1. Introduction
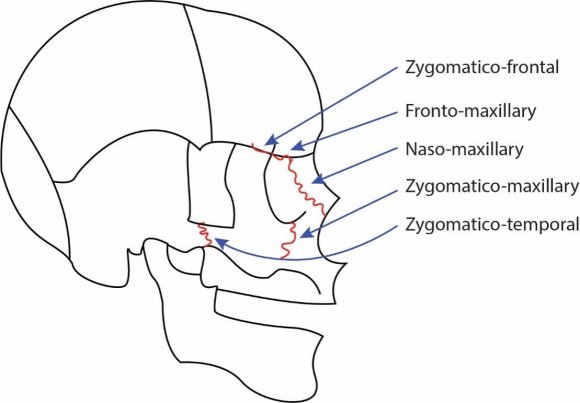
he maxilla articulates with nine other bones: the frontal cranial and the ethmoid, as well as the "nasal, zygomatic, lacrimal, inferior nasal concha, palatine, vomer, and the adjacent fused maxilla." It is connected to other bones above through sutures. (Figure 1).
In growing children, the maxilla departs from circummaxillary sutures when face mask treatment is applied (1). Face masks, also called reverse-pull headgear, have been used throughout much of history to move the maxilla both forwards and downwards in patients with midfacial deficiencies (2). Figure 2 depicts the clinical application of a face mask.
2. Figure 2: Clinical application of a face mask
The best treatment timing for growing patients is still controversial, and the correlation between cooperation and age is one of the most confounding variables. (3)(4)(5) The recommended wearing time of a face mask is usually longer than 14 hours in a day (6) (7), but this is entirely dependent on the cooperation of the patient. Studies report that received compliance is insufficient (8) (9). A previous study suggested measuring wear time using TheraMon chip technology, which used sensors that collected time and temperature data. It was placed on the forehead of the patient. (10) However, to our knowledge, no attempt has been made to measure the force applied against the full reverse headgear in real-time. Since the suggested force for face masks lies around 300 to 400 grams, keeping this pressure consistent, especially during sleep, is a challenge. To overcome the complications in this process, we used IoT technology and transferred the collected data onto their phone in real-time to use as an asset. This data could be used to create an entirely This sensor used rubber bands to detect the weight applied to the face mask.
3. Materials and Method
4. Arduino Force Sensor Circuit
This force sensor converted the code from the sensor into units (grams).
5. MIT App Inventor
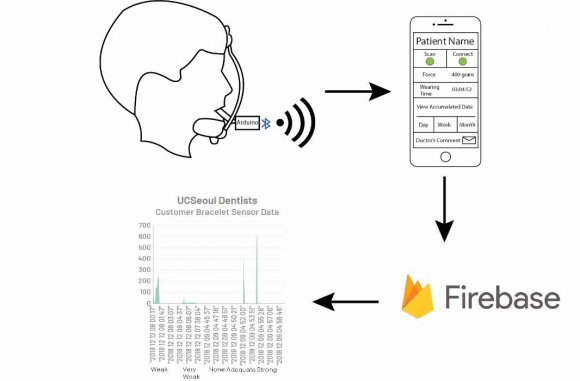
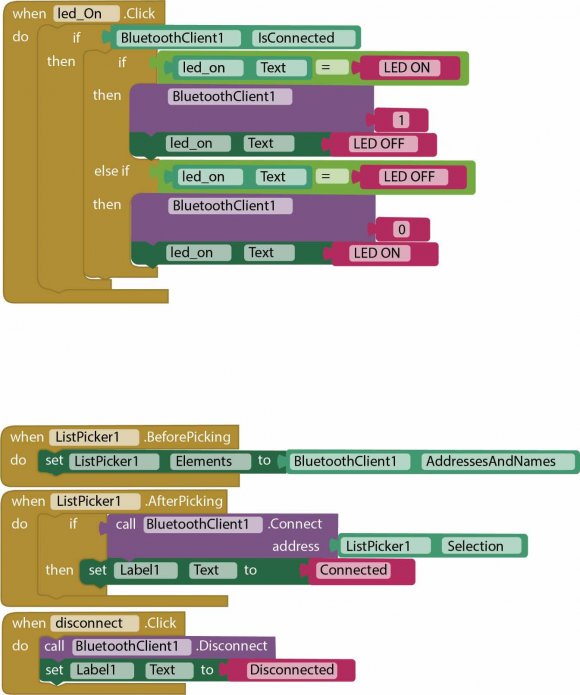
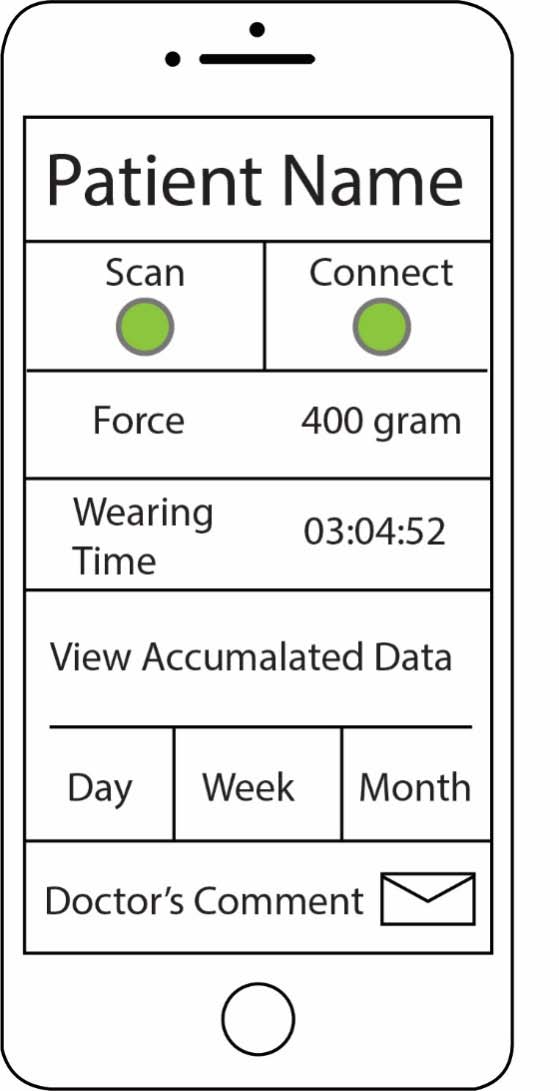
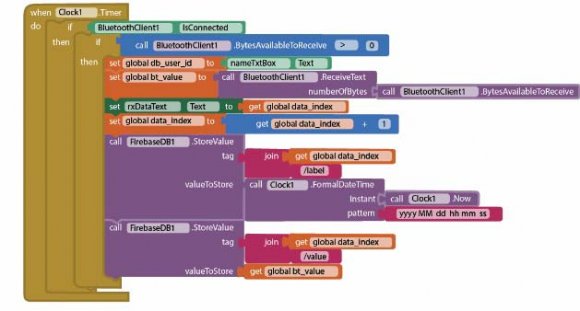
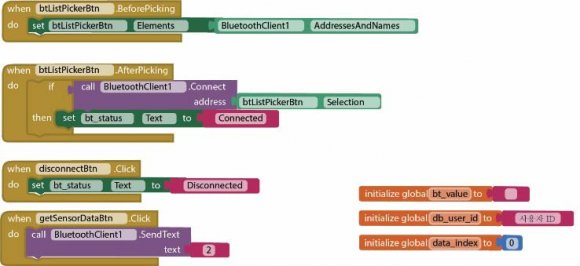
The face mask patient would run an app to connect their phone to this Bluetooth circuit, which was coded (Figure 4) and designed using MIT App Inventor. When a subject presses a 'scan' button, it will send data to the phone. (Figure 5)
6. Arduino Bluetooth Circuit
