1.
To Compare the Efficacy of Tap Block to Attenuate Pain in Laparoscopic Surgeries when Given in Pre-Incision to Post-Operative Period Arjun Joshi Abstract-The concept of Enhanced Recovery after Surgery not only saves the OT turn over time but has been shown to reduce the hospital stay and cost of treatment significantly. Various benefits of multi modal analgesia have already been proven in literature. Transversus abdominis plane (TAP) block has established itself a reliable tool for allaying pain particularly in laparoscopic surgeries. However, the timing for this block has not been specifically defined in literature. The primary aim of the present study is to compare the efficacy of preoperative vs. postoperative TAP block for allaying surgical pain while using 0.25 % plain bupivacaine via Visual Analogue Score. Secondary aim is to compare the consumption of opioids postoperatively after laparoscopic procedures when block is given pre-and post-incision period in Milligram Morphine Equivalent.
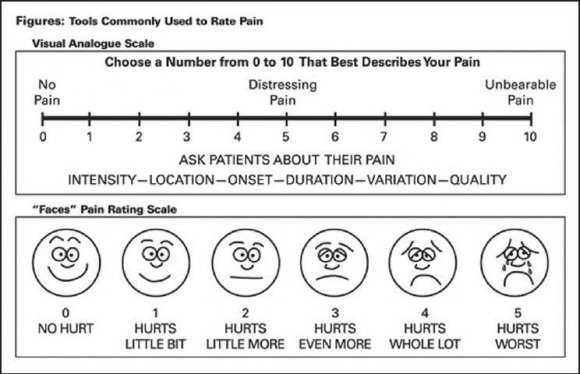
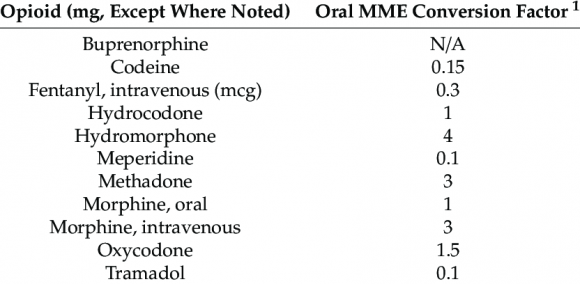
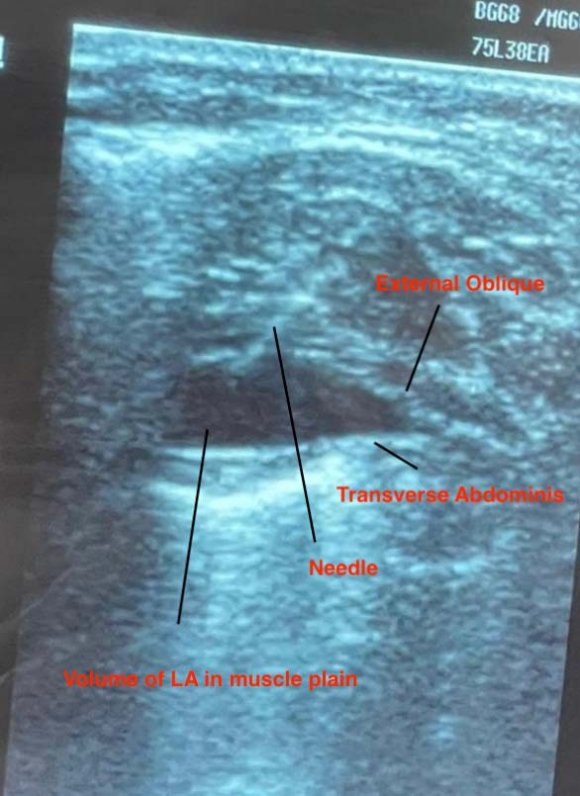
Methods: A retrospective cohort study was conducted in a service hospital of Armed forces located at an altitude of 12000 feet above mean sea level between September 2020 to September 2021 in patients who underwent elective laparoscopic appendectomy and cholecystectomy. The study was conducted to compare the efficacy of Trans Abdominal Plain block for allaying surgical pain when given pre-incision and when administered immediately after completion of surgery and before extubation using Visual Analogue Score (VAS) (Fig. 1) and postoperative opioid use in Milligrams Morphine Equivalent (Fig. 2). In the present study 40 patients were included in Group I who received TAP block 15 minutes before the incision and 40 patients were included in Group II who received block after completion of surgery and just before extubation. Standard anaesthesia technique was followed in both the groups and both the groups received the block while being under general anaesthesia under Ultra sonographic guidance by a trained Anaesthesiologist (Fig. 3). 10 ml of 0.25 % Bupivacaine was administered bilaterally in the muscular plain in both the study groups. Apart from the TAP block both the groups received 1 gram of intravenous Paracetamol prior to incision as a part of institutions multi-modal analgesia approach. The primary outcome of the study was assessment of post-operative pain by VAS at 30 minutes 3 hours and 6 hours. Secondary outcome was the comparison of opioid consumption in MME at similar time lines.
