1. Introduction
ervical cancer is a disease that affects young women regardless of their ethnic origins, and it is a public health problem worldwide. 84% of new cases throughout the world occur in developing countries [1,2,3]. However, few types of the cancer can be prevented by two methods of prevention: screening for precancerous lesions and vaccination against the Human Papillomavirus (HPV), which prevents infection and is an effective weapon for its eradication. The vaccination of girls between "9-13" is recommended by The World Health Organization (WHO) against HPV. In Senegal, the vaccine against this cancer was introduced in the Expanded Programme on Immunization (EPI) on 31 October 2018 and targeted all girls aged 9. The vaccination of HPV raises many questions. The goal of our study is to assess resident's levels in gynecology and obstetrics of knowledge of the HPV and their attitudes towards its vaccination in Dakar Aristide Le Dantec teaching hospital, Senegal.
2. I.
3. Materials and Methods
It was across sectional, descriptive and analytical study conducted in Dakar with the residents in gynecology and obstetrics of the University of Cheikh Anta Diop from March 12 to July 30, that's five months and one day. We included in our study all residents in gynecology and obstetrics from de 1st year to the 4th year of the University of Cheikh Anta Diop. We had obtained the consent of each resident at the beginning of the survey. The study was excluded all residents who refused to take part. An information sheet (appendix) was used, as a basis for collecting data from the residents. Socio-epidemiological factors included age, education level, occupation, marital status, gynecological and obstetrical history, knowledge of human papillomavirus, and knowing of vaccination against human papillomavirus and acceptability oh papillomavirus vaccine.
4. II.
5. Statistical Analysis
It was carried out using of a structured individual interview using a questionnaire. The Epi info software version 7 saved the data collection and the data analysis with the SPSS software (Statistical Package for the social sciences) version 21. The latter consisted of two parts: descriptive and analytical analysis.
It consisted of a bivariate analysis by comparing the acceptance of HPV vaccine administration with the other variables (previous socio-demographic characteristics...). The statistical tests used were the Chi2 test for the percentage comparison, the student test, or ANOVA for the mean comparison. The difference was statistically significant when the p-value was strictly less than 0.05. The ORs adjusted with their [95% CI] were allowed to know the strength of the link.
6. III.
7. Results
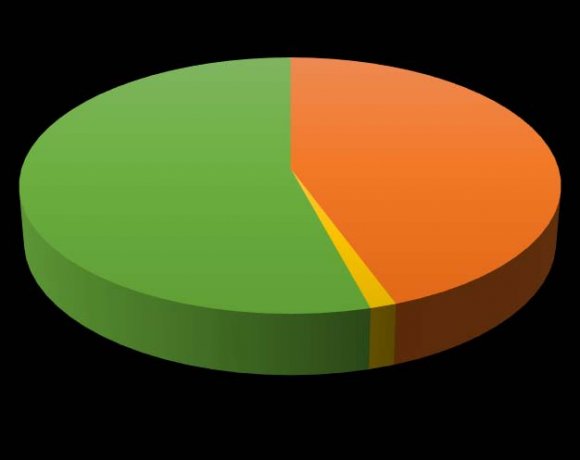
At the total, 76 residents of gynecology and obstetrics were enlisted. The average age of the residents was 30.7 years, with the extremes of 26 and 50 years. More than half of residents have more than 30 years. 54.2% of residents were married, as shown in figure 1. The average pregnancy was 0.8, with extremes of 0 to 4 pregnancies. The average age at first intercourse was 22.7 years, with extreme of 13 and 31 years. The age at first pregnancy was 27.6 years, with extremeness of 22 and 35 years. A medical history of cervical and breast cancer was found in 10.5% and 5.3% of residents, respectively, as reported in figure 2.
8. Pourcentage
9. Oui Non
In our series, all residents (100%) knew about HPV. Lessons (96.1%) were the principal sources of information. Among residents who knew about HPV, 93.2% consider HPV to be sexually transmitted infections, and 98.7% consider it to be responsible for cervical cancer, as shown in table 1 and figure 3. Among residents who were aware of the HPV vaccine, only (30.6%) were aware of the side effects. Pain at the site (45.5%) of injection and skin lesions (45.5%) were the most known side effects of residents, as reported in Table III. Among residents who were aware of the HPV vaccine, only forty-five (59.3%) were aware of the routes of administration of the vaccine. All had cited intramuscular injection as the route of administration. In our study fifty-five residents (76.4%) knew the targets. Girls under 13 years of age were the main targets mentioned by women as reported in Table IV.
10. Table I: Distribution of residents according to their sources of information on the HPV vaccine (N=76)
11. Sources on vaccine information on HPV
Tableau III: Distribution of residents by HPV vaccine side effects (N=2) ) were known to accept to take the HPV vaccine. According to sociodemographic characteristics, there were statistically significant differences in the acceptability rate the HPV vaccine. For example, residents in the 1st and 2nd year were 7.8 times more likely to accept the vaccine (Table VI). The distribution of acceptability of the HPV vaccine was almost like according to family history (Table VII).
