1.
Introduction n 11th March 2020 the World Health Organization declared the COVID-19 outbreak a public health emergency of international concern 1 , 2 . The outbreak started in mainland China in the 2003 extreme acute respiratory syndrome (SARS) and 2012 Middle East respiratory syndrome (MERS), which strongly suggests the virus' droplet transmission and contact transmission 7 , 8 . In addition to the standard respiratory disorder, less common features such as diarrhea, nausea, vomiting, and abdominal pain have been reported in different degrees and different sample populations. 9 Transmission by droplets occurs when a person is in close contact (within 1 meter) with another person who has developed respiratory symptoms (coughing or sneezing) due to infection with COVID-19 and is thus at risk of exposure of his/her mucosa (mouth and nose) or conjunctiva(eyes) to potentially infectious respiratory droplets (generally known to be greater than 5-10 ?m). Droplet transmission can also occur near the infected individual, via fomites (clothes, utensils, furniture, stethoscope, thermometer, etc. 10 , 11 India registered the first COVID-19 case in Kerala on 30 January, which grew to three cases by 3 February; all were students who had returned from Wuhan. Apart from these, there was no noticeable change in transmissions in February. On 4 March 22 new cases, including 14 infected members of an Italian tourist party were reported . 12 In March, after many people with travel experience to affected countries, the transmissions increased, and their contacts tested positive. A 76-yearold man with a travel background to Saudi Arabia on 12 March became India's first COVID-19 fatality. A Sikh preacher, who had a travelling history to Italy and Germany, turned into a "mega spreader" by attending a Sikh festival in Anandpur Sahib on 10-12 March. Twenty-seven COVID-19 cases were traced back to him. More than 40,000 people were quarantined on Around 4,000 stranded pilgrims returned from Hazur Sahib in Nanded, Maharashtra. on 2 May in Punjab, many of them tested positive, including 27 bus drivers and drivers who had been part of the scheme for transport. On 13 May 1,225 pilgrims had been tested positive . 17 A popular subject -perhaps the most thought about, and emotive issue for front-line treatment professionals dealing with Coronavirus Disease Patients (COVID-19) -is a personal protective system (PPE). During the 2019 Corona Virus Pandemic (COVID-19), a lengthy and rising list of health care workers has lost their lives . 18 . At the beginning of the outbreak, a significant proportion of health care staff became infected, probably secondary to a lack of awareness and inadequacy of personal protective equipment (PPE). For several nations throughout Europe, debates have started about how to optimally secure health care personnel. Coronavirus COVID-19 has travelled across the globe impacting public care services 19 . There are various recommendations for the protection of health care workers in each country or hospital. Nevertheless, no concrete standards for personal protective equipment (PPEs) and health protocols in the area of medicine have yet been created 20 15 Arora P, Kumar H, Panigrahi BK. Prediction and analysis of COVID-19 positive cases using deep learning models: A descriptive case study of India. Chaos, Solitons & Fractals 2020:110017. 16 Zaenuri A. KONSEPSI FIKIH DAKWAH JAM?'AH TABL?GH PADA MASA PANDEMI COVID-19: Telaah Gerakan Dakwah Jam?'ah Tabl?gh Gorontalo. JIL J Islam Law 2020; 1:1-23. 17 Sidor A, Rzymski P. Dietary Choices and Habits during COVID-19 Lockdown: Experience from Poland. Nutrients 2020; 12:1657. 18 . Health care practitioners should be trained and supported optimally from the guidelines. The average person with COVID-19 infection is known to infect 1, 5 to 3, 5 people. The capacity of an entire hospital to be significantly diminished by a single COVID-19 infection of healthcare staff. About 1300 health workers were contaminated in Wuhan, the outbreak area. More than 200 doctors have died of the illness in Italy to this day 21 . The likelihood of infection is more than three times the general population for health workers. Both healthcare staff is commonly known to wear standard surgical masks during any patient encounters. Also, the correct hand hygiene and disinfection are suggested to avoid excessive touch, preserve adequate space. Positive or suspicious patients with COVID-19 are isolated from non-infected patients in most hospitals 1, 2 , 22 There are a wide range of personal protective equipment (PPEs) globally varying from strong respiratory purifiers (PAPRs) to different facemasks, helmets, gowns, and gloves 20, . 23 . Epidemics of severe acute respiratory syndrome coronavirus 2003 (SARS-CoV-1) or Middle East Respiratory Syndrome Corona Virus (MERS) have historically occurred in countries (e.g., China, Taiwan, and South Korea), where suits for PAPR and Hazmat are available. Some of the most impressive value of PAPR is the re-usability of aerosol producing medical procedures (AGMPs), thus giving them safety . 