1. Introduction
he Mastoid air cells are open spaces containing air that are located throughout the mastoid bone, the prominent bone located behind the ear that projects from the temporal bone of the skull. The air cells are connected to a cavity in the upper part of the bone, which is in turn connected to the middle ear.
Mastoid air cells considered to be an important contributor to the physiology of middle ear function. the mastoid air cell system served as an reservoir of air and serves as buffer system to replace air in the middle ear cavity temporarily in case of Eustachian tube dysfunction. The mean volume of air in the mastoid air cell system could be about 5-8 ml. CT scan evaluation of temporal bone is considered to be the best modality to assess mastoid air cell system (1). problem) and then subsequently involve the mastoid air cells -since they are anatomically connected. Severe cases of the disease may lead to meningitis, which is an infection of the membranes surrounding the brain. Mastoid air cell disease is often diagnosed these days by CT scanning -which shows opacification (e.g. fluid accumulation) in the air cells. (1) A computerized tomography (CT) scan of the mastoid process reveals the air cells as small, dark spaces separated by lighter areas of dense bone cells. Inflamed or infected cells will appear as gray or white areas on the scan where the darkened spaces would be expected to be located. When these abnormal looking cells are present, they are called mastoid cell opacification (2).
Helical CT has become the method of choice for many routine and new clinical applications. It provides good image quality for body imaging applications at table advancement per rotation of 1 to 2 times the x-ray beam collimation (3&4). Using 3D, multiplanar reformation ~MPR! Or maximum intensity projection ~MIP! Techniques would be benefited by improved volume coverage speed performance (3&4). Recent advances in 32, 64 and now 128-slice CT scanners allow the acquisition of high-resolution, volumetric data that allows image reconstruction in any plane. The advent of high-resolution CT scanning in the 1980s has revolutionized diagnostic imaging of the temporal bone. CT scanning offers the greatest structural definition of any currently available imaging modality (5&6). Temporal bone is a complex structure which contains organs for hearing and balance. Large vessels and nerves pass through temporal bone. Because of its complex anatomic structure and functional properties temporal bone is one of the most challenging organs for radiologists to detect diagnostic findings. It is obligatory to have a good knowledge of its anatomy and functions in order to accomplish optimal radiological evaluation (7).
CT is a standard examination technique in diagnosing and treatment of temporal bone diseases (7&8) Slices in different planes can be obtained by CT and it is possible to understand the complex relationship of ana¬tomical structures. Its capability of obtaining slices less than 1 mm and the development of specific examination techniques for restricted density regions increased the imaging rate of detailed examinations. With the advent of multislice CT after gaining axial 3D volumetric scan¬ning coronal and sagittal reformatted slices can be ob¬tained. By this technique total radiation dose can be decreased using 0.5 mm slice thickness. A CT with a sub-milimetric spatial resolution, slice thickness of 2 mm or less, wide window settings, bony detail reconstruction algorithm, having target reconstruction and high quality image reformatting programs is very efficient in evalua¬tion of inflammatory middle ear pathologies (9 &10). The most important advantage of spiral CT in temporal bone imaging is its perfect visualization of the contrast between bony structures and the air in the middle ear. In addition to detailed evaluation of the bony structures it also permits assessment of soft tissue components as well. (8 &11). This study aimed to study the mastoid air cells diseases and their complications using spiral CT, it was conducted in Alfaisal Specialized hospital and Ibn Elhaitham Diagnostic center.
II.
2. Materials & Methods
were therefore obtained with the neck flexed such that the infra-orbito-meatal line was parallel to the scanning plane when obtaining images in the axial plane. A zero degree gantry tilt when obtaining such images ensured no distortion of the post-processed 3D images. Volumerendered 3D images were generated from the original 2D data with different soft tissue and bone All post-processed images, axial scans and coronal MPR were studied by senior technologist and diagnosed by radiologist.
