1. Introduction
s of now, the COVID-19 pandemic is a bane to the entire world populace, because of the pace of infectivity, inclined danger of acquiring the airborne viral disease and combined with the way that there is as of now no endorsed corrective control/vaccine for this viral infection. Arrays of investigations have set up that the general population most predisposed and powerless against the ailment are the older individuals, males, people with hidden sickness conditions including; hypertension, diabetic condition, immuno-weakened people, and people dependent on immunosuppressant use [1]. Equally, considering the already infected populace, the possibility of being asymptomatic could vary, contingent upon the conditions and populace, going from 5% to 80% [2]. Three likely method of spread have been portrayed through droplet transmission, express contact spread, via airborne transmission. By and by, of late the digestive tract has additionally been demonstrated as a likely method of spread dependent on abdominal clinical indications and manifestation of diarrhea brought about by the viral infection, just as the viral RNA saw in faeces [3]. Various elements may control the infection's transmission given the infectivity levels of the host, for example, sanitary behaviours including quarantine, hand washing, and appropriate routine care which are needed to soothe the affinity of the viral infection and infectivity. It has been definite that community wellbeing mediation that stifles over 60% of transmissions are productive to deal with the concealment levels of the COVID-19 pandemic [3].
The term herd immunity was initially utilized in 1923 by Topley and Wilson [4]. It subsequently gave the need to vaccines and their purposes, vaccine program expenditure efficacy-breakdown, and the concealment of ailments, for example, smallpox and different irresistible diseases like polio and diphtheria [5,6,7]. Herd immunity is additionally affected by elements, for example, populace immunity and the methods of the spread of causal agents [6,8].
Divergent investigations have broke down the helpfulness of vaccination projects to accomplish herd immunity in, and in this way shield the unvaccinated against different maladies [9]. The primary embodiments are the immunizations for cholera, hepatitis A, hepatitis B, human papillomavirus, haemophilus flu, meningococcal, flu, pneumococcal, polio, challenging hack, measles, chickenpox, rotavirus, and yellow fever [10,11,12,13] a few of which are represented in Table 1. The ramifications of herd immunity on the viability of infection transmission were as of late observed in America with the Chikungunya and Zika infections, which caused a pandemic in an altogether weak populace. By and by, after the surge of these arboviruses, herd immunity confined their spread [14]. In like manner, the United Kingdom of late executed a plan for the COVID-19 pandemic that caused controversy, giving space for the infection to be transmitted in the populace before charging social seclusion to boost herd immunity [15]. Deriving the orderly model of group immunity as the resistance that a specific populace has against a disease, Fox and his partners itemized four conditions under which such resistance can happen [20]. Initially, the transmittable microbe must be traced, found and restricted to a solitary host. For extreme intense respiratory disorder Covid 2 (SARS-Cov-2), the central method of spread was zoonotic in nature, with its essential host being the bat. Notwithstanding, the intermediary host through which it was transmitted to people is conditional. Transmission is known to have happened because of express contact with the contaminated animals or via their secretory liquids. Viral RNA has additionally been built up in canines and felines living with COVID-19 positive people. However, it has not been uncovered that these creatures can pass on the infection to individuals [21]. Also, the spread must happen predominantly through direct contact. Up till now, it has been standard that the spread of COVID-19 by direct individual-to-individual contact by means of coughing, sneezing, and inward breath of polluted vaporizers and contact spread through the oral, nasal, and ocular membranes [22].
With specific accentuation on the data lacking on the immune reaction incited by COVID-19 in people, it's been difficult to set up the methods by which the immune system make a drawn out response that could fight the viral infection and deflect disease relapse. At last, group immunity is exploited if the populace procure a laid-back integration model. With this situation, everybody is defense-less against getting contaminated with COVID-19 bringing to the fore its inalienable indications. By and by, this plan of laidback blending will rely upon the preventive rules executed by every nation's administration overall which involves quarantine, seclusion, social separation, and fortified pre-emptive rules for in danger gatherings, for example, pregnant ladies, the old people, and youngsters [23]. Hypothetically, it is likely to achieve group immunity under the expressed speculations. In any case, by and by absence of intrinsic comprehension of the adaptive immune response and, in the non-existence of an appropriate vaccine, the moral limitations to achieve such immunity make this cure excessively deceptive to preliminary [24].
2. a) Creating herd immunity within populations
To make herd immunity inside a populace, the immunity achieved by immunization or natural infection must be turn away ahead spread of infections. For SARS-CoV-2, clinical signs are a helpless marker of transmissibility, as asymptomatic hosts can be exceptionally transmittable and add to the spread of an epidemic [25]. For microorganisms in which deep rooted immunity is prompted, similar to the case for measles immunization, herd immunity is significantly efficacious and can turn away microbe spread inside a populace. Nonetheless, this circumstance is sensibly atypical, as immunity for some infectious diseases, for example, pertussis and rotavirus, fade in the long haul [25]. Subsequently, herd immunity is less productive and discontinuous outbreaks can still surface. Eventually, if immunity is unpredictably spread in a populace, gatherings of disease-prone hosts that can frequently interact with one another may continue.
