronation was not statistically significant at any follow-ups. That means the patient had recovered to the anatomical range of movement by 6 week follow-up, and there was no further improvement possible (Figure 13). Dash score was decreasing over one year. The Score was compared at 6 weeks to 3 month, 6 month, and 1 year respectively; at 3 month to 6 month, 1 year respectively, and at 6 month to 1 year. All intervals were statistically significant (p<0.05) indicating improvement in patients daily activities to normal over 1 year (Figure 14). Mayo score was increasing over a period of one year. The score was compared; At 6 weeks to 3 month, 6 month, 1 year respectively; 3 month to 1 year;, and at 6 month to 1 year. All interval were statistically significant (p <0.05) except at 3 month -6 month period where it was statistically insignificant due to one case of malunion, and implant failure. Otherwise, all patients recovered to almost normal over 1 year (Figure 15). VAS score was minimal at 6 weeks, and was decreasing at later follow-ups. It was found to be significant at 6 weeks i.e. patient were relived of pain by 6 weeks to 3 months. Later it was marginally significant at 6 months but it was due to case of implant failure that came up with aggrieved pain complaints. Otherwise; in other patient's it was insignificant after 3 months as patients were relived of pain, and there was no scope for any further pain relief (Figure 16).
7. b) Complications
Malunion (Cubitus varus) was seen as the most frequent complication 15.8% of the study group. Infection (CDC Superficial) and Elbow stiffness were seen in 10.5% which was second most frequent complication noticed. Delayed union and implant failure was seen in 1 case (5.3%) each. One infected patient, after getting completely treated for infection, had implant pulled out at 6 months review also she had associated varus deformity , and elbow stiffness. The patient was not willing for deformity correction. She was managed with bursa excision, wound debridement and implant exit followed by antibiotics and regular dressing. One patient had delayed union and associated elbow stiffness; post 6 months fracture healed well. No intervention was done as the patient was unwilling. Only calcium, multi-vitamin supplementation, and supervised exercises were given. One patient with varus malunion had a postoperative superficial infection which was managed with regular dressing and antibiotics. Another varus malunion had no associated complication. Both malunion did not require any intervention as it did not deteriorate any function, and patients were satisfied without come.
Fractures: None of the patients had peri-prosthetic fracture during the follow-up.
Heterotrophic ossification: None of the patients had heterotrophic ossification during the follow-up. Neurovascular Injury: None of our patients had a neurovascular injury (Figure 17).
8. Discussion
These fractures are closely associated with elbow function and its stability (7) (9), the elbow range of movement is essential for most daily activities indicating its earliest surgical fixation to restore the anatomical and functional integrity, and prevent both structural as well as neurovascular complications (3) (10) (11) 11) conducted a study on distal third humerus fractures treated using the Synthes 3.5-mmextra-articular distal humeral locking compression plate where the mean VAS score was 8.5. In the study conducted by John T Capo (1) there were 47% patients who had VAS score of 0 i.e. no pain,17% patients had score of 1-3 i.e. Mild pain,17% patients had score of 4-6 i.e. moderate pain, , and score of 7-10 in 0% patients i.e. severe pain. In our study VAS score was minimal by six weeks, and was further decreasing; Similarly Supination/pronation was evaluated at 6 weeks and at later follow-up, and it was found that complete anatomical restoration of movement was achieved by 6 week itself, and no further benefit was possible at later follow-ups. Other researchers also had observed similar values in their observation. John T capo et al. ( 1) observed supination 83 ± 22 °at 3 months where as it was 82 in Rajendraprasad Butala et al. ( 13) 6 months, and Yatinder kharbanda (12) got value of 84.5 °at the end of 1 year which is within normal range of movement. In our study Supination was 83.42±1.539 °at 6 week, 83.61±2.304 °at 3 month, 84.00±1.455 °at 6 month, and 84.00±1.455 °at 1 year, and was statistically insignificant. I.e. Range of movement was recovered to full before 6 weeks, and no further improvement was possible beyond it. Pronation 82 ± 23 °was reported by john T capo et al. ( 1) at 3 month where as it was 85 °in Rajendraprasad Butala et al. ( 13) study, and Yatinder kharbanda (12) 83.75 °at one year. In our study it was 78.16 ± 3.420 °at 6 weeks, 78.68 ± 2.810 °at 3 months, 78.06 ± 2.508 °at 6 months, and 79.17± 3.536 °at 1 year. Statistically, it was insignificant indicating it was functionally recovered before 6 weeks, and there was no further scope of improvement. Thus indicating supination and pronation movement were not affected primarily due to these fractures. Difficulty in supination pronation was due to surrounding soft tissue pain. Once the patient was pain free this movement had come back to normal (Table 3). Outcomes of Lateral Column Plating in Extra-Articular Distal Humerus Fracture At 6 week mean VAS was 1.16±2.062, at 3 month. 