1. Introduction
entral venous catheterization is a frequent procedure in medical practice performed in image-guided interventionism services, emergency services, surgical, intensive care units, and hemodialysis units, among others. Venous catheterization is the technique whereby a catheter is inserted into the central vascular space for diagnostic or therapeutic purposes (1)(2)(3)(4). The international recommendation today is the insertion of central venous catheters (CVCs) using Doppler ultrasound to guide the procedure (5)(6)(7)(8)(9)(10)(11)(12). In addition to the advantages for elective procedures, the use of Doppler ultrasoundguided CVC implantation in cases of difficult venous access is widely known and recommended (13)(14)(15)(16)(17).
CVCs are placed in large venous vessels such as the internal jugular vein, subclavian vein, common femoral vein or superficial femoral vein, vena cava or suprahepatic veins, and for each of these structures the advantages of ultrasound guidance have been extensively studied (18,19). Likewise, peripherally inserted central catheters (PICCs) can be selected when there are no prothrombotic states present, since the latter increase thrombosis cases caused by the length and the vein-catheter relationship, increasing venous stasis (1,3).
2. II.
3. Indications
The most frequent indications include hemodynamic monitoring (measurement of central venous pressure or pulmonary artery wedge pressure), administration of medications or parenteral nutrition, impossibility of peripheral venous access, hemodialysis, plasmapheresis, potassium replacement at large doses and implantation of cardiac pacemakers (1,(20)(21)(22)(23).
4. Contraindications (absolute and relative).
Absolute: infection at the puncture site, venous thrombosis. Relative: Coagulopathy, poor patient cooperation (24,25).
5. III.
6. Types of Catheters
7. IV. Technical Considerations Prior to
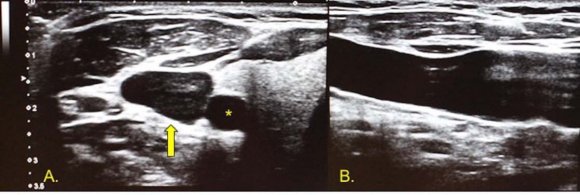
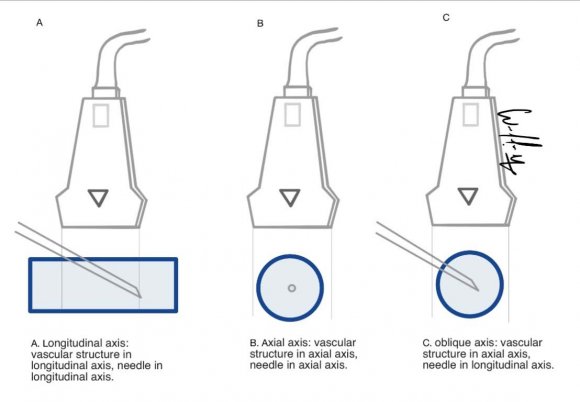
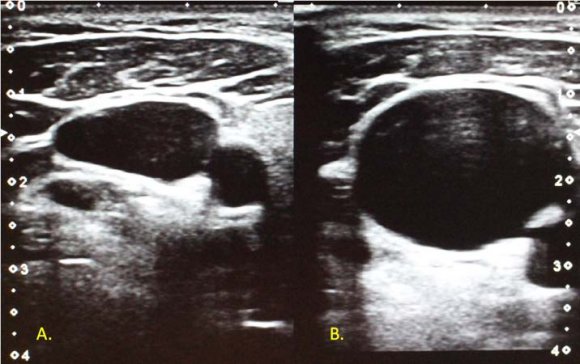
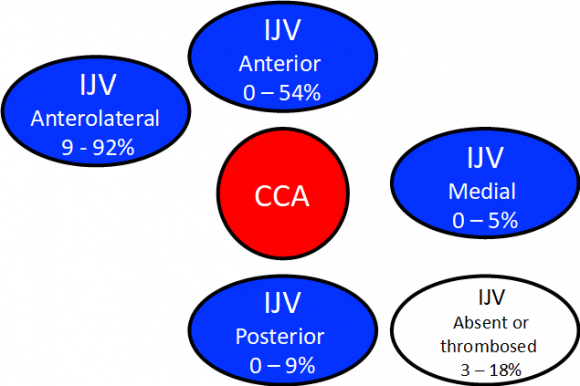
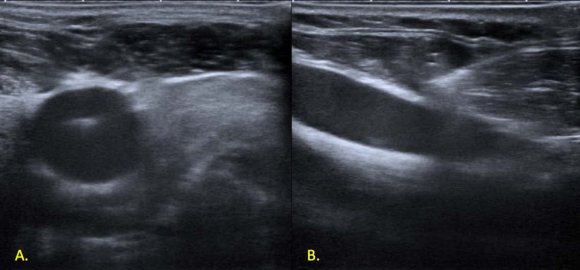
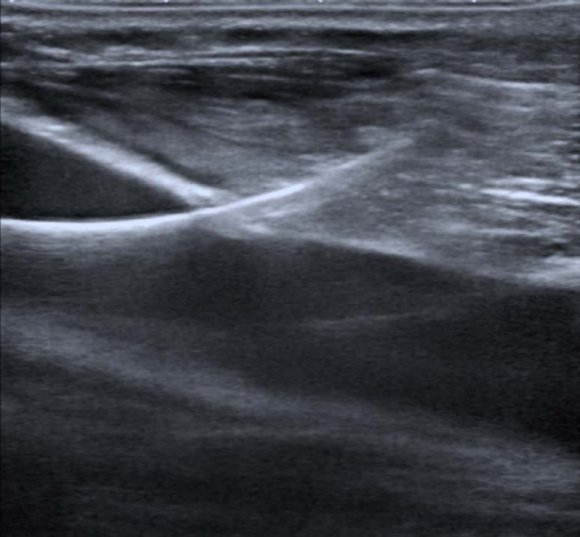
Conducting the Process Knowledge of the technical aspects of ultrasound and the characteristics of the equipment optimizes assessment prior to conducting the procedure as well as its correct display (26). High-frequency Bmode ultrasound serves to evaluate structures displayed on a gray-scale image, in real time and in different anatomical planes. Venous vessels are visualized as anechoic structures with echogenic thin and regular walls, most of the time exhibiting a greater diameter than their accompanying arteries. In some locations, with excellent image quality, it is possible to identify the venous valves which