3. b) Herd immunity efficiency for COVID-19 transmission suppression
As indicated by the WHO, herd immunity is basically serviceable for communicable diseases [26]. For transferable infections, however, the immunecompetent people must not exclusively be protected yet C there is the need of likewise decreasing disease among immununo-suppressed hosts through herd safeguard [27]. Attributable to herd protection, various maladies can be eradicated without 100% vaccination presentation. For a valid example Haemophilus influenzae type B vaccine introduction of under 70% in Gambia was adequate to eliminate Hib disease, with equal findings in Navajo populaces [28,29].
For COVID-19, herd immunity, with its relatively inherent effect, probably won't facilitate the infection as the outcomes rely upon the case and adequacy of the control measures and the ability to bring at the same time mounting outbreaks under instant control when required [30]. Antibodies for this infection are not yet accessible, however existing chemotherapeutic synergistic utilization, for example, azithromycin (AZT), hydroxychloroquine sulfate, chloroquine phosphate has been viewed as likely valuable. Regardless, their handiness and safety are built up in extra investigations for this novel malady [31,32,33].
4. III.
5. Specifics of Herd Immunity and Covid-19
The current COVID-19 pandemic has produced over 81 million of clinically established cases and has claimed an absolute number of more than 1.7 million lives worldwide as of 31 st December, 2020. A few exploratory preliminaries to evaluate novel immunization varieties and medication reconstituting approaches for the prevention and fixing of COVID-19 disease are directly in progress. Regardless, it is inconclusive whether these preliminaries will produce valuable cure, and it is dubious how broad these examinations will take albeit a positive assessment for any immunization preliminary is in any event 12 to year and a half. In the inaccessibility of an immunization, developing of COVID-19 herd immunity through common disease is still theoretically possible.
6. a) Epidemiological considerations for COVID-19 herd immunity
Inconsistency in method of spread between people may assume a key part in COVID-19 dispersal. Super-spreading occasions happen when conditions positive for high paces of transmission emerge. These occasions include a solitary index case infecting countless secondary contacts and are known to be significant in driving episodes of infectious diseases, including SARS, MERS, and measles [34]. Reports of COVID-19 super-spreading occasions have been recorded, recommending that heterogeneity in infectivity may essentially affect the elements of its transmission [35]. At long last, the variables that impact interindividual heterogeneity in COVID-19 vulnerability, clinical pathology, and disease result are not surely known.
7. b) Immunological antibody responses to COVID-19
Following contamination with COVID-19, perceptible IgM and IgG antibodies create inside days to weeks of symptom onset beginning in most infected people [36,37,38]. Why a few patients appear not to build up a humoral immune reaction, as reflected by recognizable antibodies, is dubious. Adding to this vulnerability is the indistinct connection between antibody reaction and clinical improvement. The observations from a small investigation of 9 patients with COVID-19 found that more prominent clinical severity delivered higher antibody titers [36]. Be that as it may, antibody recognition and higher titers have not generally been found to correspond with clinical improvement in COVID-19 [37,38]. Additionally, mild COVID-19 symptoms can resolve earlier detection by IgM and IgG antibodies, albeit distinguishable IgM and IgG antibodies have heralded decreases in COVID-19 viral loads [37,38]. What appears more certain is that viral load regularly peaks from the get-go in infection, and afterward declines as antibodies sprang up and antibody titers ascend over the resulting 2 to 3 weeks [37,38]. The stability of neutralizing antibodies (NAbs, principally IgG) against COVID-19 presently can't seem to be characterized; ingenuity as long as 40 days from symptom onset has been depicted [36].
