1.
treatments like growth modification 3 and surgery for correction of jaw deformities. 4 However, most studies evaluating the airway have been conducted with twodimensional (2D) cephalograms, providing limited data such as linear and angular measurements, for a complex three-dimensional (3D) structure. 5,6 Contemporarily, the lateral cephalograms still seem to be the dominating evaluation tool in the field of upper airway research inspite of its disadvantages. The main drawback, without any doubt, is considered as the degradation of a three-dimensional (3D) entity into two dimensions. With the introduction of CBCT, shortcomings of lateral cephalograms have been overcome. 7,8 Despite the widespread use of CT examinations in clinical practice, this new technology brought along concerns about the exposure to ionizing radiation and its potential hazards. Therefore, radiation dose and strategies for dose reduction, especially for younger patients, have become an important focus of interest.
With the advent of Cone Beam Computed Tomography, lower radiation doses and faster image acquisition times have become possible when compared with conventional computed tomography scans. 9,10 Also the three-dimensional diagnosis of the airway is more reliable with the Cone Beam Computed Tomography with the reduced radiation dose. 11 The isolation of the hard and soft tissue structures based on the variations in their densities is apparent in a CBCT image, which allows the segmentation and visualization of hollow structures such as the airway, and the analysis of the airway volume are easy with the use of appropriate software.
Previous studies have reported that patients with skeletal class II malocclusion with mandibular retrognathism had a reduced pharyngeal airway space. 12 Mandibular advancement surgery has been advocated as a treatment option for skeletal retrognathism, which has a strong influence on the airway post-surgically. Several studies have reported regarding the Pharyngeal Airway Space (PAS) changes two-dimensionally using lateral cephalograms after I. Introduction he upper airway has long been an area of interest in orthodontics, with topics such as the relationships between facial type and airway, 1 airway shape and volume with growth and development 2 and the clinician's potential to modify the airway through T surgical procedures. 5,6 The purpose of this study is to evaluate the airway volumetric after mandibular advancement surgery using 3D CBCT techniques.
2. II. Materials and Methods
The study protocol was reviewed and approved by 'The Institutional Ethics Committee of Meenakshi Academy of Higher Education and Research, Meenakshi University' with the Ref MAHER/COE -250/2014. Before the CBCT scan, the patients were fully informed about the purpose of this study and the radiation risks associated with the scan. All the patients included in this study were from the department of orthodontics, meenakshi ammal dental college and hospital who have reported for orthodontic treatment. Seven patients, who were advised for mandibular advancement surgery using Bilateral Sagittal Split Osteotomy, were selected for this study. The 3D-CBCT was acquired using Planmeca ProFacecone beam 3D imaging system (Planmeca, Helsinki, Finland). The pre-surgical 3D-CBCT was taken within a week before the surgery. The post-surgical 3D-CBCT was taken three months following the Bi-Lateral Sagittal Split Osteotomy. The surgery performed on the patients involved advancement of the mandible, with a mean of 4mm, in the anterior-posterior direction. Rigid fixation was done using mini-plates and screws.
3. Inclusion Criteria
All subjects were examined and oriented to have their heads positioned with the Frankfort horizontal plane parallel to the floor with maximum intercuspation. The whole maxillo-facial complex, (extending from the vault of the skull superiorly, till the level of the thyroid cartilage) was scanned with the Planmeca ProFace Cone-Beam 3D imaging system. With the exposure time of about 14 seconds, the 3D images acquired were reconstructed with 400 microns isometric voxel size, with the tube voltage of about 90 kV and 9mA tube current. Images were examined with the scanner´s proprietary software ROMEXIS (Version 3.0.2.R).
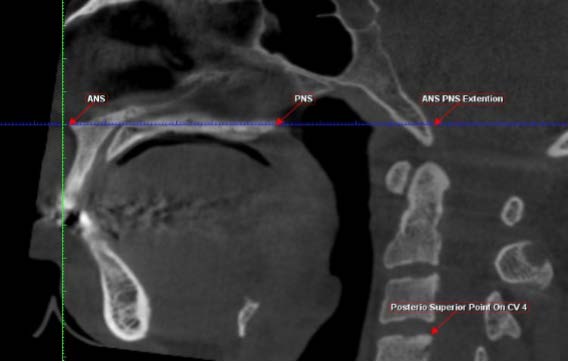
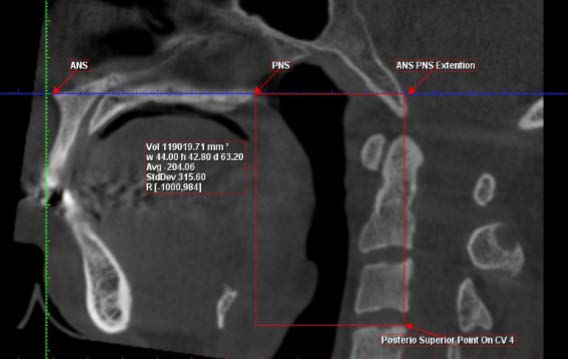
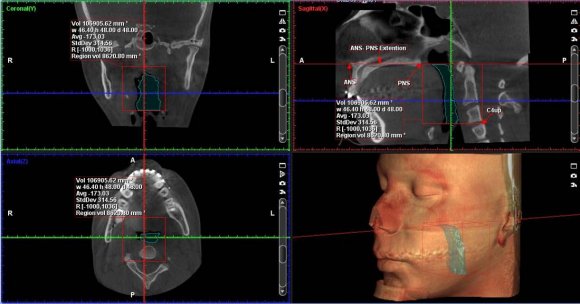
In the explorer view of the software, the image in the coronal section was oriented so that the sagittal slicing plane (Red line) passes through the anterior nasal spine (ANS). This will help to obtain the particular sagittal section which passes exactly through the midsagittal plane. In the sagittal section of the image, the following landmarks were marked (Figure : 1) Then the sagittal image is rotated so that the palatal plane (ANS-PNS) is parallel to that of the axial slicing plane (Blue Line). Since the airway is not bounded fully with hard tissue structures, the anterior and superior boundary is located at the PNS point and the posterior and inferior boundary is located at the C4up point as it corresponds to the deepest point of the vallecula. Taking these landmarks as reference, the external volume of the airway is drawn using a tool provided by the software.