This connects the Arduino force sensor to the Bluetooth network, connecting the sensors and the patient's phone. This required coding to detect when the data should be sent, i.e., when the LED was turned on, signifying that the Bluetooth signal was functioning.
7. Google Firebase
This database sent data from Arduino Bluetooth so that it could be accessed by people other than the patient, making the system functional. (Figure 6)There was also a private cloud generation process necessary to prepare it.Once data is transported from the phone to Google Firebase, the database offers it to both the patient and the orthodontist.
8. Results
Utilizing face masks and IoT technology, we were able to detect whether and how much weight (0 to 1000 grams) was being applied to a face mask in realtime with an interval of thirty seconds. (Figure 7).
9. Discussion
Orthodontists always strive to apply the optimal force to their patient's orthodontic devices. However, due to the amount of patient cooperation necessary to conduct their practice successfully, keeping track of how much force is being applied at home and outside of the clinic seems impossible.
The advent of IoT technology could potentially solve his problems.
It opens comprehensive treatment care for both doctors and patients (Figure 3). When the patients wear the facemask attached to the sensor, Bluetooth will transfer the amount of force to their cell phones. The data is real-time based, and the patient can identify the force level, which is also shown graphically in the background (Figure 4). Further warning messages or beeps will be incorporated when the patients use weak or loosened elastics or insufficient wearing time is noted. Our results were able to detect and digitalize how much weight was being applied, as well as the patient's cooperation. Such data collected will enable far more concise feedback for patients in the future. Besides, the accumulated results will be able to reveal efficient wearing time and force for individual patients, rather than just longer than 12 hours a day. Therefore, doctors can instruct individualized optimum force and wearing time based on scientific evidence with confidence.
V.
10. Conclusion
We suggested an IoT based tractable system for a facemask. This workflow can be widely applicable to any removable appliances in the future. Collected data will provide a comprehensive understanding of optimal force and timing for the treatment.