1. Background
n the United States, there are approximately 1.4 million transgender adults, which makes up 0.6% of the population. 1 Commonly viewed as the "final stage" in the female to male transition, genital surgery has rapidly moved from a metoidioplasty to a phalloplasty operation. Reasons for this change are because of the micropenis appearance of the metoidioplasty and subsequent inability for penetrative intercourse which may contribute to continued gender dysphoria in the patient. Genital surgery can be performed at the age of 18 adhering to guidelines set forth by the Standards of Care for the Health of Transsexual, Transgender, and Gender-Noncomforming People, Version 7. 2 Our main goals in the construction of a phallus for transgender men are to treat their gender dysphoria, allow the patient to have intercourse with their constructed phallus, allow for erogenous sensation and orgasm, allow the patient to urinate in the standing position through their constructed phallus, create an aesthetically pleasing phallus which has tactile sensation and will allow for the placement of a prosthesis without complications. As our surgical technique has advanced, so have the patients' desires. A study reported that more than 98% of transmen desiring phalloplasty reported a desire to stand to void. 3 Although varied options exist for nonautologous tissue, such as packers, external prosthesis, and an osseointegrated epithesis, they have multiple limitations regarding urination, sexual function, and appearance. 4 Similar techniques used in cis-gender male phalloplasty have been used for transgender men. Flaps, such as the tube-in-tube radial forearm flap, osteocutaneous radial forearm flap, scapular flaps, deltoid flaps, abdominal pedicled flaps, and anterolateral thigh flaps have all been used for phalloplasty. 5,6,7,8,9,10 To date, the free radial forearm flap continues to be the most commonly used tissue for cis and transgender phalloplasty due to its superior erogenous and tactile sensation including versatility in the inset. The urethral portion of the phalloplasty construction remains the portion fraught with the most unfavorable outcomes in this very complex procedure. The urethra after phalloplasty construction can be divided into distinct segments, from proximal to distal: native (female) urethra, fixed urethra, anastomotic urethra, phallic urethra, and meatus. 11 The fixed urethra is the portion of the urethra formed after lengthening the native urethra via local vaginal or labial flaps, extragenital flaps, and grafts of skin or mucosa (Figure 1a and b). 12 The phallic urethra can be constructed through a variety of techniques, including prelamination, tube-in-tube techniques, and pedicle flaps . 13,14 Urethrocutaneous fistulas are the most common urethral complication following surgery with rates ranging from 22% to 75%. 15,16,17 Fistulas occur most commonly at or just proximal to the anastomosis between the phallic urethra and fixed urethradue to vascular insufficiency of the flap, and the decreased lumen of the phallic urethra. At our institution, we have significantly decreased our fistula rates in transgender male phalloplasty by augmenting the paucity of vascularized tissue at this anastomosis using a pedicled gracilis flap at the time of flap transfer. 18 Urethral strictures are an equally as common untoward event following phalloplasty in transgender men with rates ranging from 11-74%and their subsequent management can be challenging. 19,20,21 To decrease unfavorable urologic sequelae following phalloplasty, surgeons have used mucosa, which has characteristics more like uroepithelium, for the urethral reconstruction. Burger used buccal mucosa grafts, which remains the mainstay for the reconstruction of the urethra. 22 Zhang specifically looked at female to male transgender phalloplasty and found vaginal mucosa graft to be an excellent material for urethral reconstruction in patients undergoing phalloplasty. These findings, of a decreased urethra fistula and stricture rate, influenced our conversion to a two-stage radial forearm phalloplasty and flap neourethra prelamination with mucosa (buccal, vaginal, or uterine) that was evaluated in this manuscript. 23 II.
