1. Introduction
eripartum Cardiomyopathy (PPCM) is an idiopathic cardiomyopathy that presents in the last month of pregnancy up to five months of delivery as heart failure secondary to left ventricular systolic dysfunction in the absence of another cause of heart failure. 1 It was first described as early as 1800, yet its aetiology is still unclear. 2 The incidence of PPCM varies in different population. It has been reported to occur in varying rates ranging from 1 in 15,000 in United states to 1 in 100 in a small region in Sub-Saharan Africa. 3 Incidence in India has not been reported.
We present a case series report of eight cases reported in our hospital over a time span of two years.
2. II.
3. Materials and Methods
A retrospective study was done at Rajiv Gandhi Government Women and Children Hospital, Pondicherry from 2017-2018. Files of the patients diagnosed with PPCM were reviewed and analysed.
The definition criteria 4 used for PPCM included:
? Heart failure in the last month of pregnancy and up to five months postpartum ? Absence of identifiable causes of heart failure ? Absence of recognisable heart failure before last month of pregnancy.
Clinical data of the patients including the age, parity, gestational age, identifiable risk factors and clinical presentation were noted. ECHO findings were noted. Treatment given to the various patients in form of diuretics, ion tropes and ventilatory support were compared. The patients were then followed up and echocardiography was repeated after 6 months of delivery and the findings were noted.
4. III.
5. Results
The demographic details, clinical presentation and management of the patients included in our study were analysed. It was observed that the mean age of incidence among the patients was 28+/-2 years.
The incidence of Peripartum Cardiomyopathy among primiparous was 50% (n=4) showing that there was equal distribution of PPCM among primi and multiparous women.
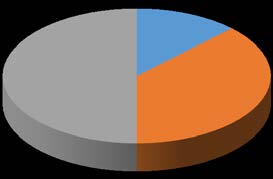
? Additional criteria included left ventricular systolic dysfunction characterised by echocardiogram finding such as depressed shortening fraction (< 30%), ejection fraction(less than 45%) and a left ventricular end diastolic dimension of more than 2.7cm/m 2 of body surface area. As seen in the pie diagram, it is evident that the incidence of Gestational diabetes (GDM) among patients with PPCM was 62% (n=5) of cases. The other risk factors observed were anemia, multiple pregnancy and gestational hypertension each contributing to 13% of the cases.
All the patients had an acute onset of symptoms with the peak incidence being within 24 hours of delivery amounting to 37.5% (n=3) of the cases. Only one patient presented in the antenatal period. The diagnosis was based on ECHO finding showing a fall in ejection fraction below 45%. Significant mitral regurgitation was noted in half the cases. The treatment given was mainly supportive which included ventilator support, ion tropes and diuretics. Ventilator support was needed in three out of eight cases.
The patients were followed up to six months postpartum. ECHO was repeated for all the patients and was compared with the initial ECHO findings.
5, 62% 1, 12% 1, 13% 1, 13%6. DISTRIBUTION OF RISK FACTORS(n=8)
GDM anemia multiple pregn GHT It was observed that 50% (n=4) of the patients had an initial ejection fraction of 35% and 38% (n=3) of the patients had an initial ejection fraction of 30%. Only one patient had an ejection fraction of 20% which was the only case that eventually culminated in maternal mortality.
On follow-up ECHO, it was noted that 7 among 8 patients (85%) had an ejection fraction of >45% and only one patient had an ejection fraction of 35%. It was noted that the patient with follow up ejection fraction 35% had an initial ejection fraction of 30%.This highlights the importance of initial ejection fraction showing that patients with better ejection fraction at the initial presentation recovered well. As the rate of recurrence in subsequent pregnancy is high, we advised the patients to avoid further conception.
IV.