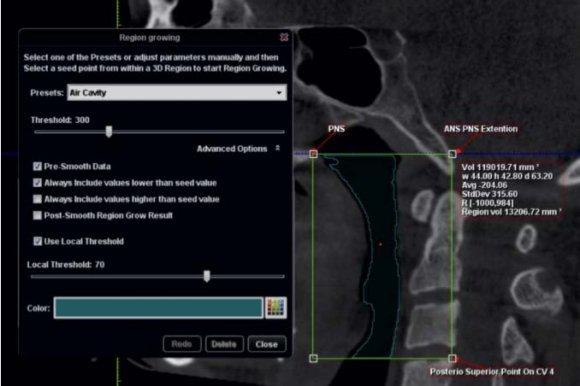
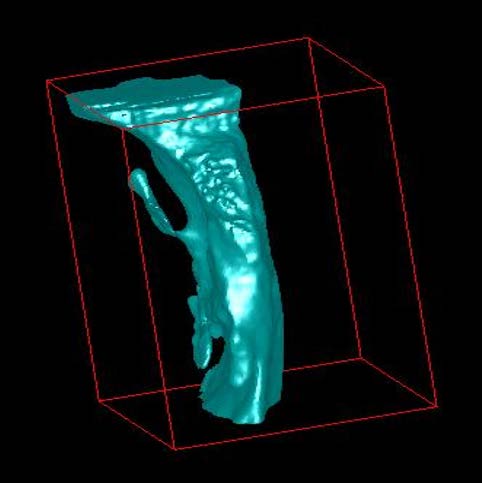
The airway could be isolated after demarking the total volume of interest required for the study. The ROMEXIS software automatically created the third dimension based on the height and the width of the region marked in the two-dimensional view (Figure : 2). Using the 3D region growing tool, the 'air cavity' was selected from the pre-sets. A local threshold level of 70 was used and the particular area of interest in the airway region was selected. This procedure was carried out by a single operator (S.K) to create and measure the rendered volumes. For reliability purpose, it was repeated by the same operator after a period of two weeks and finally, the average is taken for the calculation.
Descriptive statistics including the mean, and standard deviation for each group were calculated by using SPSS (version 20.0). The Normality test, Kolmogorov-Smirnov and Shapiro Wilk tests results showed that all the variables followed the normal distribution and therefore the parametric test was applied to analyze the data. To compare the mean values between the pre-surgical and post-surgical Pharyngeal Airway Space (PAS) volume paired t-test was applied. A p-Value < 0.05 level of significance was used for the test.
4. III. Results
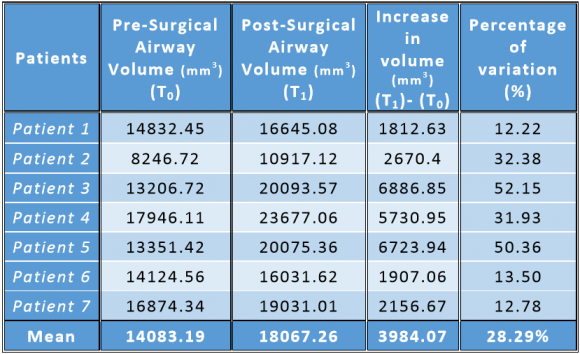
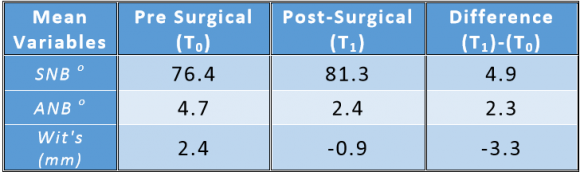
The descriptive statistics are summarised in Table-I, II shows the changes in the cephalometric measurements of the craniofacial morphology taken before and after the mandibular advancement surgery. The volumetric increase in the Pharyngeal Airway Space (PAS) for the patients (n=7) showed a significant increase from baseline (T0) to 3 months post-surgical (T1) (t=4.51, p=0.04 < 0.05), which is represented in Table-III. From baseline (T0) to the post-surgical measurements (T1), the total PAS volume for a mean mandibular advancement of 4.7mm showed an increase of 28.29%.Changes in the PAS volume before and after mandibular advancement surgery (volume in mm3) are given in Figure : 5-7.
