1.
Introduction lso known as Acne inversa or the Verneuil's disease, Hidradenitis suppurtiva is a chronic disease with recurrent abscess formation progressing to sinus tracts and resultant scarring. It was first described by Velpeau in 1839during his study involving the origin of abscess involving the sebaceous follicles in axillae [1] It is commonly seen in females and also incidence involving the axilla in both sexes is nearly equal.
Commonly seen in adolescents, it initially presents like a comedo and progresses with mucopurulent discharge eventually leading to scarring.
2. II.
3. Epidemiology
? Prevalence: 1 in 300 adults Stage 3: Diffuse or broad involvement across a regional area with multiple inter-connected sinus tracts and abscesses. Significant scarring is seen and fistula formation is present.
IV.
4. Imaging
Imaging evaluation is initially indicated to evaluate the extent and the feasibility to obtain image guided aspirate for culture and sensitivity. A simple ultrasound guided aspiration of the involved part can be used to obtain sample for culture and sensitivity if secondary infections are suspected when there is no sinus tract to directly obtain swabs. [3] MRI is the preferred modality for evaluating the extent of disease as well as follow up.
V.
5. MRI Spectrum
The protocol
The MRI of the involved area is best suited to evaluate the extent of disease and also may help in monitoring treatment response. The MRI findings parallel with the clinical features therefore avoiding any clinical confusion. STIR (Short tau inversion recovery) and T2W sequences are recommended protocol.
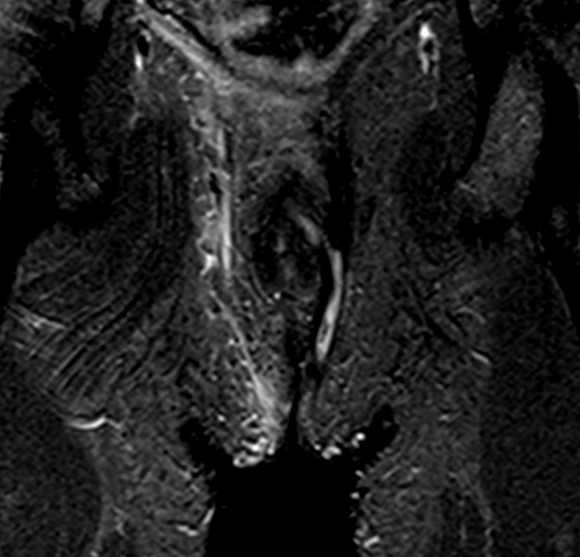
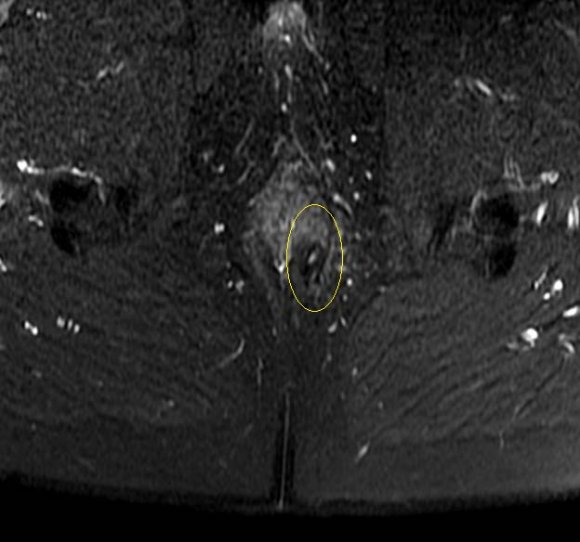
It may initially just show thickening of the skin and subcutaneous tissue which soon progresses to induration best seen on routine T2W and STIR images as subdermal hyperintense signal extending upto skin. In a few days there is formation of subcutaneous abscesses however the disease is confined to the skin and subcutaneous tissue. Rarely there is fistulous communication with bladder urethra or rectum etc. in patients with highly virulent infection or compromised immune status like diabetes.
Reactive inguinal lymph nodes are also seen in conjunction.
Post treatment cases demonstrate residual scarring as STIR hypointense tracts. (Refer figure D) VI.
