1. I.
Background nfectious diseases remain a serious public health concern worldwide [1]. Despite the significant increase in the comprehension of the pathogenesis and management of infectious diseases, they remain one of the causes of mortality and morbidity, particularly in developing countries [2]. The indiscriminate use of antimicrobials and the poor management of infections lead to a new upsurge in the loss of drugs and the increase of resistant pathogenic microorganisms in recent years [3]. Approximately 700,000 people died yearly due to antibiotic resistance, and an estimated 10 million lives may be at risk by 2050 if nothing is done to solve the problem of antimicrobial resistance [4]. This situation increases the frequency of therapeutic failures and leads to economic liability, coupled with the undesired side effects of synthetic antimicrobials which complicate treatment [5].
During infection, highly reactive free radical and oxygen species are produced. This leads to high oxidative stress, which can provoke cancer, autoimmune, degenerative, and cardiovascular diseases [6]. Synthetic antioxidants widely used in cosmetics, food, and therapeutic industries are being restricted due to their carcinogenicity [7]. At the time, the current steroidal and non-steroidal anti-inflammatory drugs present adverse side effects [8]. The need to challenge these problems, coupled with the limited number of drugs, motivates the intensive searches for novel, effective, and affordable medicines from different sources [9].
Herbal products are extensively used in African traditional medicine to manage various illnesses [10]. Natural products from plants have been recognized as a reservoir of novel drugs with possible new mechanisms of action [11][12][13]. The use of medicinal plants is increasing worldwide, especially in advanced countries where many people rely on plants as primary healthcare modality due to limited access to modern medicine [15,16].
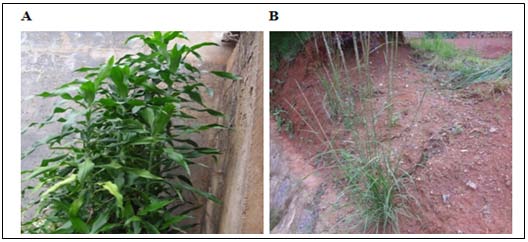
Dracaena deisteliana belongs to the family of Dracaenaceae, which includes more than 480 species distributed, principally in tropical and sub-tropical I regions [17]. The resin of D. deisteliana is used in Arab medicinal tradition to treat diarrhea, fracture, stomach, intestinal fever, and toothache [18]. In Cameroon, D. deisteliana leaf is used to treat infertility [19] and typhoid [20]. The stem is used to treat toothache [21]. In Nigeria, this plant is used to treat cough [22]. The pharmacological properties of D. deisteliana include the antileishmania, anti molluscoidal, antimalarial, antibacterial, and antifungal activities [20,23]. The phytochemical studies of D. deisteliana lead to the isolation of numerous compounds with biological properties [24,25].
S. indicus belonging to the family of Poaceae is a perennial grass that grows in dense tufts. It is represented by approximately 45 species that generally grow in tropical and sub-tropical regions all over the world [26]. The sirup of S. indicus prepared with fruits is used to fight chronic diarrhea. The astringent bark decoction of S. indicus is a medicine against scabies, ulcers, and dysentery. The leaves and bark are used as a febrifuge [27]. However, phytochemical and biological activities of these plants are less or not investigated. Therefore, this study was undertaken to investigate the phytochemical composition, the antibacterial and antifungal, and the radical scavenging properties of D. deisteliana and S. indicus.
2. II.
3. Materials and Methods
4. ) Preparation of Methanol Extracts
The different parts and the whole plant of D. deisteliana and S. indicus were air-dried during two weeks at shade at room temperature. The samples were ground separately in a mortar, and 500 g of dried powder of each sample were soaked for 72 h in methanol (1:10 w/v) with constant stirrings. The resulting supernatant was filtered through Whatman no.1 filter paper and concentrated using a rotary evaporator at 55°C. The resultant extracts were transferred into preweighed labeled glass vials. The process was repeated twice on the marc to exhaustively extract the plant material. The extraction yield of each plant extract was determined by dividing the total extracted mass by dried plant mass used for extraction. Resultant extracts were air-dried and kept at 4°C for further use.