18,22,24 Covering more of the body leads to better protection. Though, this may contribute to additional exposure as it is generally correlated with greater difficulties in placing and extracting the personal protective equipment (PPEs) because the PPE becomes less easy .Covers are the worst to remove which provide the greatest security, accompanied by long skirts, skirts, and aprons. Respirators use with coverings can have more security than a cloth-covered mask, but are easier to use. Airier personal protective equipment (PPE) forms can contribute to identical pollution rates but can be rendered more comfortable. Coronavirus disease is predominantly transmitted by contact or droplet transmission. Coronavirus disease can become aerosolized by 'aerosol-generating procedures' and then the airborne transmission is possible 1,2,20 25 For certain countries, the lack of personal protective equipment (PPE) has contributed to healthcare workers being vulnerable to probable . 21 Meier K, Glatz T, Guijt MC, Piccininni M, van der Meulen M, Atmar K, et al. Public perspectives on protective measures during the COVID-19 pandemic in the Netherlands, Germany and Italy: A survey study. PLoS One 2020;15: e0236917 22 Wang J, Zhou M, Liu F. Reasons for healthcare workers becoming infected with novel coronavirus disease 2019 (COVID-19) in China. J Hosp Infect 2020; 105:100-1. https://doi.org/10.1016/j.jhin.2020. 03.002. 23 Jh V, Jh R, Fs KB. Verbeek JH, Rajamaki B, Ijaz S, Sauni R, Toomey E, Blackwood B, et al. Personal protective equipment for preventing highly infectious diseases due to exposure to contaminated body fluids in healthcare sta (Review). 2020; 4:1-147. https://doi.org/ 10.1002/14651858.CD011621.pub4.www.cochranelibrary.com. 24 Jain VK, Iyengar K, Vaish A, Vaishya R. Differential mortality in COVID-19 patients from India and western countries. Diabetes Metab Syndr Clin Res Rev 2020 25
2. Need for Study
. The usage of personal protective equipment (PPE) in emergency operations created questions regarding its impact on surgical performance, sense of safety, non-technical efficiency, general comfort, and surgical exhaustion 1 .
Personal protective equipment (PPE) is only one part of a system to protect staff and other patients from COVID-19 transmission. Personal protective equipment (PPE) recommendations from international organizations are broadly consistent; personal protective equipment (PPE) use is not. Appropriate use of Personal protective equipment (PPE) significantly reduces the risk of viral transmission and infection. Personal protective equipment (PPE) should be matched to the potential mode of viral transmission -contact, droplet, or airborne. Many health care personnel do not know what is safe to wear 21 With a growing number of doctor's fatalities, we aimed at increasing awareness and practice of health care personnel on the issues across the use of PPE by evaluating their awareness and practice using a validated questionnaire.
? In epidemics of highly infectious diseases, such as Ebola Virus Disease (EVD) or Severe Acute Respiratory Syndrome (SARS), healthcare workers (HCW) are at much greater risk of infection than the general population, due to their contact with patients' contaminated body fluids. Verbeek et el 2019 ? Lack of awareness and proper practice regarding the use of PPE can lead to hazard known as occupational hazard caused by improper negligence
The need for the use of these PPEs has increased over the years with increasing awareness of workplace hazards, and the difficulties associated with overdependence on other control measures which for some agents cannot be eliminated or even monitored. This is especially important in hospital settings where workers are often exposed to biohazards and other infectious agents like hepatitis B, hepatitis C, and HIV. Indeed, health facilities are rife with very hazardous agents: just recently COVID-19 disease, Lassa fever, and other infections caused high mortality among health workers in the affected countries in India and subregion. Control of Coronavirus has become particularly difficult and several measures including the use of appropriate PPEs were used to contain it. Apart from biohazards, in hospitals, some departments work on radioactive materials (radiology department) and others that work on both biohazards and chemicals (laboratory department). Some hospitals have therefore established policies on PPE. 4 Nosocomial infections transmitted by direct contact can be prevented by adapting standard precaution guidelines. Appropriate use of PPE is the easiest way to prevent contact from secretions and transfer of pathogens which is mainly the mode of transmission of COVID-19. It's important to assess the level of compliance with the use of PPE by various HCWs who make direct contact with COVID-19 patients. Based on the available evidence, the COVID-19 virus is transmitted between people through close contact and droplets, though further studies are being carried out to know whether it is airborne. The people most at risk of infection are those who are in close contact with a COVID-19 patient or who care for COVID-19 patients, hence this study attempted 7 .