37±1.012, 1 year. 21±.918, except at 6 months where it was increased (.42±1.017) due to implant failure that came up with aggrieved pain complaints. The score was compared from 6 weeks to 3 months (and later); At 6 weeks-3 month it was statistically significant (p =0.05); marginally significant (p=0.58) at 6 weeks-1 year due to a case of implant failure. Otherwise, in other patient's it was insignificant at 6 weeks-6 month; 3 month -6 months, 1 year; at 6 months to 1 year. Indicating patients were relived of pain by 6 weeks, and there was no further scope of pain relief (Table 4). 15) Functional outcome of extra-articular distal humerus fracture fixation using a single locking plate elbow function was assessed by Mayo score at final follow-up, and was 90.8 -9.9 they concluded Stable reconstruction, and early initiation of physiotherapy are utilitarian to envision optimal outcome; the use of pre-contoured extra-articular distal humerus locking plates has yielded satisfactory results which were comparable to our study where mayo elbow score was 100. It was progressively increasing at follows up suggesting significant improvement at each followup. Similarly, in Deepak Jain et al. (16) prospective study of 26 patients The MEPS (average: 96.1; range 80-100) was excellent in 81% cases (n = 21), and good in 19% cases (n =5). There were 2 cases followed up to 1 year average MEPS was 90. Rajendraprasad Butala (17) mentioned MEPS score of 95.5 at 6 month, which is excellent outcomes, and is comparable to our study. In our study Mayo score was found to be increasing over a period of one year; at 6 weeks it was 88.74 ± 11.464, at 3 months 94.11 ± 7.752, at 6 month 96.39 ± 5.893, and at 1 year it was 100.00 ±.000. The score was compared 6 weeks to 3 months (and later); At 6 weeks-3 month, 6 month, 3 month -1 year; 6 month-1 year; , and at 6 month to 1 year. All interval were statistically significant (p <0.05) except at 3 month -6 month period where it was statistically insignificant. This was due to one patient who came back during this period with malunion, and implant failure. That means the patient's recovered to almost normal over 1 year. Single column plate has proved promising enough to provide equivalent fracture stabilization, eliminates olecranon impingement/ osteotomy, with less surgical exposure due to good implant strength, and designs , and is thereby helping the patients to quick return to their normal lifestyle (Table 6). 9) conducted a retrospective study on distal humerus fractures in elderly patients: results after open reduction, and internal fixation consisting of 45 patients whose clinical, and radiological follow-up was obtained after a minimum of 24 months following surgery (median 87 months; range, 24-121 months). Functional results were evaluated according to the Mayo Elbow Score. Open reduction, and internal fixation of distal humerus fractures in elderly patients should be the main goal, since good elbow function can be achieved in the majority of patients. Elbow immobilization longer than 14 days should be avoided. Stable implant anchorage at the lateral column remains problematic, reflecting a general potential for further implant improvements.
V.
9. Conclusion
Single-lateral column plating technique was a useful treatment option in the management of extraarticular distal humeral fracture. It addresses the difficulties encountered while managing these fractures, and provides predictable and satisfactory results. The plate matches the anatomic contour of the distal humerus, and does not impinge on the olecranon fossa, thus eliminates the need for olecranon osteotomy. It is low profile over the lateral column, and provides adequate stability leading to faster recovery. This technique can be safely performed using the Campbell's posterior triceps-splitting approach, which was associated with no iatrogenic radial or ulnar nerve palsies, and with less surgical exposure thus helping in quicker recovery, and reduced rehabilitation time. Early range of motion was probably the most important advantage of this technique. Full range of movements is observed by the first 6 weeks. But, patient's achieve a good functional score, recover to normal, and attain complete satisfaction over 1 year. The objective functional and radiological outcomes documented in our study were excellent, and impact of complications on the final functional outcomes was limited despite the minimal risk of postoperative varus deformity which primarily is a cosmetic deformity; as elbow had a full range of motion with no functional abnormality. Superficial infection was present in some patients, and we assume it was due to instant mobilization, and return into routine life, where wound care was neglected. Introduction of an early rehabilitation program along with the emphasis on the early use of the elbow and wound care, could improve the functional success of this technique.