5. Table I: Volumetric measurements of the Pharyngeal Airway Space before and after mandibular advancement surgery and their mean values of the patients (n=7)
Table II: Variables describing the craniofacial morphology of the samples both pre-surgical and postsurgical.
Table III
6. IV. Discussion
Several two-dimensional studies have evaluated the relationship between the airway, head posture, craniofacial morphology, and the positioning of the jaw bases. 1,2,13,14 However many drawbacks have been reported regarding the assessment of the airway using the lateral cephalograms. Some of them include, assessment of a three-dimensional structure using twodimensional imaging technique, measurements in "area" rather than "volume" and superimposition of structures.
To overcome these drawbacks, many studies have utilized the Computed Tomography (CT) Scan for the assessment of the Pharyngeal airway. [15][16][17] However the ionizing radiation and potential hazards of increased radiation dose with conventional CT Scan have limited its use in assessing the Pharyngeal airway. On the contrary CBCT imaging provides an adequate imaging quality with low radiation doses and shorter exposure time. Recently many studies have also been reported regarding the accuracy of CBCT in assessing the Pharyngeal Airway volume over the conventional lateral cephalograms, and CT Scans. 8,11 Aboudara et al 8 evaluated the PAS volumes determined from cephalograms and compared them with 3D-CBCT records. The 3D PAS analysis yields reproducible and clinically relevant data while being superior to cephalometric analysis. In the present study, Pharyngeal Airway Space (PAS) volume was analyzed by using the software PLANMECA ROMEXIS. The threshold value in the analysis software is an important tool in determining the boundaries of the airway to be measured. By varying the threshold value, the filling degree of the airway can get altered, and hence the measurements might be overestimated or underestimated when compared with the actual volume. Alves et al 18 evaluated the influence of threshold value in measuring the actual airway volume and reported that the accurate prototype airway volume could be obtained with thresholds between 70 and 75 when using the Dolphin 3D software. In the present study, Romexis Software was used; for the assessment of the airway volume, the software is provided with a pre-set local threshold value of 70, which was similar to that as suggested by Alves et al. and the software automatically calculated the airway volume in cubic millimeters.
Studies have reported that the variation in the anteroposterior jaw relationships show different pharyngeal airway volumes and patients with a retrognathic mandible have a relatively lesser airway volume when compared to the airway volume to that of a Class I skeletal base. 2,18 Treatment modalities for the correction of mandibular retrognathism in Class II patients in growing individuals include functional appliance therapy to advance the mandible where as in adults, surgical mandibular advancement is the only option available, both of which will have a strong influence in the airway volume. 19,20 Li et al. compared growing class II div1 patients and patients treated with twin block appliance and found an improvement in the oropharyngeal and the hypopharyngeal airway along with the anterior positioning of the hyoid bone after functional appliance treatment. 21 Several studies have reported the improvement of the PAS in Class II patients with mandibular retrognathia after mandibular advancement surgery. 22,23 Hernández et al. have stated that the mandibular advancement surgery results in greater improvement in the Pharyngeal airway volume due to the advancement of the skeletal attachment of the suprahyoid muscles and tendons that play a major role in the widening of the PAS. 24 Turnbull et al. described a similar effect in their cephalometric study demonstrating significant enlargement in the PAS after mandibular advancement surgery. It was noted that the volume increase is most pronounced in the lower and middle thirds of the PAS, which is related to post-operative advancement of the tongue, hyoid, and associated structures. 25 Kochel et al. in their 3D CBCT study assessed the Pharyngeal airway changes after mandibular advancement surgery in adult Class II patients and reported an increase in the PAS by 45.6%. 26 The improvement in the PAS in our study showed an increase of 28.29% for a mean mandibular advancement of 4.7mm. This was less when compared to that of the studies reported by Hernández et al. 24 and Kochel et al. 26 Probably, the reason for the reduced degree of improvement in our study is due to lesser sample size. Also, the degree of mandibular advancement might influence on the magnitude of the airway volume improvement, and Hernández et al. 24 have already reported that in their future study, they might try to evaluate a correlation between the magnitude of the skeletal forward movement and the increase in the PAS volume.
The present study evaluated the airway volume, three dimensionally using cone beam computed tomography in patients with skeletal Class II malocclusion with mandibular retrognathism. However, the limitations of the current study include limited sample size, and short-term follow-up. Moreover, the reliability of the software was not carried out.
7. V. Conclusion
The following conclusions can be drawn from the present study: 1) Mandibular advancement surgery increased the Pharyngeal Airway Space (PAS) in patients with the retrognathic mandible.
Our findings suggest that bilateral mandibular advancement surgery in patients with retrognathic mandible is a viable treatment option that not only improves the facial profile and esthetics but also enhances the functional characteristics of the airway by increasing its volume.