IV.
3. Aim
This study aims to evaluate the awareness and the practice of personal protective equipment use during COVID-19 among health care personnel.
V.
4. Objectives
To determine the level of awareness among health care personnel on the use of PPE To evaluate the practice in the use of PPE among health care workers Hypothesis H1=There will be a significant correlation between awareness and practice of use of PPE among health care workers.
H0=There will be no significant correlation between awareness and practice of use of PPE among health care workers in the treatment of COVID-19.
5. VI.
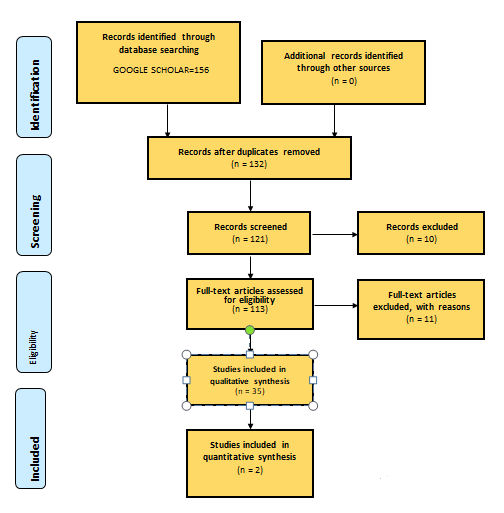
6. Methodology a) Search Strategy
The method of review is based on the PRISMA 27 27 Kublashvili K, Tsikarishvili K, Uriadmkopeli K, Kobalia S. EDITORIAL format (preferred reporting item for systematic reviews and meta-analysis). In the search for the topic, using google scholar search engine, from the identified keywords. Such as awareness, the practice of PPE, COVID-19, and health care personnel. It was decided that all and at most three out of five keywords to be used in the search for the articles related. As two researchers were consulted for the review, the first researcher worked on the literature search and the second on the technical aspect which was the extraction of articles. The initial search after entering of the title (Awareness and practice of PPE use during among health care personnel "Personal Protective Equipment COVID 19") produced 16,900 results of which custom range was applied to capture current data with 5 years, from 2016 to August 2020 and this yielded 8, 070 results. On observation of the articles, several of them did not match the search criteria. Therefore, an advanced search was applied to narrow down the subject and be more specific. The advanced search was applied "with all the words", "Personal Protective Equipment COVID 19", with words occurring anywhere in the article and dated between 2016 till 2020 were reviewed and it resulted in twenty-five articles, sorted by relevance.
7. b) Research Approach
The research approach used is quantitative; this is because the data obtained is a quantifiable data. The information collected is from sampling methods from an online validated questionnaire.
8. c) Research Design
A longitudinal cohort study in a form a prospective study was designed and used as data collection was obtained throughout specific time across the same category of individuals.
9. d) Variables
The variables are independent. This is because the variable obtained are stable and unaffected by the other variables that were measured. It refers to the condition that the experiment is systematically manipulated. It is a presumed cause.
10. Schematic representation of the study
11. e) The Setting of the Study
The study was carried out among health care workers that work in a hospital setting as they are the first in line in the battle against COVID-19. These HCWs include Physicians, hospital pharmacist, radiologist, physiotherapist, lab technicians among others
12. f) Sample and Sampling Technique
The sample was calculated using a Cochran formula.
13. i) Tool/Instruments
A self-designed questionnaire was used which is validated by medical experts. The questionnaire was designed in such a way that it provides information related to socio-demographic data, attitude, and practice of HCWs concerning personnel protective equipment used in taking care of patients with COVID-19. The questionnaire consists of a three-part, the first part being the sociodemographic data, then awareness, followed by practice. The results are presented in a tabular form
14. k) Pilot Study
A result of 20 respondents as specified in the outline provided by the school and guide was used as a pilot study. Necessary corrections made during the presentation were implemented and as such the current result provided updated information.
