1. Introduction
dolescence is a period marked by transitions and search for new experiences, such as sexual awakening, making girls more susceptible to unwanted pregnancy. Poverty and socioeconomic inequalities can further increase rates of teenage motherhood, mostly due to knowledge gaps and lack of informations about contraception.
In Brazil, 547,564 babies are born annually to adolescent mothers, accounting for 18% of all births and 11.43% of births in the South region 1 . Adolescence is a period of woman's life when major physical, cognitive, and social transformations occur, marking the transition from childhood to adulthood. Adolescent pregnancy is a public health problem and may be related to the occurrence of maternal-fetal complications such as preeclampsia, prematurity, infections, low fetal weight, among others 2,3 . There is closely intertwined between maternal nutritional status before and during gestation and neonatal outcomes 4 . Pregnancy before the age of 15 years old can be harmful to maternal and fetal health since both are under physical development and can compete for nutrients. This competition may increase the odds of low neonatal weight, micronutrient deficiencies, and fetal growth restriction 5 .
Obesity is a complex and multifactorial disease with rising prevalence worldwide 6 . In the last decades, rates of weight excess among Brazilian adolescent girls have nearly tripled 7 . Pregestational obesity is a risk factor for excessive weight gain during pregnancy and is associated with complications such as diabetes, postpartum hemorrhage, infections, thromboembolic events, and disturbs in childbirth 8 . It can also cause hypertensive syndromes, which lead to poor perinatal outcomes 9 . Maternal obesity is also associated with neonatal events such as fetal macrosomia, increased admission in the neonatal intensive care unit, congenital disabilities, hypoglycemia, low Apgar score, and death 10 .
The combination of adolescent pregnancy and obesity can further impact health outcomes in both generations. Therefore, this study aims to evaluate the relationship between pregestational weight excess and the occurrence of maternal and fetal outcomes among A pregnant adolescents in a university hospital in Southern Brazil.
2. II.
3. Methods
Between November 2014 to March 2016, we conducted a cross-sectional study carried out among puerperal adolescents (10 to 19 years old) that attended a university hospital in southern Brazil. We interviewed the adolescents in the postpartum period, after theysigning a free and informed consent form and answered questionnaires on socio-demographic, gestational and perinatal data. Ethics Committee of Hospital de Clínicas de Porto Alegre approved the project. (protocol number 14-0491).
Pregestational nutritional status was analyzed using Anthroplus software, and body mass index (BMI) z-score from 1 to -1 was considered eutrophic and ?+1 weight excess 14 . We evaluated gestational BMI according to the Atalah curve published in 1997 15 . Weight gain during pregnancy was defined suitable from 12.5-18 kg for those with initial low weight, 11.5-16 kg for eutrophic, 7-11.5 kg for overweight, and 5-9 kg for those obese, as recommended by the IOM (Institute of Medicine) 16 .
Maternal clinical variables evaluated were menarche, age at first sexual intercourse, number of gestations/parity, type of delivery, number of prenatal visits, previous and gestational diseases such as hypertension, diabetes, gestational hypertension and diabetes, obesity, anemia, and preeclampsia. According to the World Health Organization (WHO) criteria, the birth is preterm when it occurs before 37 weeks 17 . We classified hypertensive disorders according to the recommendation of ACOG (American Congress of Obstetricians and Gynecologists) 18 .
Fetal variables collected were gestational age at birth, sex, weight, length, hospitalization in the neonatal intensive care unit (ICU), and complications such as respiratory dysfunction and Apgar score. We evaluated gestational age at birth using the Capurro method.
Data were analyzed using SPSS (Statistical Package for the Social Sciences) version 18.0 (SPSS Inc., Chicago, IL, EUA®). Categorical variables are presented by absolute number (n) and percentage (%), symmetric continuous variables by the mean and standard deviation (SD), and continuous variables asymmetric by the median and interquartile range [25-75 percentile]. We used a Chi-square test for categorical variables and t-test for quantitative variables. We considered, for all analyses, a significance level of 5% (p<0.05) and a 95% confidence interval.
4. III.
5. Results
We evaluated five hundred adolescents and their respective newborns. Maternal mean age was 17.77 ± 1.36 years, with the mean age at first sexual intercourse at 14.8 ± 1.5 years. 57.6% (n=235) had a family income of 1.5 to 3 minimum wages, and 63% had white skin color. Primiparous women composed 83.4% of the sample, and 84.8% (n=420) were single with a partner. Regarding pregestational nutritional status, 31.2% (n=156) were weight excess. Table 1 shows other characteristics of the sample.