2. Material and Methods
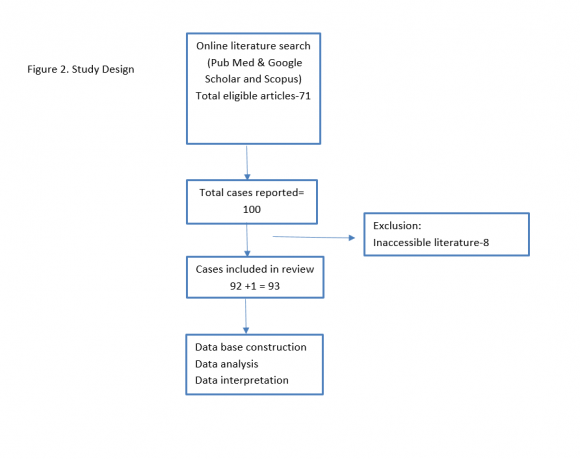
A retrospective review of transgender male patients undergoing phalloplasty between June 2016 and June 2019 was conducted. Inclusion criteria included age over 18, surgical treatment for gender dysphoria with two-stage radial forearm phalloplasty, and flap neourethra prelamination with mucosa (buccal, vaginal, or uterine). Exclusion criteria included patients opting for single stage tube-in-tube phalloplasty construction, skin graft only prelamination of the neourethra, and cis-male patients undergoing reconstructive phalloplasty.
Patients were identified for inclusion on review of a prospective list of patients treated by the senior author. Charts of patients meeting criteria for inclusion were reviewed for demographic data and complete medical and surgical history. Date of birth, body mass index (BMI), history of or active tobacco use, as well as co-morbid medical conditions were recorded. Operative notes of the phalloplasty procedures were reviewed with the following data recorded: date of operation, tissues used in prelamination including the type of mucosa, neurovascular structures anastomosed during free tissue transfer, and augmentation of the urethral anastomosis with a gracilis muscle flap. Post-operative records were reviewed and final constructive outcomes including length of the phallus as well as complications were recorded.
3. a) Vaginectomy and Flap neo-urethra prelamination (Stage I)
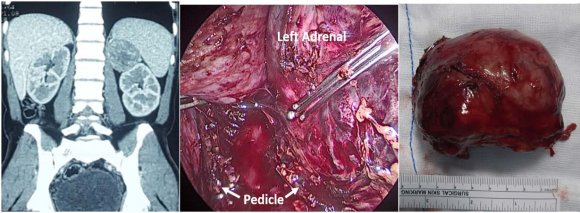
Our technique for radial forearm phalloplasty has previously been published in detail. 12,18,24 The radial forearm flap is our flap of choice due to the superior donor site and sensibility of the flap, in addition to its lower complication rate compared with other commonly used flaps such as the anterolateral thigh flap. 25 The procedure is completed in two stages to facilitate the creation of a neo-urethra. The first stage entails flap prelamination during which the radial forearm flap is designed and the neo-urethra is formed using autologous tissue, typically the vaginal mucosa at the time of vaginectomy and urethral lengthening (Figures 1a and b).
Flap prelamination occurs during the first stage of phalloplasty. The markings for the planned flap are determined pre-operatively after a normal Allen's test (Figure 2). Creating the urethra with mucosal tissue and not using forearm tissue allows for a smaller width in the flap skin paddle compared to the traditional tube within a tube urethra, and therefore if a patient places his upper extremity across his chest with the donor site toward his chest there is no visible skin graft. Also, the patient does not require the out-of-pocket expense of hair removal from the forearm since there will be no hair growth within the urethra. The boundaries for the flap are defined during this stage as the flap is elevated to allow placement of the neo-urethra. The tissue is raised in an ulnar to radial direction in the suprafascial plane. The neo-urethra is formed by circumferentially enveloping a 16 -24 French Foley catheter with mucosal tissue (Figure 3). The vaginal mucosa is harvested during the vaginectomy for the creation of the neo-urethra. When not previously performed, a hysterectomy may be performed during this stage providing additional mucosal tissue using buccal mucosa if needed (Figure 4). 26 Our technique for urethral lengthening has also been published in detail. 27
4. b) Free Tissue Transfer (Stage II)
The design of the radial forearm flap is defined during the first stage. Whereas the flap was elevated in a suprafascial plane for prelamination, the flap is now elevated in the subfascial plane to avoid injury to the neo-urethra (Figure 5). The medial and lateral antebrachial cutaneous nerves are preserved during dissection for coaptation to one dorsal nerve of the clitoris for erogenous sensation and the ilioinguinal and or genitofemoral nerves for tactile sensation. The radial artery and venae comitantes are ligated distally and proximally dissected for vascular anastomosis. The basilic and/or cephalic veins are preserved and dissected with the flap.