15. l) Data Collection Process
An online validated questionnaire was used which as stated was validated by medical experts. A google doc form was constructed shared among the targeted respondents listed above, who fulfil the inclusion criteria.
16. m) Plan for Data Analysis
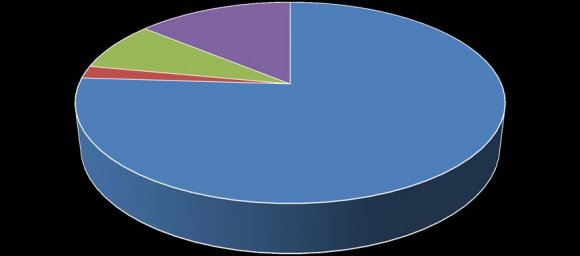
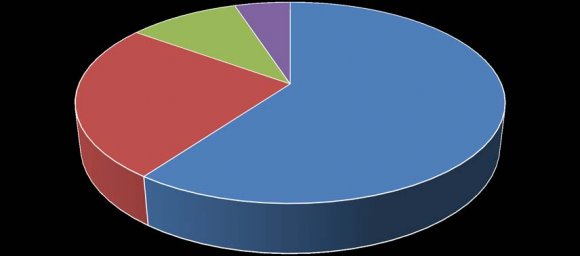
Data analysis was done using descriptive and inferential statistical methods to meet the objectives of the study. Findings were presented in the form of Tables and figures. Using SPSS and EXCEL. In terms of practice, 60% of our correspondents are practicing while 25% are not. Table 4 shows the demographic and professional characteristics data of the health care workers. The study analyzed 132 health care workers(HCW), of which 76.5% (105) were found to be male and 23.5% (27) female, this is due to the data obtained from random sampling among the HCW. 52.3% (69) of the HCWs are from the age limit of 26-30 which has the highest percentage and 3.8% (5) age limit 36-40 is the lowest. This is by a study on Personal protective equipment for preventing highly infectious diseases due to exposure to contaminated body fluids in healthcare workers, which also shows a higher percentage of men as compared to women at the age group of 26-30 years [23] . The experience of the HCWs was analyzed, 1-5 years being the highest with 64.39 %(85) followed by those with < 1year having 30(22.72%). Those with high school education represent 5.31 %(7) and 94.69%(125) have at least a degree. This is also following a study on the use of personal protective equipment by health care workers in a There is a high level of awareness among the HCW recorded as seen from Table No.2, this can be attributed to the fact that COVID-19 is a pandemic disease and the method of which it can be transmitted as defined by the World Health Organization (WHO) is through physical contact with the infected patient 1 Though PPE prevents the risk of exposure as health workers are more at risk to be infected. The media also plays a vital role in increasing the level of awareness regarding the importance of PPE in the fight against COVID-19, as various outlets provide knowledge to the society, health workers inclusive on the preventive measures required to protect oneself against the pandemic.
On the questionnaire, the level of awareness of the respondents was analyzed. 75.72 % of health care workers are aware of personal protective equipment, 77% are aware of the role personal protective equipment play in the prevention of the spread of COVID-19, 5% are not aware, which shows that more education and awareness is needed, this is in conjunction to the fact that an average person with COVID-19 infection is known to infect 1-5 to 3-5 people. The capacity of an entire hospital to be significantly diminished by a single COVID-19 infection of healthcare staff 2 90% of health care workers are mindful of the added precaution health workers need to protect themselves from COVID-19. The cause of occupational hazards due to the lack of personal protective equipment is a known fact for 80% of the population, though 5% still shows no knowledge on that aspect (reason), some studies show that covering more of the body leads to better protection. Though this may contribute to additional exposure as it is generally correlated with greater difficulties in placing and extracting the personal protective equipment (PPEs) because the PPE becomes less easy 20 . The availability of personal protective equipment amongst health care workers is very low according to our study, this is very alarming due to how fast the disease is spreading and how highly expose health workers are. According to a report by WHO, there is a quite shortage of overall availability of PPE during the outbreak of COVID-19 and a recommendation of management of PPE should be coordinated through essential national and international supply chain management mechanisms, this explains the 68% of the respondents regarding the unavailability of the PPE 1 Another thing we discussed is the ability of the personal protective equipment to interfere with your work. 92.5% of the respondent shows how it affects their ability to do work, studies show how covers are the worst to remove which provide the greatest security, accompanied by long skirts, skirts, and aprons, Though, this may contribute to additional exposure as it is generally correlated with greater difficulties in placing and extracting the personal protective equipment (PPEs) because the PPE becomes less easy 1,2,20 .