should be avoided when inserting catheters (27,28). Depending on transducer orientation, the venous vessels and the catheter are identified as tubular structures (in a longitudinal plane of the transducer with the vessel) or oval structures (if the transducer is placed transverse or axial to the axis of the vessel) (Image 1) (6). However, in some special cases, such as the catheterization of the internal jugular vein, it is possible to perform oblique orientations, where the vessel is projected in the axial plane and the needle in the longitudinal plane (scheme 1) (29). Under normal conditions the venous vessels collapse with gentle compression with the transducer and, increase their caliber with the Valsalva maneuvers (Image 2). Knowledge of normal vascular anatomy, anatomical variants and possible pathological conditions that may hinder the correct characterization of venous vessels is essential (30,31). In most cases, the internal jugular vein is located anterolateral to the common carotid artery (image 3) presenting a diameter that varies between 5 and 11.5 mm. The right vein diameter is relatively greater than the left, in up to 65% of cases (32), and the right is also generally preferred as the first option for catheter placement.
8. Scheme by William Prada.
Image 2: transverse image of the internal jugular vein at rest (A), during the Valsalva maneuver (B), there is an increase in caliber. The common femoral vein is made up of its tributaries: the deep femoral vein and the femoral vein (previously known as the superficial femoral vein), is located approximately 9 cm from the inguinal ligament and medial to the common femoral artery (Image 4). Proximally, the femoral vein runs medially to the artery, but, distally, it crosses over it and is located laterally (33). In some percentages and especially in the pediatric population, the femoral artery may adopt an anterior location to the vein (34).
The subclavian vein is the continuation of the axillary vein, delimited at the superior edge of the first rib (where the axillary vein receives its tributary, the cephalic vein) to the sternoclavicular joint at its junction with the internal jugular vein, forming the jugulo-subclavian confluent. It presents an arched path towards the cephalic region, its anterior wall is related to the posterior facet of the clavicle and its posterior wall is related to the subclavian artery, anterior scalene muscle, first rib and pleura (27).
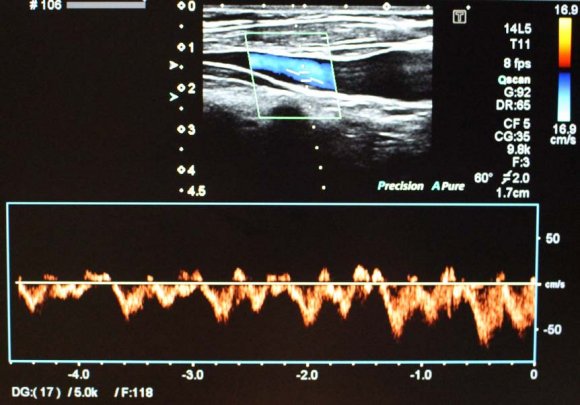
Examination with color Doppler and pulsedwave Doppler facilitates differentiation between arterial and venous structures, as well as the assessment of their patency. The veins have spontaneous and phasic flow (which vary with the respiratory and cardiac cycle) (27) (Image 4).