3. ii. Data Analysis
The data were collected by using questionnaire and medical reports and were analyzed by using statistical package of social science (SPSS).
III.
4. Results
This study carried out in 100 patients their ages between (15 to 70) years old, whom suspected of mastoid air cells pathologies using 4 MDSCT (Toshiba medical system), the study was done according to gender, clinical diagnosis, side of lesion, signs & symptoms, anatomical variations and CT diagnosis and the results obtained as following.
were then reconstructed at 2 mm intervals. All studies a) Materials i. Machine Toshiba (4 multi slice detector) Spiral CT scanner which is not different in external appearance from conventional CT scanner However, there are significant differences in several major equipment components
5. Discussion
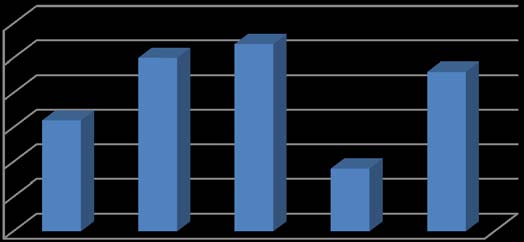
This study was performed in 100 patients (58 female & 42 male) their ages between (15 -70 years) whom suspected of mastoid air cells pathologies and they were referred to CT department centers for CT scan of the temporal bones using 4 MDSCT (Toshiba Medical System) and the results as the following:
The gender distribution was 58 female & 42% male as explained in figure (4.1). 41% of them were diagnosed clinically as having CSOM (figure 4.2) while by CT 28% of them were diagnosed of having chronic mastoiditis & CSOM , 8% were diagnosed of having CSOM, 2% having chronic mastoiditis and 2% having cholesteatoma &CSOM as shown in table(4.1) & figure (4.14).
44 % of patients were diagnosed clinically as having chronic infection (figure 4.2), while by CT, 19% of them were diagnosed as having chronic mastoiditis &CSOM, 14% as having chronic mastoiditis,7% as having cholesteatoma & CSOM and 4% as normal.
10% of patients were diagnosed clinically as having chronic mastoiditis, while by CT they were diagnosed as follows; 6 % of them having chronic mastoiditis & CSOM and 4% of them having chronic mastoiditis, figure (4.14).
5% of patients were diagnosed clinically as having cholesteatoma (figure 4.2), also by CT they were diagnosed as having cholesteatoma (figure 4 This study also relative to (Keskin 2011) who detect 35 patients of scutum erosion by helical CT, 28 patients of them were confirm by surgery.
The tegmen timpani erosion were detected in only 2% of patients as shown in table (4.9) & fig (4.22). Also this result was compared with (Keskin2011), there were no tegmen erosion in surgery among 11 patients whom diagnosed as having tegmen erosion by CT, but no tegmen erosion detected by surgery or CT among 44 patients.
Inner ear and external ear structures changes were very low (2% of patients & 6% of patients) respectively, table (4.10) & (4.11) figure (4.23 & 4.24). These results indicate that the middle ear structures were affected more than the inner and external ear structures, thus there was correlation between middle ear diseases and mastoid air cells diseases.
V.
6. Conclusions
Spiral CT is an effective imaging modality in studying mastoid air cells diseases and their complications. The diseases of mastoiditis with CSOM had higher frequency and also their complications (ossicular erosion, scutum erosion, and loss of hearing). There was correlation between mastoid air cells diseases and middle ear diseases, and with the help of spiral CT it is possible to acquire multiple slices and understand the complex relationships of anatomic structures. CT with a spatial resolution below 1 mm, ? 2 mm slice thickness, wide window, having bone -detail reconstruction program, target reconstruction and high quality image reconstruction programs is very efficient in studing of mastoid air cells and middle ear pathologies. Using 3D, multi-planar reformation ~MPR! Techniques would be benefited to detect and diagnosed the complications of mastoid air cells diseases. The advent of high-resolution CT scanning has revolutionized diagnostic imaging of the temporal bone. Spiral CT scanning offers the greatest structural definition of any currently available imaging modality.