PPE used by HCWs includes gloves, medical masks, goggles or a face shield, and gowns, as well as for specific procedures, respirators (i.e. N95 or FFP2 standard or equivalent), and aprons (WHO,2020). In this study, 100% practice the use of at least one type of PPE. Regarding the comfortability experienced by HCWs when using PPE, 40% complained about breathing problems and prefer the N95 respirator over the regular surgical masks. The use of overall disposable gown to provide a physical barrier to microbes as well as COVID-19 was a common practice by 85% of the respondents. There is a wide range of personal protective equipment (PPEs) globally varying from strong respiratory purifiers (PAPRs) to different facemasks, helmets, gowns, and gloves. Epidemics of severe acute respiratory syndrome coronavirus 2003 (SARS-CoV-1) or Middle East Respiratory Syndrome Corona Virus (MERS) have historically occurred in countries (eg, China, Taiwan, and South Korea), where suits for PAPR and Hazmat are available. Some of the most impressive value of PAPR is the re-usability of aerosol producing medical procedures (AGMPs), thus giving them safety [53] . Job performance is affected by at least 41% of the respondents while 43.6 % experienced no such issues. To improve the practice, 87.2% stated that, the presence of reminder posters at their places of work significantly increases their ability to wear a PPE. Hence, 85% regularly wear their PPE.
17. VIII.
18. Conclusion
In conclusion, the level of awareness is quite high as seen from the results, and also there is a need to educate more regarding the use of PPE despite their uncomfortably stated by few HCWs. The practical use of PPE during this pandemic is also much as the result shown. Their availability is a matter of great importance F disease outbreak, showing that the majority of health workers associated with disease outbreak are degree holders, this shows that people are educated, and shows that at the beginning of the outbreak, a significant proportion of health care staff became infected, probably secondary to a lack of awareness and inadequacy of personal protective equipment (PPE) [1] . as there is a shortage of overall equipment due to high demand.
IX.
19. Recommendation
? Recommendation to the next researcher 1. A similar study can be conducted to access the awareness and practice of personal protective equipment use during COVID-19 among health care personnel and to find the actual impact of the transmission of the disease. 2. Along with an individual approach, all the health care personnel should be encouraged to participate in international and national awareness of personal protective equipment use during COVID-19
? Recommendation to the policymakers and health sector: 1. A public health approach that seeks to change the status and promote supportive strategies for better health and protection against diseases like COVID-19 which are easily transmitted. 2. Government legislation should increase awareness of personal protective equipment use during COVID-19, along with some guidelines in public places and advertisement of encouraging the use by both patients and healthcare workers.
20. Public Health Implication
? Public health is the science and art of preventing diseases, prolonging life, and improving human health through better education and awareness, policymaking, promoting a standard lifestyle, research, and prevention. ? The issue of personnel protective equipment and health care workers is an important integral part of public health care as a whole. Since the outbreak of COVID-19, health care workers have been the face in the fight and prevent the spreading of this disease. ? The finding of this study can help in planning an education program to raise awareness in the public regarding the safe use of personnel protective equipment, COVID-19, and its ill effect on health. ? The findings brought to light that if awareness and health education programs are implemented, it will help to change the negative behavior to positive and health situations. And still, the education of the youths remains the most effective policy and strategy on hygiene misconception.
21. Limitation of the Study
This study is only limited to those health workers that are only based in the hospital, which are the for the front in the fight against.
Funding: This research received no external funding.
22. Conflicts of Interest:
The authors declare no conflict of interest.
23. Ethics approval and consent to participate
There's no need for ethical approval for this review since no patient data will be collected. In this study author has thoroughly analyzed ethical issues including the plagiarism, confidentiality, malfeasance, data falsification and/or falsification, double publishing and/or submission, and duplication.