6. Differential Diagnosis
Carbuncles, Lymphadenitis, Infected Bartholin's cyst, sebaceous cysts, Cellulitis/ erysipelas, Lumbosacral epidural abscess are few of the common differential diagnosis which can be easily ruled out combining the imaging and the clinical picture. [4] VII.
7. Sequelae
Various sequel can be strictures, disfiguring edema, arthropathy and chronic cases may undergo metaplasia and even lead to squamous cell carcinoma.
8. VIII.
9. Treatment
Treatment of HS is directed according to disease severity. Aim is to alleviate symptoms and improve quality of life. Many a times combination therapy is resorted. a) Anti-inflammatory Agent [5] ? Intralesional steroids: Triamcinolone acetonide 2-5mg/ml can be used for few lesions
? Anakinra: An IL-1 inhibitor (100mg SC/day for 12 weeks) showed reduction in severity of disease
? Antibiotics: Many topical and oral antibiotics like clindamycin(1%;300mg BD), tetracycline, rifampicin(300mg BD); have been used alone or in combination for their anti-inflammatory and immunomodulatory properties. [6] A study of hyperbaric oxygen therapy with antibiotic combination showed good improvement in sartorius and DLQI score. [7] Antiandrogens: Although anecdotal in females, a double blinded study in women with Cyproterone acetate(100mg) and Ethinyl estradiol(50 micrograms) as per reversed sequential therapy laid down by Hammerstein and Cupceancu, showed reduced discharge and swelling. [8] Finasteride(5-10 mg/day) used primarily for prostate cancer showed good results in pediatric patients. [9]
10. b) Retinoids
Isotretinoin worked in patients with mild disease when given in low doses 0.5-1.2 mg/kg/day over 4 to 12 months. [10] A study of Acitretin (0.6mg/kg/day) over 6 to 12 in 12 patients with moderate to severe disease showed improvement. [11] The mechanism of action is through the keratolytic action thereby reducing ductal occlusions.
11. c) Immunosuppresive therapy
Cyclosporine (4.5mg/kg/day) showed raid relief in resistant cases to antibiotics and UVB therapy. [12] TNF? inhibitors have been proven to be quite effective in Hurley's II and III stages of the disease.
Infliximab 5mg/kg IV at week 0, 2 and 6 were given to 33 patients; drug was well tolerated and showed good improvement in symptoms and severity of the disease. [13] Etanercept showed varied results when administered twice weekly 50mg for 12 weeks.
Adalimumab when given weekly instead of fortnightly showed superior results when 4 randomized control trials were analysed. [14,15] Apremilast a selective phosphodiesterase 4 inhibitor (30 mg BD); used primarily for psoriasis; showed moderate results. [16]
12. d) Miscellaneous
Botulinum toxin reduces acetylcholine release and in turn reduces the sympathetic activation of apocrine glands. A dose of 40 to 50 Units per session for 3 to 4 times over 3 years reported remission in 4 cases. [17,18] Metformin helps in decreasing androgen sensitivity by lowering circulating insulin and helps in managing the metabolic syndrome associated with disease. [19] Others: Zinc, Cryotherapy and Photodynamic therapy e) Surgical Intervention This is the last resort to unresponsive cases. Deroofing is most effective in combination with antibiotics and anti-inflammatory. [20] f) Laser therapy Nd: YAG laser in 22 patients showed significant improvement in all (65%), axilla (62%), Inguinal (53%), Inframammary (51%). [21] Carbon dioxide laser for lesions to heal by secondary intention has also been tried. [


| Clinical Classification: Hurley stages-3 well delineated | |
| stages have been described by Hurley emphasizing the | |
| clinical diagnosis. | |
| Stage 1: | |
| ? Sex predilection: Females > Males | |
| ? Onset: Adolescent to middle age | |
| ? Family history: Positive family history with an | |
| autosomal-dominant mode of inheritance | |
| ? Associations: Crohn's disease, Dowling Dego's, | |
| Arthropathy (SAPHO), Smoking, Obesity, Hormonal | |
| influence [2] | |
| III. | pathophysiology |