1. Introduction
besity is a chronic illness where there is an increase in body fat. Its prevalence has increased considerably both in developed and developing countries. It is usually the result of an unbalance between calorie intake and output. Its excess leads to high morbidity and mortality rates and to socially significant direct and indirect economic burdens. Body mass index (BMI) is a relatively simple method to measure body fat, calculated by dividing the weight in kilograms by the square of the height in meters, expressed in kg/m 2 (WHO 1997).
2. O
The following parameters are registered: height (meter) and weight (kg) in order to obtain BMI (kg/m 2 ), age, fresh spermatic count (m/mL), progressive motility (%) and normal morphology (%).
Like every other systemic illness, obesity affects every tissue, including the reproductive system. On the one hand, most published studies up to date have focused on analyzing the impact of BMI on female patients, reporting its negative effect on fertility potential, hormone levels, the increase in the risk of developing polycystic ovary syndrome, anovulation, and poor results after an assisted reproduction treatment (ART) (Pinborg et al (2011)).
On the other hand, both male overweight and obesity cause endocrine disorders that can affect reproductive capacity. Some authors inform of a negative impact on natural and assisted conception, while others report similar reproductive results to those observed in males with normal BMI. Regarding the influence of male BMI on seminal quality, studies are more controversial, as this relationship is multifactorial and represented by an altered hypothalamic-pituitarygonadal axis, peripheral aromatization of steroids to estrogen, decrease in testosterone levels, increase in estradiol levels, decrease in binding of sexual hormones to globulin and an increase in scrotal temperature (Crujeiras, A.B., Casanueva, F.F., 2015). Moreover, there is proove that the accumulation of toxic substances and liposoluble endocrine disruptors in the fatty tissue magnifies these disruptions (Katib, A., 2015; Sermondade, N, 2013) . Some publications have been able to relate the increase in BMI in infertile males with poor spermatic quality (decrease in sperm concentration, abnormal sperm morphology, and decreased motility) in comparison with normal BMI males (Hanafy, S., Halawa, F.A., Mostafa, T., Mikhael, N.W., Khalil, K.T., 2007; Hofny, E.R., et al. 2010). Regarding spermatic DNA integrity, it has not been possible to establish an association between greater DNA damage in overweight and obese males (Smit, M., Romijn, J.C., Wildhagen, M.F., Weber, R.F., Dohle, G.R., 2010). However, some authors have observed an increase in mitochondrial damage of sperm belonging to overweight patients (Bandel, I. et al. 2015).
The objective of the current study was to investigate if the increase in male BMI is associated with seminal parameter quality.
3. II.
4. Materials and Methods
The present study is a retrospective observational study, where the medical records of 1009 males who consulted in Instituto FIVIR of Valencia were reviewed between January 2011 and December 2018.
The information included was that of patients who met the following criteria: ? Inclusion criteria: being 18 years old or older, male, weight and height registered previous to obtaining the sperm sample, one spermiogram made at this clinic with the following parameters: spermatic count per ml (million per milliliter (m/mL)), motility (%), normal morphology (%). The conditions for collecting the seminal sample were: three-day abstinence, no history of fever in the previous four weeks, and obtaining the total of the ejaculated fluid. ? Exclusion criteria: Patients with a medical history of chronic illness that require chronic medical treatment, cigarette, alcohol, and other toxic consumption. Patients with an oncological history who required treatment with chemotherapy, radiotherapy, or testicular surgery.
The seminal fluid parameters and definitions of the spermiogram used were those determined by WHO (2010 5th edition). Hence: concentration ( ? 15 x 10 6 /ml), progressive motility ( ? 32%), sperm morphology (normal forms > 4%).
The classification of BMI was adapted from the World Health Organization's (WHO) (World Health Organ Tech Rep Ser., 2000).
? Underweight -BMI under 18.5 kg/m2
? Normal weight -BMI greater than or equal to 18.5 to 24.9 kg/m2 ? Overweight -BMI greater than or equal to 25 to 29.9 kg/m2 ? Obesity -BMI greater than or equal to 30 kg/m2 III.
5. Statistical Analysis
The normality of the continuous quantitative variables was evaluated using the Anderson-Darling test, resulting in all of them non-normal. The mean values of the abnormal continuous quantitative variables were compared using the Kruskal-Wallis test, considering a p value of p? 0.05 as a statistically significant difference.
IV.
6. Results
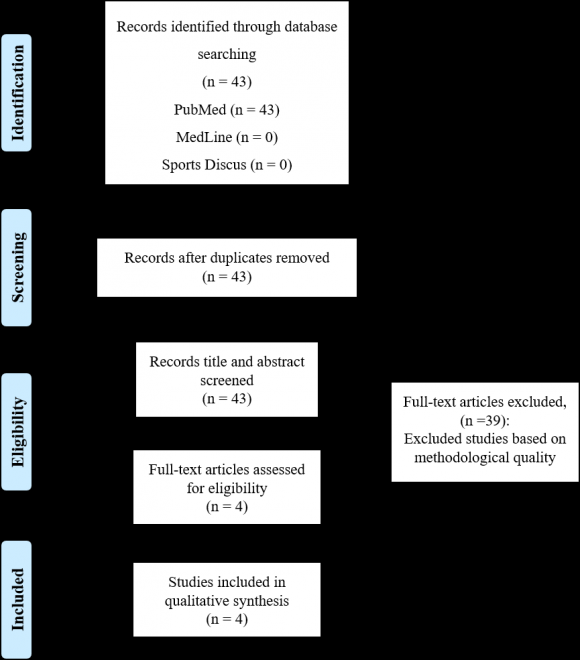
During the study period, 1009 white European males between 20 and 46 years old were attended, of which 471 met the criteria (Figure 1), with an average age of 32.8 (SD ± 3.491) (21 -41 years old). The classification was made according to their BMI, and the distribution was: Low weight or LW (BMI ? 18.5) in none of the patients; Normal weight or N (BMI between 18.5-24.9) in 212 patients; Overweight or OW (BMI between 25-29.9) in 193 patients and Obesity or OB (BMI ? 30) in 66 patients. Therefore, patients with normal BMI(N) represent 45% of the studied population, whereas patients with excess weight are 55% of the studied population. The characteristics of the population are described in Table 1. There were no statistically significant differences found for age (Kruskal-Wallis p=0.308) between the groups. Sperm normality (%) had no statistically significant differences according to the classification of BMI (Table 4). Males with obesity or over weight had a significantly lower sperm concentration and progressive motility than men of normal BMI (p< 0.05). Tables 2 and 3.