8. IV. Applications of Herd Immunity in the Current Covid-19 Pandemic
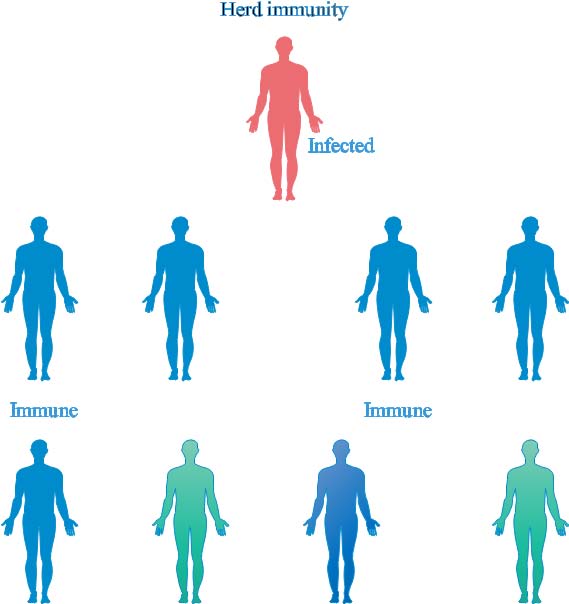
As per various models applied to infectious diseases, herd immunity is mathematically-connected with the spread and infection inclinations of the virus [39,40] as displayed in the herd immunity network in Figure 1, which are the consequence of the relationship set up over a specific timeframe between the number of healthy subjects and those vulnerable to infection, the infected subjects that can no longer add to the transmission of the infection, infected subjects, and the normal or vaccine-immune subjects in a populace, mediated by the infectiousness of the virus, the incubation time frame, the transmissibility period, the virus limit between individuals, the elements of contact among the populace, and the term of the viral disease [41]. Hardly, any investigations describe children as key cases in familial groups [42,43], and plainly, children all the more regularly have asymptomatic diseases when contrasted and grown-ups [33,43,44]. It is of dire significance in demonstrating the pandemic to attempt cautious surveillance, including asymptomatic children and velocity of infection dependent on serology, to more readily describe disease in children and their part in transmission frameworks. Regardless of whether diverse control guidelines decelerate, in the end halting the local spread of COVID-19 infection, the effective containment of this infection actually leaves the populace in danger of resurgence because of deficient acquisition of immunity. In the event that herd immunity can be actuated, it would go about as a boundary to stop the spread of disease [45]. Additionally, vaccines, variable susceptibility and exposure to a great extent establish herd immunity.
Immunization of children to instigate herd immunity has demonstrated efficacy in forestalling the spread of numerous infectious diseases, where children have a critical part in transmission. An elevated level of immunity in one age gathering, who assume a function in transmission, can create herd immunity for others [46], and it is obvious that vaccine inoculation of children is more successful than immunization of old individuals, in specific circumstances, as exhibited in vaccination against flu [46,47], pneumococcal infection [48], rotavirus [19] and numerous others. It is imperative that the overall function of various age cohorts in transmission must be considered. The backhanded advantages of COVID-19 vaccination in children may give or make some assured protection to more established, unvaccinated populaces. At the point when children are immunized, it will be simpler to accomplish enough immunity required for general protection in a given populace.
Coronavirus mortality is emphatically age-ward, and Africa has a similarly more youthful populace than other continents [49]. Consequently, children may be a significant objective for mediations pointed toward decreasing transmission in nations with youthful populaces, particularly since access through school vaccination might be more direct than getting to grown-ups. Despite the fact that the need for COVID-19 immunization would legitimately be for that at the most noteworthy danger of infection, for example, medical services labourers, and those at the most elevated danger of severe infection, for instance, older adults, vaccination of children might be another critical cohort for their own safeguard and to help herd immunity. a) Herd immunity constraints in the current covid-19 pandemic Herd immunity might be accomplished when the populace is exposed to the infection and develops a characteristic immune reaction and somatic defense system to the infection or when the populace is vaccinated against the COVID-19 malady to accomplish immunity along these lines, by vaccinating certain cohorts of the populace, the spread of the infection will go down. Without an immunization, building herd immunity against COVID-19 through natural infection is hypothetically conceivable. Be that as it may, there is no ethical way to arrive at this objective, as the social results of characteristic natural exposure might be overwhelming [42].
Without a doubt, current mathematical and epidemiological examinations propose that herd immunity through common methods may not be the response to stop the novel coronavirus; exposure to the viral infection ought to be maintained until either an immunization or viable pharmacological medicines are accessible. Hence, pharmacological Interventions (PIs, for example, the utilization of hydroxychloroquine, azithromycin, lopinavir, ritonavir, ribavirin, chloroquine phosphate, and arbidol, have been proposed to be conceivably compelling in fighting COVID-19 once the infection's hereditary arrangement and component of infection are unchangeable [50]. Notwithstanding, the adequacy and efficacy of these competitor drugs in the treatment of COVID-19 should be affirmed in further preclinical and clinical preliminaries, in spite of the in vitro examinations and non-clinical preliminaries previously available [51].
9. V. Group Immunity and Vaccination in Covid-19 Transmission Supression
Vaccine development could help halt the spread of the infection, particularly among the most susceptible populaces. This objective has become the procedure most seriously sought after by worldwide research facilities [52,42]. Immunizations have generally been viewed as a type of a preventive mediation for immediate and aberrant protection for herd immunity in an comprehensive populace Reformist vaccination missions and enhancements in complete disinfection in metropolitan settings have assisted with improving herd immunity [53]. Note that vaccination is additionally balanced by vaccine type, the individual life form reaction, anticipation program adherence, and the age of administration [54].