Table 2 shows the association of pregestational body mass index classification with maternal and fetal outcomes. Mothers with pregestational weight excess were more likely to attend fewer prenatal consultations (24.7% vs. 36.3%, p=0.007) and have excessive weight gain during pregnancy than the others (62.2% vs. 32.9%, p<0.001). Prevalence of gestational hypertension (5.1% vs. 1.7%, p=0.037) and gestational diabetes (4.5% vs. 1.5%, p=0.045) were higher in the weight excess group when compared to the lean/eutrophic group. The proportion of birth by cesarean was also significantly higher in weight excess adolescents (24.4% vs. 17.2%, p=0.04).
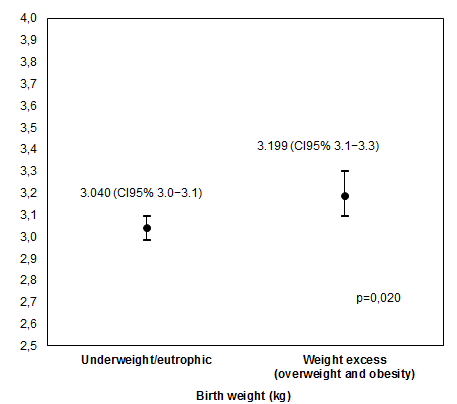
Children of weight excess mothers had a longer length (48.3 cm vs. 47.5 cm, p=0.018) and weight (3.199 kg vs. 3.040 kg, p = 0.020) at birth, as observed in figures 1 and 2, respectively. Prematurity, neonatal ICU admission, respiratory dysfunctions, and Apgar score were not associated with pregestational weight excess.
IV.
6. Discussion
Pregnancy in women before the age of 19 years is characterized by poorer outcomes when compared to those aged 20-24 years 19 . One explanation for this is that teenage mothers are smaller, due to uncompleted growth at conception. Competition for nutrients can occur between the still developing mother and the fetus, causing developmental impairment in one or both parts. The deficiency of nutrients and energy due to gestation can further impair growth and make adolescent mothers more prone to metabolic imbalances such as obesity and cardiovascular diseases in adulthood 20 .
Obesity is a growing public health problem. In the United States, the prevalence of overweight in girls aged 12 to 19 years was 4.7% in 1970, increasing to 15.4% in 2002 21 . In Brazil, weight excess affects more than 23% of teenage women 7 . Obesity during adolescence can persist in adulthood, increasing the risk of associated diseases such as hypertension, diabetes mellitus, osteoarthritis, and cardiovascular disease 22 . Furthermore, maternal obesity is associated with adverse obstetric outcomes, such as increased cesarean rates, preeclampsia and, gestational diabetes. A menarche is a late event in the pubertal process that is related to genetic, environmental, and nutritional factors. Literature shows that adolescents with a higher risk of obesity in adulthood are those with early menarche and those with a short period between menarche and first parturition 37 . We also observe this correlation in our study, as weight excess young women had menarche at an earlier age.
During pregnancy, women with overweight and obesity should gain a maximum of 11,5 and 9 kg, respectively 26 . Adolescent mothers are more likely to have inappropriate weight gain compared with adult women 36 , and over 60% of teenage mothers have excessive weight gain. In our study, 31.2% of them had pregestational overweight, and the majority of those gained gestational weight above the recommended for their BMI before pregnancy, corroborating with previous findings 31,34. The weight gain can be explained because the body of adolescents has to work to both meet their own growth needs and those of the fetus.
Prenatal consultations provide the necessary medical support during pregnancy, and performing them correctly is necessary to prevent possible complications associated with maternal and fetal health. Pregnant women with weight excess were significantly more likely to have inadequate prenatal care, having less than the six visits recommended by the Brazilian Ministry of Health 32 . Adolescent mothers may not attend gestational care due to fear or non-acceptance of the pregnancy; therefore, professionals should be rightly trained to guide and stimulate them about gestational care 32 .
Regarding maternal outcomes, we found a significant association of maternal weight excess with hypertension and gestational diabetes mellitus (GDM), corroborating literature previous findings. Sukalich et al. showed that cesarean delivery, preeclampsia, and gestational diabetes were more frequent in pregnant women with a BMI greater than 25, as well as labor induction and cephalic-pelvic disproportion 36 . Another study also demonstrated that maternal weight excess and excessive weight gain during pregnancy were associated with an increased risk of gestational hypertension 46 . The association between obesity and GDM can be explained by more propensity of decreased insulin sensitivity before and during gestation in these women 47,42 .