12. The distribution of the acceptability of the HPV vaccine was almost similar according to the knowledge of HPV (table V).
Table VI shows that the distribution of acceptability of the HPV vaccine varied, according to the education level of the respondents. Indeed, the acceptability of vaccination against HPV was 7.8 times high among 1st and 2nd-year residents. In table V, 60% think HPV is not an STD, and the main cause of refusal of vaccination is le lack of knowledge 56%.
13. Discussion
14. Socio-demographics characteristics
In our study, the average age of residents was 30.7 years; the majority were married (54.2%). The mean age at first intercourse was 22.7 years; the average was 24 years. The mean age at first pregnancy was 27.6 years with extremes (22 and 35). The average pregnancy rate was 0.9, and the average parity rate of 0.8. A medical history of cervical and breast cancer was found in 10.5% and 5.3% of resident, respectively. The resident survey, and data from Gassama can be superimposed our data.
15. Knowledge
During our study, 100% of student knew about HPV, among which 93.2% consider HPV to be an STI and 98.7% consider it to be responsible for cervical cancer which corresponds to the results of a study among students in china with a slightly lower rate 67.8% and 86.1% respectively [14] and 85.8% in a study in South Africa [5]. However, in a study in Lagos's knowledge about was very poor, as only 39.8% had good acquaintance of the subject [8]. For the residents, knowledge of the main etiological factor is paramount in the prevention of this scourge.
Regarding the source of information, most of the residents interviewed had heard about it through school course, which was consistent with a finding from a Chinese study followed by an entourage, the media (television, radio) [14]. However, in a study in Lagos, the three highest sources of knowledge and information about HPV vaccination among the respondents were identified as, internet (23.2%), television/radio (14.9%), and teachers (12.4%) [8].
As for vaccination, ¾ of residents (72.4%) knew about the HPV vaccine. The main sources of information -generally the lessons (96.1%), the media (26.3%) and the entourage (3.9%) as a study in South Africa the principal sources of knowledge reported by the participants were school (60.1%) and the media (33.0%) [5]. Media plays a significant role in getting information to the youth, which can create and raise awareness about cervical cancer and HPV. Residents have a high percentage (100%) of knowledge of the cervical cancer vaccine, and this is related to the level of education and instruction provided during their teaching, and 62.0% knew that the vaccine was available in South Africa [5]. This finding is made by several authors who have shown that, for example, in a study conducted in China, the knowledge they have about the HPV vaccine is mainly related to the teaching given [6,7]. However, in a study in India, none of the students were aware of cancercausing HPV types and names of the HPV vaccines, which reflect that they have very restrictive knowledge and understanding of the disease [6].
16. Acceptability
In 44 residents, (59.5%) was noted the acceptability of taking the HPV vaccine, corroborating the findings of one Chinese study (57.2% among male and 78.5% among female) [14]; the main reason was the prevention of cervical cancer and concern about the virus and its health consequences. Actually, there is a correlation between the fact of being sensitized about the HPV, the vaccine, and its acceptability.
On the contrary, in France in 2018, a study revealed that a relatively not enough knowledge of the disease does not constitute a barrier to the acceptability of vaccination [10]. The increased reluctance in France of vaccination can be explained by these contradictions. One of the reason of residents for the no acceptability of the vaccination is the lack of knowledge about the anti-HPV vaccine and the lack of information (Consistently, lack of information about HPV infection and vaccines has been identified as a common barrier to the uptake of HPV vaccines in earlier studies (Kahn et al., 2003;Lee et al., 2007;Iliyasu et al., 2010). These are the reasons why lack or less information can hinder vaccination [14]. In India, the reasons for not getting vaccination are cost, safety, efficacy, no knowledge [7]. Reason for unwillingness to accept the HPV vaccine in Lagos is a lack of adequate information on the HPV vaccine (63.2%), fear of negative consequences of receiving the HPV vaccine (12.4%), and fear of injections (8.0%) [8].
Vaccination against cervical cancer is a controversial subject, especially the side effects such, as autoimmune diseases, multiple sclerosis as reported in literature. These side effects are not attributable to vaccination and yet are major obstacles to the acceptability of vaccination. In our study, the most wellknown side effect is the reaction at the injection site (4.5%).
We can, therefore, consider that have already received information on cervical cancer and its prevention methods promotes vaccination. It should, therefore, encourage us to inform as many representatives of the medical community as possible so that they can correctly relegate information to the population on HPV vaccination.
Also, the second barrier to HPV vaccination was related to the vaccine itself, the fear of side effects, and this matches with the literature. Fear of side effects is at the top of the list in most acceptability surveys.
In an American study published in 2013, there was even an increase in this concern, with 4.5% of parents worried about possible side effects in 2008, compared to 16.4% in 2010 [11].
V.