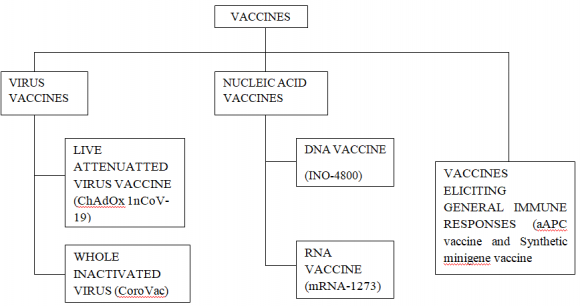
Vaccines train the body to perceive and battle a particular microbe. The viral spread is confined when the immunization rate or the commonness of a high level of positive serological people in the populace truly limit the transmission of the infectious agent starting with one human then onto the next. Building up a "basic" populace immunity rate to control the expansion of COVID-19 is, with current logical information simply theoretical. Moreover, the mass immunization of billions of individuals could be one of the most significant worldwide challenges of the 21st century [15]. Presently, 25 vaccines are being created to battle COVID-19, with subsidizing chiefly originating from private drug foundations. Figure 2 shows the varying vaccine choices presently being investigated. Some research groups are utilizing inactivated viruses, however most investigations on vaccine varieties center around vaccinations dependent on viral proteins and nucleic acids. As recently detailed, COVID-19 is particularly hazardous in individuals of cutting advanced age or with existing underlying conditions, for example, diabetes, coronary issues, malignancy, or a weakened immune system. Other natural elements, for example, diet quality, inactive way of life, and clinical medicines, may likewise restrict the immune reactions of most weak individuals before future vaccine administration against COVID-19. Thusly, herd immunity might be the most significant "present moment" technique to secure this segment of the population (55). Until a safe vaccine is ultimately developed, research on definite novel treatments (or an efficient blend of existing treatments), together with action plans to contain the spread of the virus, seem to be the only substitute for protecting atrisk populations [56].
Discovering an efficient vaccine will not be without firm challenges to surmount, such as its resultant effects, price and ease of accessibility, limited secondary effects to vulnerable people, long-term immune response, and the keenness of the population to be vaccinated voluntarily [27]. There are certain limits to swaying people to engage in mass vaccination [57], even when direct immunization could safely extend indirect immunity to the most vulnerable populations [58,59]. However, public communication plans on the importance of herd immunity and easily accessible vaccination campaigns will be necessary to increase observance to prevention programs in the fight against the COVID-19 infection [60].
10. VI.
11. Conclusion
Among humans, the novel COVID-19 spread happens by direct person-to-person contact via coughing, sneezing, and inhalation of droplets/infected aerosols and contact spread with the oral and nasal membranes. Herd immunity has expansively been used for the containment of multiple diseases and presents the basis for vaccines and their relevancies. The communicable pathogen has been discovered, but the transitional host is still undecided. Additionally, there should be long-lasting immunity, which is still feasible for COVID-19. With no vaccine in view, cluster immunity is likely to be attained when about 70% of the people has been infected. Diverse forms of vaccines are in advance stages of formulation worldwide in order to curb the scourge of the virus. The COVID-19 pandemic could only end if a clinically-safe, tested and effective vaccine is confirmed, with the concept of herd immunization acquired and embraced. Finally, pending the availability of a vaccine, epidemic spread suppression via exceptionally-concentrated health criterions potentially shows to be the workable and secure plan, implementing quarantine and the application of numerous contact with wherewithal management to suppress the spread of the virus.
| Viral vaccines | Age range (yrs) of vaccine coverage | Sample population | Vaccination recipients | Percentage herd immuned reduction of | Location/year References | |||
| Seven-valent | <5 (vaccinated) | 851 | 2,105 | 98% reduction | UK/2006 | [16] | ||
| pneumococcal | >65(not | 1812 | 85% reduction | [16] | ||||
| conjugate | vaccinated) | |||||||
| vaccine (PCV7) | ||||||||
| Measles | 18 | months | 3,115 | 2,105 | 85% reduction | Australia/2005 | [17] | |
| conjugate | (neonates) | 100% reduction | [17] | |||||
| vaccine (MCV) | 10-13 (congenital) | 12,855 | 12,853 | |||||
| Live attenuated | 4-12 | 15,721 | 9021 | 60% reduction | Canada/2008 | [18] | ||
| influenza | 86% vaccinated | |||||||
| vaccine (LAIV) | 14% unvaccinated | |||||||
| Rotavirus | 0-4 | 66,000 | 64,000 | 15% reduction United States/2008 | [19] | |||
| vaccine | 5-14 | |||||||
| (Rotarix) | 15-24 | |||||||
| II. | Elements of Herd Immunity in a | |||||||
| Population with Covid-19 | ||||||||