| S/N | Activity | Aug | Sept | Time Frame Oct Nov Dec Jan Feb Mar Apr May | Jun | Responsible person | |
| Research topic development | Health worker | care | |||||
| Concept | Health care | ||||||
| development | worker | and | |||||
| and approval | supervisor | ||||||
| Research proposal writing | Fin al exa m | Health worker supervisor care and | |||||
| Submission of | Health | care | |||||
| research | worker | ||||||
| proposal | |||||||
| Health | care | ||||||
| Data collection | worker | and | |||||
| supervisor | |||||||
| Health | care | ||||||
| Data analysis | worker | and | |||||
| supervisor | |||||||
| Dissertation writing | Health worker supervisor care and | ||||||
| Submission of | |||||||
| dissertation | |||||||
| and | Hospital | ||||||
| dissemination | health | care | |||||
| of results | worker | ||||||
| S/n | AWARENESS | YES(%) | NO(%) | NOT SURE(%) | VERY MUCH (%) | LITTLE BIT (%) |
| 1 | Do you know what personal protective equipment is | 75.72 | 2.50 | 0 | 18.94 | 3.20 |
| 2 | Do you know the role of personal protective equipment in the prevention of Covid-19? | 77.00 | 17.50 | 2.5 | 0 | 2.5 |
| Do you know that additional precautions are | ||||||
| 3 | required by health care workers to protect | 90 | 5 | 2.5 | 2.5 | 0 |
| themselves from Covid-19? | ||||||
| Do you know that the type of personal | ||||||
| 4 | protective equipment used for COVID-19 | 84.6 | 10.3 | 0 | 5.1 | 0 |
| patients varies among personnel? | ||||||
| Do you know that the lack of use of | ||||||
| 5 | Personal protective equipment can lead to an occupational hazard related to COVID- | 80 | 5 | 2.5 | 7.5 | 5 |
| 19? | ||||||
| 6 | Does Personal protective equipment always available to you? | 27 | 62.2 | 2.7 | 2.7 | 5.4 |
| Do you know that personal protective | ||||||
| 7 | equipment interferes with the ability to do a | |||||
| job? |
| AWARENESS | |||||||
| 14, 14% | |||||||
| 8, 8% | |||||||
| 2, 2% | |||||||
| 76, 76% | |||||||
| YES | NO | NOT SURE | DON'T KNOW | ||||
| S/N | PRACTICE | YES (%) | NO (%) | NOT SURE (%) | MAYBE (%) | I DON'T KNOW (%) | |
| 1 | Do you think wearing personal protective equipment is uncomfortable for you? | 37.88 | 49.24 | 20.45 | 0 | 0 | |
| 2 | Do you think personal protective equipment provides a physical barrier to COVID-19? | 84.85 | 7.56 | 3.79 | 3.79 | 0 | |
| 3 | Do you believe your job performance is affected by wearing personal protective equipment? | 41 | 43.6 | 12.6 | 2.6 | 0 | |
| Did you experience any difficulties, incidents, or | |||||||
| 4 | accidents while using personal protective | 23.1 | 59 | 5.1 | 12.8 | ||
| equipment? | |||||||
| Do you think that posters in the working area | |||||||
| 5 | are important in reminding you to wear personal | 87.2 | 0 | 5.1 | 5.1 | 2.6 | |
| protective equipment? | |||||||
| 6 | Do you regularly wear personal protective equipment? | 85 | 15 | 0 | 0 | 0 | |
| 7 | Do you share your protective equipment? | 5 | 85 | 2.5 | 5 | 2.5 | |
| Crosstab | ||||||
| Practice-based on literacy and education | ||||||
| yes | no | Not sure | maybe | I don't know | ||
| Years | <1 | 36 | 9 | 4 | 5 | 74 |
| of | 1-5 | 26 | 8 | 3 | 0 | 57 |
| practic | 6-10 | 27 | 5 | 1 | 3 | 36 |
| e | 11> | 10 | 3 | 0 | 0 | 13 |
| Total | 89 | 25 | 8 | 8 | 132 | |
| Chi-Square Tests | ||||||
| Value | Degree of freedom | Asymptotic Significance (2-sided) | ||||
| Pearson Chi-Square | 7.354 a | 9 | .600 | |||
| Likelihood Ratio | 10.560 | 9 | .307 | |||
| Linear-by-Linear | .338 | 1 | .561 | |||
| Association | ||||||
| N of Valid Cases | 180 | |||||
| Crosstab | ||||||
| Year 2022 |
| 15 |
| Volume XXII Issue III Version I |
| D D D D ) |
| ( |
| Medical Research |
| Global Journal of |