In our study, 24.4% of overweight adolescents had cesarean deliveries. A study with obese teenage mothers at hospitals in the United States 42 and Colombia 20 found similar results. High prevalence of cesarean deliveries may be related to higher fetal weight in mothers with a still-developing body structure 43 . Furthermore, we stand out that our study obtained a mean number of the cesarean sections below the national average reported by the Brazilian National Health System Database of 2011 44 . This finding may be related to the fact that these adolescents were in a tertiary hospital that prioritizes vginal delivery and has specific institutional protocols regarding medical indications of cesarean.
Excessive weight gain during pregnancy and pregestational weight excess can result in newborns with bigger weight and length 46,48,49 . These findings are in agreement with our study since a significant association of maternal weight excess and anthropometric variables of the babies was found. Pregnant women who are overweight, obesity, or underweight can still have babies of adequate birth weight, provided that they gained appropriate weight during pregnancy 11 .
V.
7. Conclusion
Adolescence is a period of transition in which girls are still in the stage of physical and psychological growth. Gestation alone, at this stage, is already a risk factor for adverse outcomes. Our study demonstrates that these adverse outcomes are potentiated when gestation in adolescence is associated with obesity. Excessive weight increase during pregnancy is also associated with adverse maternal and fetal outcomes, such as preeclampsia, increased rate of cesarean section, and macrosomia. These findings highlight the necessity of further studies in the adolescent population, which accounts for 20% of all deliveries.
This study has a few limitations. Among the significant results, such as the association between obesity and gestational hypertension, confusion factors may be involved. Also, we obtained pre-pregnancy informati from participants' reports, depending on memories.
Our study contributes to a better understanding of pregestational weight excess in teenage mothers. The assessment of the initial nutritional status is essential to adjust weight gain during pregnancy, to minimize possible harms to the mother-child binomial. Although historically, the concern with teenage motherhood involves low weight gain and nutritional deficits, increasing rates of obese pregnant adolescents make interventions in eating habits is necessary to change this paradigm. Therefore, educational programs orientating this population about contraception, pregnancy, and healthy eating habits should be implemented, as well as actions encouraging early prenatal care. Acknowledgments: We would like to express our deepest gratitude to the participants for their time and patience throughout this study.
Financial disclosure: The authors have no financial relationships relevant to this article to disclose.
| Average | Standard deviation |
| Underweight/Eutrophy | Weight excess 1 | P value | |
| Mean age at menarche, years | 12.38 ± 1,67 | 11.62 ± 1.63 | <0.001* |
| Apgar score | |||
| 1st minute | 7.85 ± 1.94 | 7.95 ± 1.57 | 0.594 |
| 5th minute | 9.03 ±1.58 | 9.06 ± 1.01 | 0.833 |
| Number of prenatal care consults | |||
| < 6 consults | 122 (36.3) | 38 (24.7) | 0.007 |
| ? 6 consults | 214 (63.7) | 116 (75.3) | |
| Weight gain during pregnancy | |||
| Insufficient | 124 (36.2) | 23 (14.7) | |
| Adequate | 106 (30.9) | 36 (23.1) | <0.001* |
| Excessive | 113 (32.9) | 36 (62.2) | |
| Pathology during pregnancy | |||
| No | 95 (27.7) | 44 (28.2) | 0.494 |
| Yes | 248 (72.3) | 112 (71.8) | |
| Gestational hypertension | |||
| No | 228 (98.3) | 148 (94.9) | 0.037* |
| Yes | 6 (1.7) | 8 (5.1) | |
| Preeclampsia | |||
| No | 127 (95.1) | 146 (93.6) | 0.316 |
| Yes | 17 (4.9) | 10 (6.4) | |
| Gestational diabetes | |||
| No | 339 (98.5) | 149 (95.5) | 0.045* |
| Yes | 5 (1.5) | 7 (4.5) | |
| Anemia during pregnancy | |||
| No | 216 (63) | 108 (69.2) | 0.104 |
| Yes | 127 (37) | 48 (30.8) | |
| Type of delivery | |||
| Vaginal | 285 (82.8) | 118 (75.6) | 0.040* |
| Cesarean | 59 (17.2) | 38 (24.4) | |
| Labor complications* | |||
| No | 313 (91) | 140 (89.7) | 0.385 |
| Yes | 31 (9) | 16 (10.3) | |
| Gestational age | |||
| Preterm | 45 (13.4) | 23 (14.7) | 0.393 |
| Full term | 297 (86.6) | 133 (85.3) | |
| Newborn complications** | |||
| No | 245 (71.2) | 108 (69.2) | 0.703 |
| Yes | 98 (28.5) | 48 (30.8) |