7. Discussion
The mean age of incidence of PPCM in our present study was 28+/-2 years. Similarly, in a study conducted by Amos 5 et al the mean age of incidence was 29 years. Chapa 6 et al and Vettori 7 et al also reported a lower age of incidence of 27 years. Elakayam 8 et al reported a mean age of 29 years. In a study conducted by Kolte 9 et al, it was noted that the mean age of incidence was higher averaging 30.8+/-7.1 years. Similarly a study conducted by Hasan 10 et al also showed a higher age of incidence amounting to 32 years. Asad 11 et al reported a mean age of 27-32 years.
8. Table 1: Mean age of incidence of PPCM in various studies
In our study, there was equal distribution among primiparous and multiparous women. This is in contrast with many studies including Fett 12 et al who in their study on the incidence of peripartum cardiomyopathy had concluded that there was an increase in the incidence of PPCM with increasing age and increasing parity.
On analysing the risk factor profile of the patients, it was observed that in our study the incidence of Gestational Hypertension was 13% (Fig 1). Chapa 6 et al reported a low incidence of 16% in their study. Kolte 9 et al reported a higher incidence of 59.6% in their study. Similarly, Vettori 7 et al (50%), Amos 5 et al (45%) and Elakayam 8 et al (43%) also reported a high incidence of Gestational Hypertension among patients with PPCM. In our study, Gestational Diabetes was a major contributor amounting to 62% of cases as shown in figure 1. In study conducted by Kolte 9 et al, a lesser incidence of GDM among patients with PPCM amounting to 18.2%.
The incidence of multiple pregnancy in patients with PPCM was 13% in our present study (Fig 1 ). A similar incidence rate of 13% was reported in studies conducted by Chapa 6 et al and Elakayam 8 et al. A slightly higher rate of 17% was reported in a study conducted by Vettori 7 et al. In a study conducted by Kolte 9 et al, it was noted that the incidence of multiple pregnancy in patients with PPCM was 6.2%.
In our present study, the incidence of anaemia among patients with PPCM was 12%. A higher rate of 30.5% was reported in a study conducted by Kolte 9 et al. The variation in the distribution of risk factors among patients with PPCM can be explained by the fact that our study was conducted in Southern India while other studies were conducted elsewhere.
In our present study, the diagnosis was made within 24 hours of delivery in 37.5% of cases (Fig 2). This correlates with the finding of the study by GowriSayi Prasad 13 et al who found out that 11 out of 16 cases in their study presented in the first postnatal day.
V.
9. Add on Points on PPCM
Peripartum Cardiomyopathy is a rare condition recently on raising incidence with high maternal mortality and morbidity 14 . The incidence varies widely in different population.
It is characterised by left ventricular systolic dysfunction occurring in the last months of pregnancy or in the post natal period in the absence of other causes of heart failure. The aetiology is still unclear and many theories have been postulated. Genetic basis for the diseases has been proposed in several studies 15 .
The diagnosis is based on clinical suspicion and echocardiogram. The main drawback in the diagnosis is that symptoms of heart failure may be confused with the symptoms of normal pregnancy which may cause a delay in diagnosis and hence a delay in the start of treatment. The Centre for Maternal and Child Enquiries has suggested that " women in late pregnancy or within 6 months of delivery with symptoms of breathlessness, orthopnea, and signs of tachycardia and tachypnea may have PPCM and investigation with chest X-ray and echocardiogram are indicated" 16 .
The management of patients with PPCM should be individualised. Management strategies should be dictated as to the fact whether the patient is pregnant or post partum as certain drugs are to be avoided in pregnant women 17 . Beta blockers can be used safely in pregnancy, while ACE inhibitors, ARB and aldosterone antagonist should be avoided. Diuretics should be used in caution as it can affect uteroplacental circulation.