17. Conclusion
Acceptability of HPV vaccination requires knowledge of the papillomavirus and vaccination. Awareness remains an essential element in the prevention strategy.
| Knowledge on the HPV | Acceptability of vaccine | ||||||||
| vaccine | Yes | No | Total P value Ods[Ic à 95%] | ||||||
| N | % | N | % | ||||||
| Sources of information on | 0,481 | ||||||||
| Side effects of HPV vaccine HPV one source 34 | Number 61,8 21 38,2 55 | Percentage 1,5[0,5-4,2] | |||||||
| Pain at the site of injection More than one source | 10 | 52,6 9 | 10 47,4 19 | 45,5 | Ref | ||||
| Skin lesions HPV responsible of STD Neurological trouble Yes Non | 40 2 | 10 2 59,7 27 40,3 67 40,0 3 60,0 5 | 0,388 | 45,5 2,2[0,3-14,2] 9,1 Ref | |||||
| Headache HPV responsible of breast | 3 | 0,400 | 13,6 | ||||||
| Vomiting cancer Fever yes Nausea No Sources of vaccine | 42 1 | 3 2 58,3 30 41,7 72 2 100,0 0 0,0 1 | 0,253 | 13,6 9.1 9,1 | 0,0 | ||||
| Sclerosis information | 2 | 9,1 | |||||||
| Itching one source Diarrhea More than one source Infertility Type of vaccine Yes In our study, 44 residents (59.5% | 30 10 43 | 2 54,6 25 45,4 55 1 71,4 4 28,6 14 1 59,7 29 40,3 72 | 0,782 | Ref 2,1[0,6-7,4] 9,1 4,5 4,5 1,5[0,1-26,7] | |||||
| Lupus No | 1 | 50,0 1 | 1 50,0 74 | 4,5 | Ref | ||||
| Stenosis Side effects Urticaria Yes Arthralgia No Way of administration | 11 32 | 1 1 50,0 11 50,0 22 1 65,3 17 34,7 49 | 0,222 0,430 | 4,5 0,5[0,2-1,5] 4,5 Ref 4,5 | |||||
| Yes | 31 | 55,4 25 44,6 56 | 0,6[0,2-2,0] | ||||||
| No | 10 | 66,7 5 | 33,3 15 | Ref | |||||
| Targets Targets | Number | Percentage 0,236 | |||||||
| Virgin girl Yes No | 42 2 | 55 58,3 30 41,7 72 100,0 0 0,0 2 | 76,4 | ||||||
| Virgin teenagers Age of vaccin | 10 | 0,104 | 13,9 | ||||||
| All people Yes No | 37 7 | 1 57,8 27 42,2 64 87,5 1 12,5 8 | 0,2[0,02-1,7] 1,4 Ref | ||||||
| All women HPV entourage | 6 | 0,542 | 8,3 | ||||||
| Total Yes Non | 11 31 | 72 35,3 17 56,4 24 43,6 55 64,7 6 | 1,4[0,4-4,4] 100 Ref | ||||||
| Lack of information | 0,072 | ||||||||
| Yes | 11 | 44,0 14 56,0 25 | 0,4[0,2-1,1] | ||||||
| No | 31 | 66,0 16 34,0 47 | Ref | ||||||
| IV. | ||||||
| Social-demographic | Acceptability of vaccine | |||||
| characteristics | Yes | No | Total P value Ods[Ic à 95%] | |||
| N | % | N | % | |||
| Age group | 0,776 | |||||
| <30 | 17 63,0 10 37,0 | 27 | 1,1[0,4-3,2] | |||
| ?30 | 22 59,5 15 40,5 | 37 | Ref | |||
| Occupation | 0,286 | |||||
| Married | 22 56,4 17 43,6 | 39 | 0,6[0,2-1,6] | |||
| Single | 22 68,7 10 31,3 | 32 | Ref | |||
| Level of residency | 0,000 | |||||
| 1&2 | 36 76,6 11 23,4 | 47 | 7,8[2,7-22,6] | |||
| 3&4 | 8 | 29,6 19 70,4 | 27 | Ref | ||
| Gender | 0,271 | |||||
| Female | 28 56,0 22 44,0 | 50 | 0,5[0,2-1,6] | |||
| Male | 16 69,6 7 | 30,4 | 23 | Ref | ||
| Address | 0,174 | |||||
| Dakar Suburb | 15 78,9 4 | 21,1 | 19 | 2,4[0,7-9,0] | ||
| Dakar Center | 20 60,6 13 39,4 | 33 | Ref | |||
| Family history | Acceptability of vaccine | |||||
| Yes | No | Total P value Ods[Ic à 95%] | ||||
| N | % | N | % | |||
| Cancer du col | 0,515 | |||||
| Yes | 3 | 75,0 1 | 25,0 | 4 | 2,1[0,2-21,4] | |
| No | 41 | 58,6 29 41,4 | 70 | Ref | ||
| Breast cancer ( age | 0,852 | |||||
| group) | ||||||
| ?25 | 5 | 62,5 3 | 37,5 | 8 | 1,1[0,2-5,2] | |
| >25 | 39 | 59,1 27 40,9 | 66 | Ref | ||