5. c) Phytochemical Screening
Qualitative methods were used to determine different classes of phytochemicals (phenolic compound, tannins, saponins, alkaloids, anthocyanins, terpenoids, glycosides, cardiac glycosides, phlobatannins, and flavonoids), as previously described by Trease and Evans [28], and Sofowora [29] Cryptococcus neoformans). These clinical isolates were obtained as a donation from the Laboratory of Microbiology, Faculty of Science, University of Yaounde I. All strains were cultured 24 h on Mueller Hinton Agar (MHA) for bacteria and Sabouraud dextrose agar (SDA) for fungi before any test. The Mueller Hinton broth (MHB) and Sabouraud dextrose broth (SDB) were used as liquid medium for the determination of the minimum inhibitory concentrations (MICs) and the minimum bactericidal/fungicidal concentrations (MBCs/MFCs). Gentamicin 1 mg/mL (bacteria) and Fluconazole 100 mg/mL (fungi) were used as positive control.
6. ii. Preparation of Microbial Inoculum
The microbial inoculum was prepared using a direct colony suspension method. Suspensions of bacteria and yeasts were prepared in normal saline from 24 h grown on fresh MHA or SDA at 37°C. The bacterial suspension formed was adjusted with a spectrophotometer to a McFarland standard of 0.5, which is approximately 1.5 x 10 8 CFU/mL. The turbidity of fungal strains was adjusted to a standard of 0.9 to give 1-5 x 10 7 CFU/mL. Each suspension was then diluted 1:100 by transferring 0.1 mL of the bacterial suspension to 9.9 mL of sterile MHB while preparing for experiments [30].
7. iii. Agar Well Diffusion Assay for Antibacterial Screening
The antibacterial activity was performed using the agar well diffusion method according to the modified Kirby Bauer diffusion technique [31]. The agar plates were swabbed with overnight bacterial suspensions of each strain. Then, wells were bored into the agar medium with heat sterilized 6 mm cork borer. A 75 ?L of the methanolic extracts (100 mg/mL) was dispensed into the wells, and the plates were left for 30 min before being incubated for 24 h at 37 °C. Each zone of inhibition around the wells was measured using a vernier caliper.
8. iv. Determination of the minimum inhibitory concentrations (MICs) and minimum bactericidal/ fungicidal concentrations (MBCs/MFCs) of the plant extracts
The MICs values of the plant extracts for bacteria and yeasts were determined using serial dilution microplate methods [32,33]. Two-fold serial dilution of the extract (dissolved in MHB or SDB) was made in a 96-wells microplate for a final concentration ranging from 100 to 97.65 x 10 -3 mg/mL. An equal volume (100 µL) of the 1.5 x 10 6 CFU/mL bacterial inoculum or 1-5 x 10 5 CFU/mL fungal inoculum prepared in MHB or SDB was then added. The plates were covered with a sterile plate sealer and then incubated for 24 h at 37°C (48 h for fungi). After incubation, 40 ?L of 2,3,5-triphenyltetrazolium chloride 0.01 % w/v (TTC) was added in each well of the plates and incubated for 30 min at 37°C. The MIC, defined as the lowest sample concentration that prevented the growth of the bacteria, was then detected by any observed color change. The MBCs/MFCs of each fraction were determined by subculturing the sample (50 ?L) taken from the wells without growth during MIC determination to 150 ?L of MHB or SDB. The plates were incubated at 37°C for 48 h (72 h for fungi). The MBC (or MFC) was regarded as the lowest concentration of extracts with the absence of growth that prevented the color change of the medium after the addition of TTC as mentioned above.