V.
7. Discussion
The relationship between male obesity and fertility has been widely described. However, there is a debate regarding the magnitude of this relationship and its mechanisms. On the one hand, various groups of researchers have not been able to establish any or little relation between BMI and a worsening of spermatic quality, as registered by MacDonald et al. in a revision of the most relevant publications (31 studies) between January and February 2009 (MacDonald, A.A., Herbison, G.P., Showell, M., Farquhar, C.M., 2010). Similar findings were found by Chavarro et al. in the study carried out on 483 males where BMI had no association with sperm concentration, motility, or morphology. Moreover, males with BMI ? 35 kg/m 2 had lower total sperm count than males with normal BMI, showing that only extreme obesity impacts negatively on male reproductive potential (Chavarro, J.E., Toth, T.L., Wright, D.L., Meeker, J.D., Hauser, R., 2010) mainly affecting maturation in the epididymis and therefore it is considered a poor prognostic factor. Furthermore, males with obesity present an increased risk of oligo and teratozoospermia (Luque EM et al. 2017) azoospermia and alterations in hormonal serum parameters, which show a slight but significant association with BMI, possibly contributing to sub fertility in this population (Bieniek JM et al. 2016).
On the other hand, researcher groups such as Belloc et al. (2014) found a clear association between BMI increase and seminal quality decrease, where volume, concentration, and sperm motility were mostly affected. However, the percentage of normal forms was not diminished (Belloc, S et al, 2014) as opposed to the findings of Oliveira et al. even though they did not find an association with an increase in DNA fragmentation (Oliveira, J. et al., 2018).
In the present study, more than half of the males included (55%) suffered from obesity or overweight (14% and 41%, respectively). This data is similar to that found in a recently published article where 60.9% of the general Spanish population suffers from these conditions and, in comparison to preceding data, shows an increase mostly in males (Aranceta-Bartrina J., Pérez-Rodrigo, C., Alberdi-Aresti, G., Ramos-Carrera, N., Lázaro-Masedo, S., 2016). Such data is even more significant as amongst these men, there is a 50% higher probability of presenting infertility when compared with healthy weight males (Phillips KP, Nongnuj T., 2010).
The average sperm count was lower in patients with overweight and obesity, this is in accordance with previous studies where there is up to 20% fewer spermatozoids when compared to males with a healthy weight (Du Plessis, S. S., Cabler, S., McAlister, D. A., Sabanegh, E., & Agarwal, A.,2010; Nicopoulou SC et al. 2009). Motility was similar to that found in other studies, with a decrease in patients with obesity, hence showing an association.
Therefore, some of the characteristics in the spermiogram could vary depending on body weight, which in turn has an impact on male fertility.
8. Study Limitations
Our study presents the following limitations: small sample and its retrospective character. Broadening the sample in a prospective study could help define more precisely the relationship between body weight and seminogram alterations.
9. VI.
10. Conclusions
In this study, there is an association between overweight and obese patients and a decrease in seminal quality, which mostly affects sperm count and motility with a higher frequency than in patients with a healthy weight. However, these statistically significant differences found in fresh samples were not found when comparing sperm morphology.
Therefore, given the adverse consequences of obesity and the possible detrimental effect of male BMI in assisted reproduction treatment outcomes, the benefits of reducing body weight should be discussed when counseling interested couples in fertility treatments.
| BMI (kg/m2) | Age | |
| Variable | Mean SD | Mean SD |
| (Min-Max) | (Min-Max) | |
| N | 22,333 | |
| (n=212) | 1,552 | 3,341 |
| (19,487-24,977) | (22,00-40,00) | |
| OW | 26,962 | 32,984 |
| (n=193) | 1,275 | 3,609 |
| (25,00-29,752) | (21,00-40,00) | |
| OB | 34,249 | 32,803 |
| (n=66) | 4,054 | 3,626 |
| (30,043-46,875) | (25,00-40,00) |
| Variable | Median | Mean | Standard Deviation |
| N (n=212) | 100.0 | 111.65 | 70,39 |
| OW (n=193) | 85.0 | 106.17 | 73,47 |
| OB (n=66) | 39.0 | 43.09 | 31,76 |
| Variable | Median | Mean | Standard Deviation |
| N (n=212) | 70.0 | 62.71 | 19,43 |
| OW (n=193) | 65.0 | 60.02 | 20,63 |
| OB (n=66) | 60.0 | 54.97 | 23,66 |
| Year 2020 | ||||
| 27 | ||||
| Volume XX Issue VII Version I | ||||
| D D D D ) | ||||
| ( | ||||
| Medical Research | ||||
| Variable N (n=212) OW (n=193) (n=66) OB | Median 5 5 5 | Mean 1.3390 1.498 1.699 | Standard Deviation 1,3390 1,498 1,699 | Global Journal of |