9. a) Seldinger Technique, Modified Seldinger and Process Description
The Seldinger technique, described by Radiologist Sven Ivar Seldinger in 1953, is used for percutaneous vascular catheterization with needle puncture and blood return (35)(36)(37). The advent of ultrasound and its use as a guide for procedures prompted a modification of the Seldinger technique, resulting its use in many interventional radiology procedures (biliary and urinary tract intervention, collection drainage, etc.).
Once the vessel has been channeled, a guide is inserted through the needle, the needle is withdrawn and a catheter is inserted through the guide, after path dilation. Central venous catheterization requires a linear transducer with a 10 MHz frequency or more, ideally narrow band for better maneuverability. Before starting the procedure, it is necessary to have all the requisite supplies, check the status of the catheter, permeabilize it with saline solution and keep in mind the length to be introduced for proper location of its distal end.
The skin must be prepared using an aseptic and antiseptic technique, setting up a sterile field, and the transducer must be covered with a sterile drape. Sterile gel should be used between the transducer cover and the patient's skin, and non-sterile gel between the cover and the transducer, facilitating the transmission of the ultrasound beam. The transducer shall be located according to the anatomical landmarks mentioned below and the vessel insonated in transverse and longitudinal planes. Local anesthetic is injected into soft tissues using ultrasound guidance with two objectives: to avoid intravascular injection and to verify the catheter's access route. Subsequently, the vessel is located in the center of the screen of the equipment obtaining a longitudinal axis, taking into account that catheterization in the longitudinal axis avoids accidental arterial puncture (7,38).
The puncture should be done with a Seldinger needle, with the bevel facing up and ideally at an angle of 45° to the skin. The needle is identified as a linear echogenic structure, which projects an acoustic shadow, and its movement ("ballotment" technique) displaces the adjacent tissues, enabling its location (6). The needle is visualized continuously, entering through the anterior wall of the vessel and aspiration is performed with a syringe attached to it. Obtaining blood confirms its correct location and patency. The insertion of the guide should be visualized in the longitudinal axis of the vessel, demonstrating correct direction (39-41) (Figure 5). The use of the vessel in the axial axis should be considered in cases where the longitudinal axis is not possible, such as in jugular access in patients with a short neck. Progression of the guide, the dilator or the catheter should not put up resistance; if so, the process should not continue, since it may cause vascular dissection. The performance of these steps should be observed under ultrasound guidance (Figure 6). The ultrasound can show the cause of resistance, such as vascular stenosis, vascular thrombosis or insertion towards the opposite wall of the vessel (6). In addition, the trajectory of the guidewire toward distal should be verified and it should not move cephalad.
10. VEIN ADVANTAGES DISADVANTAGES
11. Image 6:
The ultrasound allows to corroborate guide progress inside the vessel.
12. Ultrasound-Guided Central Venous Catheterization. Study Guide
Once the catheter has been inserted, ultrasound can be used to identify the mildly echogenic swirling with a rapid saline flush through the catheter ports. The use of pulmonary ultrasound can be recommended as well, to verify immediate complications such as pneumothorax and focused cardiac ultrasound to verify flushing of the solution and the distal location of the catheter.
13. b) Anatomical Repairs and Procedure Specifications for Central Venous Catheterization i. Internal Jugular Vein
The patient must be positioned supine, in the Trendelenburg position and with the head rotated to the contra lateral side by 45° (Image 7). The transducer must be placed parallel to the clavicle in the space formed between the sternal and clavicular heads of the sternocleidomastoid muscle (Sedillot's triangle) (3,6). This way, the internal jugular vein, carotid artery and sternocleidomastoid muscle are identified (scheme 2b). The patient should be positioned supine, in the Trendelenburg position with the head rotated to the contra lateral side. A supraclavicular or infraclavicular approach can be performed (42). In the supraclavicular approach, the transducer is positioned parallel (or slightly oblique) to the medial clavicle, above it, directing the transducer beam caudally, in order to identify the jugulo-subclavian confluent (6,27). In the infraclavicular approach, the transducer is positioned parallel to the clavicle, under it, at its junction of the external third and the middle third (scheme 2a). The puncture must be delivered by directing the needle towards the sternal notch and horizontally, with respect to the chest wall. (42.43). The subclavian artery and the lung are identified below the vein, thus avoiding accidental puncture.
Scheme by William Prada. iii
14. . Femoral Vein
The patient should be positioned supine, in reverse Trendelenburg position (semifowler), with the hip in external rotation. The transducer should be placed longitudinally, in the medial half of an imaginary line that joins the anterior superior iliac spine and the pubic symphysis (Inguinal ligament pathway), identifying the femoral vein medial to the artery (scheme 3). The puncture should be performed below the inguinal ligament, since it facilitates control of bleeding and avoids accidental puncture of intra-abdominal structures. However, the more distal, the greater the risk of arterial puncture (42). V.