9. e) Free Radical Scavenging Assay
The DPPH (2.2-diphenyl-1-picrylhydrazyl) radical-scavenging potential of D. deisteliana and S. indicus extracts was determined following a modified method of Brand-Willians et al. [34]. A 10 ?L of each extract prepared in methanol at different concentrations was added into 1990 ?L of DPPH solution (0.04 mg/mL) in different tubes for final concentrations of 5 µg/mL; 10 µg/mL; 15 µg/mL; 20 µg/mL; 25 µg/mL; 30 µg/mL. After vortexing, the tubes were kept in the darkness at room temperature for 30 min. The absorbance at 517 nm was taken. The percentage inhibition was calculated from [(A 0 -A 1 )/A 0 ] x 100, where A 0 is the absorbance of the control at 30 min (DPPH solution), and A 1 is the absorbance of the extract/reference. Ascorbic acid was used as a reference. The inhibition curves were prepared, and EC 50 (Efficient concentration of the sample (g) to scavenge 50 % of the DPPH free radical) values were calculated.
10. f) Statistical Analysis
Data were represented as mean ± standard deviation (SD) of three replicates and subjected to one way analysis of variance (ANOVA) using the Fisher test at the threshold of p ? 0.05 with Stat graphics plus 5.0 for windows. Linear regression analysis was used to calculate EC 50 values. Microsoft Excel was used to enter and capture data.
11. III.
12. Results and Discussion
13. a) Extraction Yields of the Plant Extracts
The plant material was extracted using methanol as solvent. The highest yield was obtained with D. deisteliana leaf extract (8.89 %). The least yield of extraction was obtained with S. indicus extract (3.46 %) (Table 1). It has been shown that the type of solvent used in extraction procedure determines the success of isolated compounds from the plant material [35]. The yield of extraction of the stem extract of D. deisteliana was 5.63, which is higher than 0.95 previously obtained by Kougan et al. [25]. [36,37]. The phytochemical investigations of D. deisteliana leaf extract by Kougan et al. [25] reported the presence of steroidal saponins and saponins. Anthocyanins and tannins were found in the crude extracts of S. indicus. In a previous study, it has been reported that S. indicus is rich in tannins [27]. Several classes of secondary metabolites found in these plant extracts have been reported to posses' antimicrobial activities [38][39][40].
14. Medical Research
15. c) Diameter of Inhibition Zones
The presence of inhibition zones after incubation showed that the Gram-positive, Gramnegative, and fungi isolates exhibited a varied degree of susceptibility to each of the plant extracts that can be considered as a plant with a broad spectrum of activity (Table 3). Considering the susceptibility of the isolates to D. deisteliana, the inhibition zones ranged between 8.5 ± 0.28 (K. pneumoniae) and 15 ± 0.57 mm (K. oxytoca and E. coli) for the leaf extract while no activity was noted on B. cereus and P. aeruginosa. In the previous report, the leaf extract of D. deisteliana exhibited the inhibition zones of 8.5 ± 00 mm (80 mg/mL) and 12 ± 00 mm (160 mg/mL) on S. typhi [20]. The stem extract The results are expressed as means ± standard deviation of three determinations. Values with different letters in the same line are significantly different at p?0.05.