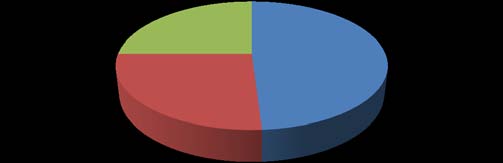
| External ear structure changes | |||||||||||
| Normal Unremarkable | |||||||||||
| 6% | |||||||||||
| 94% | |||||||||||
| 0 10 20 30 40 50 60 Figure (4.14) : Shows CT diagnosis & clinical diagnosis Cross tabulations 53 20 10 6 2 4 5 Frequency Table (4.2) : Demonstrates CT diagnosis * signs & symptoms Cross tabulation | |||||||||||
| CT diagnosis Chronic mastodities | Chronic Ear pain & mastodities swelling 4 | CSOM Ear pin & Chronic mastoiditis & ? Signs & amp; symptoms Cholesteatoma Chronic CSOM & chlesteatoma discharge Ear discharge Eear Normal discharge & swelling mastoidites & ? 5 7 2 | Ear pain & loss of hearing 2 | Total 20 | |||||||
| CSOM | 2 | 2 | CT diagnosis 3 | 2 | 1 | 10 | |||||
| Chronic mastoditis | 8 | 13 | 17 | 5 | 10 | 53 | |||||
| &CSOM | |||||||||||
| Cholestetoma | 1 | 0 | 0 | 0 | 5 | 6 | |||||
| cholesteatoma Chronic mastoidites & | 4.1) : Demonstrates CT diagnosis * Clinical diagnosis Cross tabulation 0 0 0 0 2 | 2 | |||||||||
| CSOM & cholesteatoma | 1 | 0 | 0 | 0 | 3 | 4 | |||||
| Normal | CT diagnosis Total | 0 16 | CSOM | Clinical diagnosis 0 Chronic Infection 5 Cholesteatoma 0 25 27 9 | 0 mastoiditis Chronic 23 | Total | 5 100 | ||||
| Chronic mastodities | 2 | 14 | 0 | 20 | |||||||
| CSOM | 8 | 2 | 0 | 10 | |||||||
| Chronic mastoditis& CSOM | 28 | 19 | 0 | 53 | |||||||
| Cholesteatoma | 0 | 2 | 4 | 6 | |||||||
| Chronic mastoidites & | 1 | 1 | 0 | 2 | |||||||
| cholesteatoma | |||||||||||
| CSOM & chlesteatoma | 1 | 2 | 1 | 4 | |||||||
| Normal | 1 | 4 | 0 | 5 | |||||||
| Total | 41 | 44 | 5 | 10 | 100 | ||||||
| Table (4.7) : Demonstrates CT diagnosis * Ossicular changes Cross tabulation | |||||||||
| CT diagnosis | Ossicular changes Normal Erosion | ||||||||
| Chronic mastodities | 18 | 2 | 20 | ||||||
| CSOM | 04 | 6 | mastoid air cells Abcent 10 | ||||||
| Chronic mastodities Chronicmastoiditis &CSOM CSOM Chronic mastoiditis & CSOM Cholesteatoma Cholesteatoma Chronic mastoidites & cholesteatoma CSOM & cholesteatoma Normal Total | Chronic mastoidites & | cholesteatoma | 40 2 0 2 5 CSOM & cholesteatoma 71 | Normal | 13 4 2 2 0 29 | pnematization mastoid air cells Decreased pnematization mastoid air cells Normal 53 6 2 4 5 100 | |||
| CT diagnosis | |||||||||
| 4.6) : Demonstrates CT diagnosis & middle ear cavity changes cross tabulation | |||||||||
| CT diagnosis | Middle ear cavity changes Obacified Normal | Total | |||||||
| Chronic mastodities | 5 | 15 | 20 | ||||||
| CSOM | 9 | 1 | 10 | ||||||
| Chronic mastoiditis&CSOM | 53 | 0 | 53 | ||||||
| Cholesteatoma | 6 | 0 | 6 | ||||||
| Chronic mastoidites & | 1 | 1 | 2 | ||||||
| cholesteatoma | |||||||||
| CSOM & cholesteatoma | 4 | 0 | 4 | ||||||
| Normal | 0 | 5 | 5 | ||||||
| Total | 78 | 22 | 100 | ||||||