Using a modification of Monstrey's scrotoplasty technique the clitoris is dissected free from the lengthened urethra and subsequently denuded of skin. 28 The clitoral hood skin is removed and used for the coronaplasty using a technique described by Gottlieb (Figure 6). 29 The recipient arteries harvested for the vascular anastomoses are either the inferior epigastric artery or the descending branch of the lateral femoral circumflex artery. The thigh incision made for the lateral femoral circumflex is also used for the harvest of the saphenous vein.
Absorbable suturesare used for the urethral anastomosis in two layers, which is the first anastomosis performed (Figure 7). The vascular and neural anastomoses are performed next and are all hand sewn using 9-0 nylon suture with the aid of an operative microscope. In addition to a mucosa-only neourethra to decrease urinary complications that we have added to our surgical approach, which is beneficial in decreasing urinary complications, is the deployment of a gracilis flap urethroplasty at the time of flap transfer. 18 Upon closure of all incisions, a coronaplasty is performed with a skin graft obtained for the clitoral hood (Figure 8). The penile Foley catheter is removed once the patient has been discharged and 8-12 weeks after flap phalloplasty upon a normal pericatheter retrograde cystourethrogram revealing no extravasation of dye indicating there is no urinary fistula (Figure 9). Following successful bladder training and urination from the phallus, the suprapubic tube is subsequently removed.
5. III.
6. Results
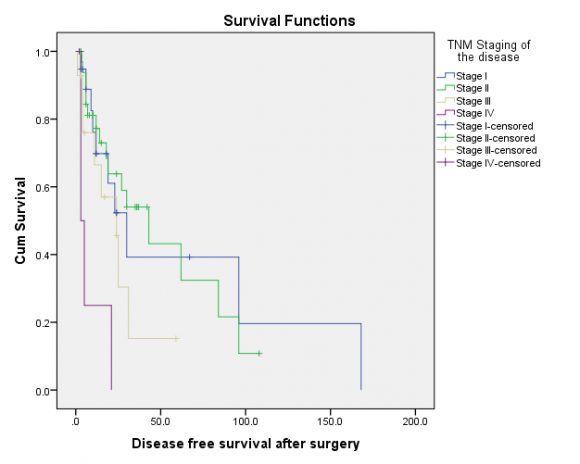
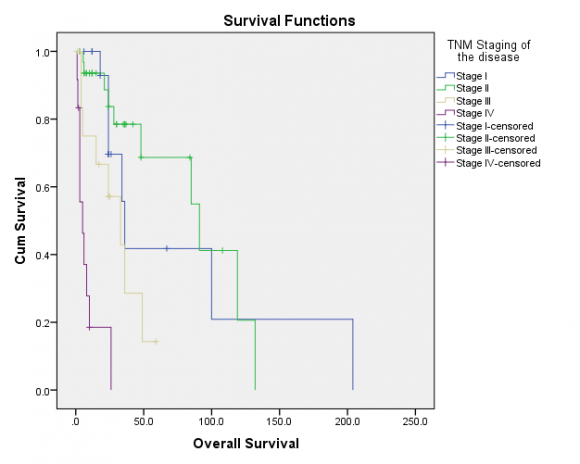
A total of 21 transgender male patients undergoing gender affirmation bottom surgery with a two-stage prelaminated radial forearm phalloplasty were identified and included in the study. The average age at the time of the first stage procedure was 35.7 ± 12.2 (range 21-54).The average BMI of included patients was 30.8 ± 7.2 (range 22.3 -48.5). Demographics and medical history are presented in Table 1. Neo-urethra prelamination was completed with either vaginal and/or buccal mucosa in all cases.
All of the 21 patients completed both the first and second stages of radial forearm phalloplasty. The second stage procedure was performed on average 60.3 ± 27.6 days (range 37 -126) after the first stage procedure. Donor and recipient vessels used for free tissue transfer are shown in Table 2. Final neophallus length averaged 13.7 ± 2.1cm (range 11 -17.8 cm).