16. d) Minimum Inhibitory Concentrations (MICs) and Minimum Bactericidal/Fungicidal Concentrations (MBCs/MFCs)
In this study, the extracts obtained from both the plant extracts displayed varying antimicrobial activities according to their MICs (6.25-50 mg/mL for bacteria and 1.56-50 mg/mL for yeasts) as reported in Table 4. The leaf and the whole plant extracts of D. deisteliana were the most active (MIC = 6.25 mg/mL) against E. cloacae and E. coli (Gram-negative) while both bacteria had the same degree of susceptibility (MIC = 50 mg/mL) to the stem extract. The whole extract of S. indicus (MIC = 6.25 mg/mL) had remarkable activity against B. cereus (Gram-positive). The sensitivity of Gram-negative and Gram-positive bacteria could be due to the difference in their membrane morphology [41]. The phospholipidic bilayer of the outer membrane of bacteria is the target of interactions with antimicrobial compounds. Damages on the bacterial membrane could increase permeability to ions, the release of intracellular constituents, deterioration of the enzymatic system of bacteria, and even dead [42,43]. All the tested extracts of D. deisteliana were most active on C. albicans and C. krusei (MIC = 1.56 µg/mL). A similar activity was observed with the leaf and the whole-plant extracts on C. parapsilosis. C. neofarmans had the least susceptibility (MIC = 50 µg/mL) to all the extracts of D. deisteliana. The antimicrobial activity can be classified as interesting (CMI < 100 ?g/mL), moderate (100 < CMI < 625 ?g/mL) and weak (CMI ? 625 ?g/mL) [44,45]. Therefore, all the plant extracts have weak activity on the tested microorganisms. The weak antibacterial activity exhibited by all the plant extracts could be correlated to the few amounts of secondary metabolites since it has been proven that the concentration, the nature, and the origin of active compounds present in plant extracts may influence the antimicrobial activity [40,46]. The antimicrobial mechanism of active ingredients may vary with species, chemical composition, cell wall composition, and genetic material of each microorganism [38,41,47].
According to Mims et al.
[48], the leaves extracts of D. deisteliana had a bactericidal effect on S. aureus, K. pneumoniae, B. cereus, and K. oxytoca. In comparison, the stem extracts had bacteriostatic effect on S. aureus, K. pneumoniae, E. cloacae, and E. coli. The whole-plant extract of D. deisteliana exhibited a bactericidal action on S. aureus, K. pneumonia, and B. cereus. At the same time, the bacteriostatic effect was was less active on K. pneumoniae with inhibition zone of 11 ± 00 mm and exhibited higher activity on E. cloacae with inhibition zone of 18 ± 00 mm. The inhibition zones varied between 9.5 ± 0.28 (K. pneumoniae) and 16.5 ± 0.28 mm (E. cloacae) for the whole plant extract. This study provides additional data on the antimicrobial activity of D. deisteliana. The whole extract of S. indicus exhibited inhibition zones varying between 7 ± 00 (E. coli) and 14 ± 0.43 mm (Acinetobacter spp). These results revealed for the first time information on the antimicrobial properties of S. indicus. Nevertheless, the antibacterial activity of both the plant extracts was less pronounced compared to the standard antibiotic (gentamicin) with inhibition zones varying between 21 ± 00 and 29.67 ± 0.88 mm. observed on K. oxytoca, E. cloacae, and E. coli. The whole-plant extract of S. indicus exhibited a bacteriostatic effect on K. pneumoniae, E. coli, B. cereus, and P. vulgaris while the bactericidal effect was observed on the rest. All the extracts of D. deisteliana have a bactericidal effect on all the yeast strains used in this study.
17. Medical Research
18. S. indicus
19. Ascorbic acid e) Antiradical Properties of Plant Extracts
The free radicals scavenging properties of the plant extracts are reported in Figure 2. The crude extracts of D. deisteliana and S. indicus exhibited radical scavenging properties in concentration-dependent manners. The inhibition percentages of the stem (26 %) and the whole plant extract of D. deisteliana (28 %) and S. indicus (24 %) were most pronounced than that of the leaf extract of D. deisteliana (14 %) at the concentration of 1 mg/mL. The higher inhibition percentage was observed with the stem extract of D. deisteliana (62 %) at the concentration of 5.5 mg/mL. It can be observed that the DPPH activity D. deisteliana and S. indicus were found to be increasing in concentration-dependent manner.