2. Fig. 2: [14]Morphine milligram Equivalent conversion factor
Result: Patients who received pre-incision plain 0.25 % Bupivacaine in TAP blocks had a better Visual Analogue Score and lesser opioid requirements at 30 minutes, 3 hrs and 6 hrs (1.03 vs 2.83, 0.98 vs 3.73 and 2.00 vs 5.35) and (0 vs 1.75, 0 vs 3.375, 0.875 vs 5.125 in MME) respectively. Conclusion: Administration of 0.25 % Plain Bupivacaine TAP block pre-incision was associated with significantly better control of pain and lesser consumption of opioid medications in post-operative period.
3. I.
Background n order to reduce the surgical stress response and to facilitate the early return of baseline function for patients undergoing surgery the concept of Enhanced Recovery After Surgery (ERAS) has been well established [1]. Reduction of surgical stress by methods including but not restricted to attenuation of pain by use of regional anaesthesia, early mobilization, and early enteral nutrition encompasses the components of ERAS [2,3]. Various clinical publications have supported that following ERAS protocol has shown a considerable reduction in duration of hospital stay, period of postoperative ileus, reduced morbidity, and an earlier return of baseline physiology [1,4,5,6] Attenuation of perioperative pain forms an integral part of ERAS, more so after abdominal surgeries. Sub-optimal pain control is proven to increase the in-patient department load, which itself has financial implications leading to patient dissatisfaction [6]. Use of multimodal anaesthesia techniques including but not restricted to neuraxial blockade in order to achieve an optimal pain control not only leads to a better patient experience in post op period but also reduces the demand of opioids. [7,8,9]. Transversus abdominis plane (TAP) block is an example of a regional anaesthetic technique that has been used extensively in abdominal surgery [10,11]. The block involves injecting local anaesthetic agent into the fascial planes between the internal oblique and transversus abdominis muscles. The duration of action for plain bupivacaine ranges from 2 to 10 hours with peak effect noted around 30 to 45 min [12]. Although the TAP block is used extensively for laparoscopic abdominal surgeries the time for administering the block for postoperative analgesia has not been clearly established in literature. In the present study, we assessed the effect of preoperative vs. postoperative administration of TAP block using plain 0.25 % bupivacaine on postoperative opioid use in patients undergoing elective laparoscopic appendectomy and cholecystectomy.
4. II.
5. Material and Methods
6. a) Patient selection
After taking ethical clearance from the institute and informed consent from participants we included ASA I, II patients undergoing elective laparoscopic appendectomy and cholecystectomy in a service hospital of Armed forces located at an altitude of 12000 feet above mean sea level between Sep 2020 to Sep 2021. Standard anaesthesia technique was followed in both the groups and participants in both groups were administered Intravenous paracetamol 1 gram prior to the surgical incision as a mart of multi-modal anaesthesia approach. Patients were divided in 2 groups based on timing of TAP block procedure. Group I included the patients who were administered block 15 minutes before the surgical incision and Group II included the patients who received the block after completion of surgery just before extubation.
7. b) TAP block technique
Both the groups in the present study were administered TAP block inside the operating room after induction with general anaesthesia following standard anaesthesia techniques and under Ultrasound guidance by a trained Anaesthesiologist. (Fig. 3) In group, I the block was administered 15 minutes prior to the surgical incision while in Group II the block was administered after the completion of the surgical procedure and before extubation. TAP block in both groups was administered bilaterally by injection total of 10 mL of 0.25 % plain bupivacaine each side in the fascial plane under ultra-sonographic guidance between the internal oblique and transversus abdominis muscles in the
8. Statistical Analysis
Statistical analyses were conducted to compare the baseline characteristics of the patients who received pre-incisional TAP blocks with those who received postoperative TAP blocks. Continuous variables were described using the mean and standard deviation (SD), Students t test was used and P < 0.0001 was considered statistically significant. All analyses were done in SAS 9.4 (SAS Institute, Cary, NC).
9. Result a) Descriptive analysis
A total of 80 patients were included in the present study. Group I included 40 patients who received TAP block 15 minutes prior to the surgical incision while Group II included 40 patients who received TAP block after the completion of surgery and before extubation. The mean (SD) patient age was 31.88 in Group I and 32.73 in Group II, the mean (SD) body mass index was 23.753 kg/m 2 in Group I and 23.663 kg/m 2 in Group II. There were no significant differences in the 2 groups with regard to age, sex, body mass index, American Society of Anaesthesiology classification, history of opioid use inflammatory pathology (Table 1.) The 2 groups were similar in terms of comorbidities, including history of hypertension, diabetes mellitus, hyperlipidaemia, smoking, and alcohol use. The surgical indications and surgical approaches were similar between the 2 groups. Group I had however comparatively lower Visual Analogue Scores noted at 30 minutes, 3 hours and 6 hours postoperatively as compared to group II noted as 1.07 vs 2.82, 0.97 vs 3.85 and 2.00 vs 5.357 respectively Graph 2. Moreover, the consumption of opioids as noted by Morphine milligram equivalents in similar time lines was significantly lesser than in group I when compared to group II noted as 0 vs 1.75, 0 vs3.375 and 0.875 vs 5.125 respectively Graph 1in with a p value of <0.0001. .