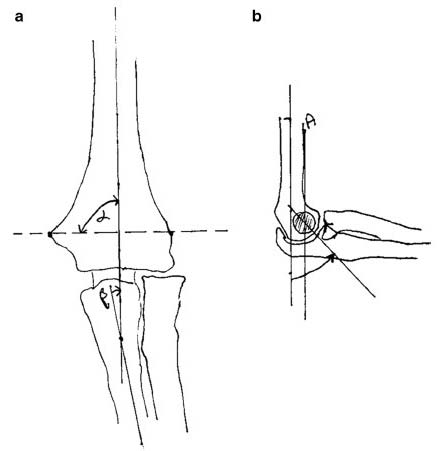


| N | Minimum | Maximum | Mean | Std. Deviation | |
| Metaphyseal diphyseal angle | 19 | 82 | 91 | 86.21 | 3.441 |
| Humeral ulnar angle | 19 | 12 | 18 | 14.63 | 2.338 |
| Shaft condylar angles | 19 | 38 | 42 | 39.84 | 1.500 |
| Anterior humeral line | 19 | 48 | 52 | 50.00 | 1.491 |
| D D D D ) |
| ( |
| Elbow ROM | John T. Capo et al (post op) | Yatinder Kharbanda et al | Gregory M. Meloy (At 4 month) | Rajendraprasad bhutala et al | Our Study | |||
| Flexion (mean) | 138.74 ± 8.685 | °Extension | ||||||
| 6 week | ||||||||
| (mean) | 3.68 ±6.634 | °3 | ||||||
| Flexion (mean) | 136.1 +7.78 °141.67 ± 4.201°E | |||||||
| months | ||||||||
| xtension (mean) | 3.62+4.96 °1.11 ± 3.234 | °6 | ||||||
| Flexion (mean) | 128 °144.44 ± 1.617 | °Extension | ||||||
| months | ||||||||
| (mean) | 0 °; 3 cases ffd of 10 °.00 | °1 | ||||||
| Flexion (mean) | 126±16°125 °145.00 ± .000 | °Extension | ||||||
| year | ||||||||
| (mean) | -7 ± 7 °0 °.00 | °Table | ||||||
| 3 | ||||||||
| Supination | John T. Capo et al | Yatinder Kharbanda et al | Rajendraprasad butala et al | Our Study | ||||
| 6 week | - | 83.42 ± 1.539 | °3 | |||||
| months | 83±22°83.61 ± 2.304 | °6 | ||||||
| months | 82 °84.00 ± 1.455 | °1 | ||||||
| year | 84.5 °84.00 ± 1.455 | °Pronation | ||||||
| John T. Capo et al Rajendraprasad butala et al | Yatinder Kharbanda et al | Our Study | ||||||
| 6 week | - | 78.16 ± 3.420 | °3 | |||||
| months | 82±23°78.68 ± 2.810 | °6 | ||||||
| months | 85 °78.06 ± 2.508 | °1 | ||||||
| year | 83.75 °79.17 ± 3.536 | °Hassan | ||||||
| Fawi et al. ( | ||||||||
| Hassan Fawi et al | John T Capo et al | Our Study | ||
| 0 None 47% | 6 week 1.16 ±2.062 | |||
| VAS | 1-3 Mild 17% | 3 month .37±1.012 | ||
| (mean) | 8.5 | 4-6 Moderate 17% | 6 month .42±1.017 | |
| 7-10 severe 0% | 1 year .21±.918 | |||
| Table 5 | ||||
| DASH | John T. Capo et al | Yatinder Kharbanda et al | Our Study | |
| 6 week | - | 40.72+5.498 | ||
| 3 months | 25.8±17.7 | 33.81+5.522 | ||
| 6 months | 30.51+4.447 | |||
| 1 year | 17.6 (13.3-38.3) | 15.82+4.450 | ||
| Vivek Trikha et al. ( | ||||
| Outcomes of Lateral Column Plating in Extra-Articular Distal Humerus Fracture |
| Volume XIX Issue II Version I |
| D D D D ) H |
| ( |
| Medical Research |
| © 2019 Global Journals |
| Mayo | Vivek Trikha et al | Deepak jain et al Rajendraprasad butala et al | Our Study | |
| 6 weeks | - | 88.74 ± 11.464 | ||
| 3 months | - | 94.11 ± 7.752 | ||
| 6 months | - | 96.66 | 95.5 | 96.39 ± 5.893 |
| 1 year | 90.8 ± 9.9 | 90 | 100.00 ± .000 | |
| Korner J et al. ( | ||||