From each graph, the EC 50 of each extract was determined. The EC 50 is the concentration of the samples, which scavenges 50 % of free radicals. Figure 3 shows the scavenging activity of the crude extracts of D. deisteliana and S. indicus in comparison with that of ascorbic acid. The EC 50 obtained showed that among the crude extracts of D. deisteliana, the leaf extract exhibited the lowest activity (646.75 µg/mL), while the stem extract had the higher one (491 µg/mL). The whole plant extract of S. indicus had an EC 50 of 550.5 µg/mL, while the EC 50 value of the standard was found to be 411 µg/mL. Numerous previous studies show the correlation between antiradical activity and the phenolic compounds [49]. These studies have confirmed that the phenolic compounds contribute significantly to the antioxidant activity [50]. The antiradical activity depends on the content in phenolic compounds that give up hydrogen to the free radicals and interrupt the chain of lipid oxidative reaction in the first step of inhibition [51]. This higher efficiency of the phenolic compounds to scavenge free radicals like singlet oxygen, superoxide, and hydroxyl radicals is due to their hydroxyl phenolic group [52]. Flavonoids and tannins found in these plant extracts possess a large spectrum of antiradical properties [53]. However, these activities may be due to
20. Ethics approval and consent to participate
Not applicable
![the synergistic action of the chemical compounds presents in the extracts[54].Phytochemical Analysis, Antimicrobial and Radical Scavenging Properties of Methanol Extracts of Dracaena Deisteliana(Dracaenaceae) and Sporobolus Indicus(Poaceae)](https://medicalresearchjournal.org/index.php/GJMR/article/download/2199/version/102100/6-Phytochemical-Analysis-Antimicrobial-and-Radical-Scav_html/33848/image-8.png)

| d) Antimicrobial Assays | |||
| i. Microbial Strains and Culture Media | |||
| Twelve bacteria including ten Gram-negative | |||
| (Enterobacter cloacae, Klebsiella oxytoca, Klebsiella | |||
| pneumoniae, Morganella morganii, Bacillus cereus, | |||
| Escherichia coli, Proteus vulgaris, Citrobacter freundii, | |||
| Pseudomonas aeruginosa, Acinetobacter sp) and two | |||
| Gram-positive | (Staphylococcus | aureus | and |
| Streptococcus faecalis) and four yeasts (Candida | |||
| albicans, Candida krusei, Candida parapsilosis, and | |||
| Plant | Part used | Solvent used | Yield of extraction (%) |
| Leaf | Methanol | 8.89 | |
| D. deisteliana | Stem | Methanol | 5.63 |
| Whole plant | Methanol | 6.37 | |
| S. indicus | Whole plant | Methanol | 3.46 |
| b) Phytochemical Screening |
| Plant constituents | D. deisteliana | S. indicus | |||
| Leaf | Stem | Whole plant | |||
| Phenolic | Ferric chloride test | + | + | + | + |
| Potassium dichromate | + | + | + | + | |
| Tannins | Ferric chloride test | - | - | - | + |
| Anthocyanins | Ammonia HCl test | - | - | - | + |
| Saponins | Frothing test | + | + | + | + |
| Flavonoids | Alkaline reagent test | +++ | ++ | ++ | + |
| Lead acetate test | + | + | + | + | |
| Alkaloids | Tannic acid test | + | + | + | + |
| Mayer's test | + | + | + | + | |
| Wagner's test | + | + | + | + | |
| Terpenoids | Salowski test | +++ | ++ | ++ | + |
| Anthraquinones | Borntrager's test | + | + | + | + |
| Glycosides (Free sugar) | Legal's test | - | - | - | - |
| Cardiac glycosides | Killer Killani test | - | - | - | - |
| Phlobatanins | Hydrochloride test | - | - | - | - |
| +++ = abundant; ++ = moderate ; + present ; -completely absent | |||||
| D. deisteliana | ||||||
| Microorganisms | Parameters | S.indicus | ||||
| 1 | 2 | |||||
| B. cereus | MIC | 25 | 25 | 25 | 6.25 | 0.19 |
| MBC | 50 | 100 | 50 | 25 | 0.39 | |
| MBC/MIC | 2 | 4 | 2 | 4 | 2 | |
| K. oxytoca | MIC | 25 | 25 | 25 | 25 | 10 |
| MBC | 50 | 100 | 100 | 25 | 20 | |
| MBC/MIC | 2 | 4 | 4 |