15. Location of the Distal end of Catheter
With the exception of catheters for measurement of pulmonary artery pressure, it is recommended that the end of the catheter be located in the lower third of the superior vena cava (SVC) or the caval atrial junction and choosing a position parallel to the longitudinal axis of the vessel. The most widely used method to check the location of the end of the catheter is chest radiography, ensuring the location of the catheter in the extrapericardial SVC. For hemodialysis catheters, localization in the upper third of the right atrium is recommended, considering it offers specific advantages (better flow rates, reduced thrombus formation and stenosis venous) and minimal complications (44,45). The formulas established by Czepizak et al. in adult patients report an efficacy of 95% for the placement of the catheter in the superior vena cava for punctures in the internal jugular and subclavian veins (Table 2). The optimal positioning of the distal end of femoral central venous catheters has not been extensively studied. It is recommended in the inferior vena cava below the arrival of the renal veins for administration or extraction of fluids, but not for measurement of central venous pressure (35).
16. VI.
17. Complications
Up to 15% of CVCs present complications, which can be classified into mechanical, infectious and thrombotic, and in turn, into acute or chronic depending on the onset. The most frequent are those related to mechanical complications that occur between 5% and 19%, thrombotic complications between 2% and 26%, and infectious between 2% and 6% (5,42,46) (Table 3). Taken from (42,47,48).
( D D D D ) KPneumothorax is most often associated with catheterization of the subclavian vein, especially with the infraclavicular approach and less frequently with the catheterization of the internal jugular vein (49,50). Patients with pneumothorax who require pleural drainage present dyspnoea, tachypnea, coughing and/or desaturation. When this is suspected, radiographic and ultrasound monitoring should be performed (35). Hemothorax can be caused by arterial puncture or be one of the presentations of vascular perforation. It is one of the most feared complications, which occurs in 0.25% of cases and more frequently in left access, possibly due to the acute angle formed between the guide or the catheter and the wall of the SVC.
Due to the proximity of the internal jugular vein to the common carotid artery, arterial puncture is a frequent complication, which can be managed with extrinsic compression. Complications secondary to arterial puncture such as hematomas, pseudoaneurysms with or without neural compression, arterial thrombosis or dissection, cerebrovascular disease, arteriovenous fistulas, hemothorax or hemomediastinum have occurred.
Venous air embolism has an incidence of 0.8% and it can occur with the insertion, extraction or exchange of a CVC (44). It can be identified by direct observation of air bubbles in the catheter or sudden desaturation and may be reduced with the patient in Trendelenburg position (35). Benign and-to a lesser extent-malignant cardiac arrhythmias have been reported, caused by the guide or the catheter in the atrium or ventricle. If persistent, they require pharmacological or electrical intervention, and repositioning. Malposition or kinking of the device is associated with local vascular complications (phlebitis, perforation, thrombosis or occlusion), which can be suspected during catheterization with the absence of venous return and can be detected real time on fluoroscopy (50).
Puncture of the left subclavian vein is rarely associated with injury to the thoracic duct (50). Retroperitoneal hematoma is one of the most fatal complications in femoral vein catheterization, which occurs in 1.3% of patients without the use of ultrasound guidance (50).
Catheter-associated vascular infection has a significant effect on morbidity, mortality and health costs. Risk factors include poor insertion technique, emergency placement and long-term use of the catheter (49,50). Given its proximity to the perineal area, femoral vein catheterization is the one that is most associated with infectious complications, while subclavian catheterization is the least (8,49). Nevertheless, Timsit et al. published an analysis in 2013 of two clinical trials involving 2,128 patients, showing no differences in the rate of infection or colonization in the jugular and femoral catheters (P=0.34), presenting infection in 1 versus 1.1 per 1,000 catheters, respectively (50).
18. VII.
19. Conclusions
The use of Doppler ultrasound guidance for central venous catheterization is becoming increasingly popular in medical practice. The known advantages widely recommend its use to the point that, if not performed, it is considered bad clinical practice. Knowledge of venous anatomy and its features, the procedure technique and the physical properties of ultrasound are very useful to conduct a successful procedure. It is important to have experience in all the anatomical routes of ultrasound-guided venous catheterization and with the different techniques in order to deliver better results when facing vascular access.

| D D D D ) K |
| ( |
| Insertion Site | Formula |
| Right Subclavian Vein | (Height/10) -2 cm. |
| Left Subclavian Vein | (Height/10) + 2 cm. |
| Right Internal Jugular Vein | Height/10 |
| Left Internal Jugular Vein | (Height/10) + 4 cm. |
| FRECUENCY (%) |