Among the 21 patients completing second stage phalloplasty, ischemic complications occurred in 4 patients. With 4 of 21 patients developing vascular compromise postoperatively, our take-back rate for this series was 19%. Of note, once we switched to using the descending branch of the lateral femoral circumflex artery as our recipient artery we no longer had re-open procedures due to vascular compromise. In each case, the patients were taken back to the operating room and underwent successful revision of the vascular anastomoses. One patient with a BMI of 40, history of HIV, and diabetes was found to have a urinoma and bacterial infection resulting in thrombosis of both the artery and two outflow veins three weeks following flap transfer. Upon debridement of the flap, an anterolateral thigh flap was performed for his phalloplasty. Our flap loss in this series was 5%.This is a number we quote our patients when they are seen preoperatively.
Our urethral fistulas were commonly detected at the time of the first retrograde cystogram performed however following a subsequent negative study penile catheters were removed. Fistulas developed in 28% of patients however only 14% required operative intervention with a Johannsen urethroplasty. Urethral strictures occurred in 19% of patients and all required urologic cystoscopy and dilation which was readily done with balloon dilation due to the mucosa nature of the urethral conduit. One required a more invasive procedure for repair. Other complications noted in our series are presented in Table 3 however, most notable was our incidence of cellulitis of 33%, the majority of which occurred early in our series prompting our broadening of antimicrobial coverage of all aerobic and anaerobic species including fungus for an extended period of their hospitalization. Due to the proximity of this operative field to the colorectal system and its involvement in the urinary system the tissue is susceptible to a variety of microbes and traditional Surgical Care Improvement Protocols do not apply.
IV.
7. Conclusion
Our two-stage phalloplasty technique with prelamination of the neourethra with mucosa for transgender male gender affirmation bottom surgery was developed to decrease complications after using a one-stage tube within a tube radial forearm flap and a staged skin graft prelamination staged phalloplasty. Our goal was to decrease urinary fistulas and urethral strictures with our modification of technique. With urethral fistula rates ranging from 24% to 83% 11,19 and stricture rates ranging from 11 to 74% 11,20 we felt that the creation of a neourethra of mucosa would decrease these complications. Our operative fistula rate was 14% I and urethral stricture rate was 19%. The fistula rate is smaller than previously published. The gracilis flap which has been used to increase the vascularity of the urethral anastomosis has also been beneficial in the augmentation of the neoscrotum which has been able to obviate the need for testicular implants (Figure 10). Urethral strictures were not uncommon in this series with a rate of 19% of which three of four cases were managed conservatively with dilation only. One reason for stricture development may be the natal female detrusor muscle with aging and its subsequent limitations in channeling urine through a longer conduit, although further studies are warranted. 30 Although a two-stage technique may be more cumbersome we felt that in our hands we have been able to decrease urinary complications and minimize the commonly large donor site with this technique compared to the previously used skin within a tube radial forearm flap. Approximately 3-4 cm of forearm tissue is spared since this is not used for the urethra. This skin can be used for a phalloplasty of a greater circumference and a donor site that is not visible when patients place their forearm against their chest. Using a pre-laminated urethra our patients do not need to undergo electrolysis since the urethra is not created from forearm tissue, so we do not have the risk of hair growth in the urethra and its associated complications. An additional complication which is seen even with urethras pre-laminated with skin grafts. Although there have not been any blinded, randomized controlled trials comparing single-stage to two-stage phalloplasty, we believe that prelamination using vaginal mucosa for the construction of the transmale phallus urethra is a worthwhile technique that has demonstrated a reduction in the prevalence of complications with this already very challenging procedure.
8. Availability of data and materials
The data will not be shared, because they are in confidential patient files.
9. Financial support and sponsorship None
10. Conflicts of interest
"All authors declared that there are no conflicts of interest."
11. Ethical approval and consent to participate
Not applicable because this is a retrospective chart review.
12. Consent for publication
Informed consent was obtained for the publication of this article.