10. Graph II
V.
11. Discussion
Pain management forms an integral part of the post-operative care. With the evolution of minimally invasive surgical procedures, the modern surgical management is moving towards fast turnover of patients and decreasing over all hospital stay. The ERAS protocol in surgery has not only facilitated in the early return of baseline physiological parameters but has also been pivotal in reducing the financial implications on the patients, needless to mention the additional burden on the health care services. In the recent times of pandemic like Covid 19 pneumonia it is always prudent to decrease the in hospital stay of the patients as much as possible while not refuting them the benefit of surgery. Since the postoperative pain management is a fundamental part in achieving the goals of ERAS; usage of multi-modal anaesthesia but not restricted to neuraxial blocks have been an attractive modality for attenuating post-operative discomfort. Regional anaesthesia techniques viz. TAP blocks have established themselves as an appealing methodology for diminishing post-operative opioids use especially given their low risk of adverse effects. More so in high altitude areas where conservation of minute ventilation is of paramount importance due to existing hypoxic conditions it is essential to avoid drugs which cause depression of central respiratory centres. In the present study, better VAS scores were seen in post-operative periods at 1hour, 3 hours, 6 hours in patients who received pre-operative TAP blocks when compared to those who received TAP block after the completion of surgery. Furthermore, the requirement of opioids as well as non-opioid analgesics in the post-operative period was significantly reduced in the patients who received the block pre-incision Graph 1. There was no significant difference in the average length of stay, surgery time or re-surgeries in both the groups.
Various clinical publications have already established the benefit of TAP block in laparoscopic procedures for abdominal surgeries. Tikuisis et al. in his study demonstrated that patients who were administered TAP blocks pre-incision had significantly lower pain scores at 1, 3, and 6 h [15].
Pirrera et al. compared the use of preoperative Ropivacaine TAP block vs. thoracic epidural analgesia in patients before elective laparoscopic colon resection. Both patient groups were a part of a standard enhanced recovery after surgery pathway. Additionally, the TAP group had significantly lower rates of postoperative nausea, vomiting, ileus, and paraesthesia. There was no significant difference in hospital length of stay or 30-day readmission rate [16].
In a prospective, randomized, double-blind study, Keller et al. assessed the effect of TAP blocks on postoperative pain in patients following laparoscopic colorectal resections. Compared to their counterparts, the TAP group had significantly lower pain scores and used fewer opioids. However, there was no difference in hospital length of stay and readmission rate between the groups [17]. These research study findings are consistent with our current results. The administration of TAP block before the surgical incision is in line with preemptive analgesia in the present study we found that the administration of TAP block using Bupivacaine postsurgery and before surgical incision is an optimal time. The first study on pre-emptive analgesia was published by Woolf and Wallin 1986. In a model of central hyper excitability produced by electrical stimulation of C-fibres and recorded in rat dorsal horn neurons, they showed that the amount of systemically administered morphine needed to prevent the development of hyper excitability was much less than the amount needed to reverse it after the establishment of hyper excitability [18] Surgeryinduced central sensitization has two phases: incisional and inflammatory (reaction to the damaged tissue). It is possible to suggest that with inflammatory injury playing the dominant role, anti-nociceptive protection provided by pre-emptive treatment extends well into the postoperative period to cover the inflammatory phase.
VI.
12. Conclusion
The modern medicine aims at minimally invasive procedures and enhanced recovery after surgery to decrease the hospital stay. More so in the present era of Covid-19 pandemic it may be only prudent to keep the in-hospital exposure of the patients minimal while not denying them the benefits of surgery. A reduced hospital stay would not only decrease the financial implications on patients but would also decrease additional burden on health care services. Since allaying the post-operative pain is pivotal in early recovery of patient's usage of neuraxial blockade has become a vital modality. We advocate the usage of TAP block for Laparoscopic abdominal surgeries and strongly recommend that TAP block be administered after the completion of surgical procedure and before extubation for better post op analgesia.
| Year 2022 | |||||
| 29 | |||||
| Volume XXII Issue I Version I | |||||
| D D D D ) | |||||
| ( | |||||
| Group I Group II | Mean of age 31.88 32.73 | SD 9.63 8.85 | SEM 1.52 1.40 | P value 0.6822 | Medical Research |
| Group I Group II | Mean of BMI 23.753 23.663 Mean of VAS 30 minutes post | SD 2.067 1.925 SD | SEM 0.327 0.304 SEM | P value 0.8408 P value | Global Journal of |
| extubation | |||||
| Group I | 1.075 | 0.62 | 0.10 | 0.0001 | |
| Group II | 2.825 | 8.87 | 0.14 | ||
| Mean of VAS 3 hours post extubation | SD | SEM | P value | ||
| Group I | 0.975 | 0.62 | 0.10 | ||
| Group II | 3.85 | 0.78 | 0.12 | 0.0001 |