Bromocriptine may be a novel disease-specific treatment for PPCM 18 .Several case reports have suggested that the addition of bromocriptine to standard therapy for HF may be beneficial in patients with acute onset of PPCM. In addition, a proof-of-concept randomized pilot study of patients with newly diagnosed PPCM presenting within 4 weeks of delivery also showed promising results. Patients receiving bromocriptine 2.5 mg twice daily for 2 weeks, followed by 2.5 mg daily for 4 weeks, displayed greater recovery of LVEF compared with patients assigned to standard care. However, the use of bromocriptine has been found to be associated with incidence of acute myocardial infarction 19 . Hence it should be used with anti coagulants.
Women with PPCM should have a multispeciality care. Unless there is deteriotion in maternal condition, there is no need for urgent delivery 20 . The primary consideration is maternal hemodynamic stability. Labour natural is the preferred mode of delivery 21 . Continuous electronic foetal monitoring is recommended. Left lateral position of the mother is preferred to prevent supine hypotension 22 . Epidural analgesia should be administered 20 . During caesarean section, spinal or combined epidural-spinal anaesthesia is preferred. Second stage of labour should be cut short. Active management of third stage of labour is a must. Breast feeding is not advised as prolactin sub fragments are suspected to have a role in PPCM.
PPCM is known to have high maternal mortality, ranging from 15-50% 3 . Timely diagnosis and critical care support has found to reduce the mortality rate.
Elkayam 8 et al studied 44 women with PPCM and a subsequent pregnancy and found that LVEF increased after the index pregnancy but decreased again during the subsequent pregnancy, irrespective of earlier values. Development of HF symptoms was more frequent in the group where LEVF had not normalized before the subsequent pregnancy. Hence patients with PPCM in index pregnancy should be properly counselled and should have an ECHO done before the next pregnancy.
10. Upcoming researches on PPCM
A genomic association has been proposed as aetiology for PPCM. There has been shown to be a familial concordance of PPCM, however it can be a simple presentation of familial dilated cardiomyopathy 15 . There has been a proposal of association between gene 12 and incidence of PPCM 23 .
A study conducted on mice has shown that prolactin cleavage causes impairment of cardio myocyte function due to anti-angiogenic and pro-apoptotic properties. This effect has been showed to be completely reversed by administration of bromocriptine. This finding may hold therapeutic promise in humans. 24 Antibodies directed against cardiac tissues have been found in PPCM patients, though it remains unclear whether it is a causative factor or it occurs after destruction of myocytes by another mechanism 25 .
11. VI.
12. Conclusion
Peripartum cardiomyopathy is a rare entity but has high mortality rates. Hence cases presenting with features of heart failure should be treated with high suspicion. Prompt diagnosis and treatment is crucial for a better outcome. Proper counselling should be given to the patients regarding subsequent pregnancy.
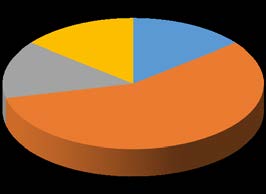
| INTIAL ECHO | POST NATAL ECHO | |||
| PRESENTATION-Ejection fraction % | PRESENTATION-Ejection fraction% | |||
| 1, 12% | ||||
| 1, 14% | 1, 15% | |||
| 4, 50% | 1, 14% | |||
| 3, 38% | 4, 57% | |||
| 20 30 35 | 35 45 50 58 | Year | ||
| 11 | ||||
| Study Present study Amos 5 et al Chapa 6 et al Vettori 7 et al Elakayam 8 et al Kolte 9 et al | Mean Age of Incidence of Ppcm in Years 28+/-2 29 27 27 29 30.8+/-7.1 | Volume XX Issue I Version I | ||
| Hasan 10 et al | 32 | D D D E D ) | ||
| ( | ||||
| Medical Research | ||||
| Global Journal of | ||||
| Study | Incidence of GHT in Patients with PPCM in Percentage | |||
| Present | 13% | |||
| Chapa 6 et al | 16% | |||
| Kolte 9 et al | 59.6% | |||
| Vettori 7 et al | 50% | |||
| Amos 5 et al | 45% | |||
| Elakayam 8 et al | 43% | |||
| © 2020 Global Journals | ||||