| 0 10 60 Figure (4.20) : Shows CT diagnosis & ossicular changes Cross tabulation 50 40 30 20 Table (4.8) : Demonstrates CT diagnosis * scutum changes Cross tabulation | |||||||||
| Chronic mastodities CT diagnosis Chronic sup otitis Chronic mastodities COM Chronic mastoiditis &CSOM media Cholesteatoma cholesteatoma Chronic mastoidites & | Chronic | mastoiditis&CSOM | Cholesteatoma Normal Chronic mastoidites & 19 10 50 0 0 | cholesteatoma | Normal Scutum changes middle ear cavity Obacified middle ear cavity Normal Total Partial erosion Total erosion 0 1 20 0 0 10 2 1 53 3 3 6 CSOM & chlesteatoma 2 0 2 | ||||
| CSOM & chlesteatoma Normal | 0 CT diagnosis 5 | 1 0 | 3 0 | 4 5 | |||||
| Total | 84 | 8 | 8 | 100 | |||||
| The ossicular changes were detected in 29% of | |
| patients, 14% of them with partial erosion, while 15% of | |
| them with total erosion as shown in figure (4.8).21 patients of them were diagnosed by CT as having | 013 |
| chronic mastoiditis & CSOM while 8patients of them were diagnosed as having cholesteatoma. (Table 4.7 & fig 4.20). | 2 Year |
| study of ( | |
| in diagnosing mastoid air cells diseases. The signs & symptoms was; 77% of patients were having ear pain, discharge & swelling (figure4.3), all of them were diagnosed by CT as having chronic mastoiditis & CSOM, 23% of patients were having ear pain & loss of | Volume XIII Issue III Version I |
| hearing, most of them (13patients) were diagnosed as having chronic mastoditis &CSOM and the others (10 | ( D D D D ) F |
| patients) were diagnosed as having cholesteatoma | |
| (table 4.2 & fig 4.15). | |
| The side of lesions in 49% of patients was | |
| bilateral (fig 4.4), most of them were diagnosed by CT | |
| as chronic mastoiditis & CSOM (table 4.3&fig 4.15), 26% | |
| of them at the right side and 25% at the left one. | |
| The pathological changes on the mastoid bone | |
| was explained as 13patients with mastoid bone | |
| sclerosis (fig 4.5) all of them were diagnosed by CT as | |
| having chronic mastoiditis & CSOM , 6 patients with | |
| mastoid bone erosion 4 of them were diagnosed by CT | |
| as having cholesteatoma & 81 patients with normal | |
| mastoid bones ,as shown in table (4.4 & fig 4.17). | |
| The mastoid air cells changes as follows; 61% | |
| of patients were absent pnematization (figure 4.6), 53 | |
| patients of them were diagnosed by CT as having | |
| chronic mastoiditis & CSOM while 8 patients were | |
| diagnosed as having cholesteatoma, 32% of patients | |
| with decreased pnemataization, 29 patients of them | |
| were diagnosed by CT as having chronic mastoiditis & | |
| CSOM while 3 patients were diagnosed as having | |
| cholesteatoma and 7 patients with normal pnematization | |
| as shown in table (4.5 & figer 4.18)). This result indicate | |
| that the helical CT had effective role in diagnosing | |
| © 2013 Global Journals Inc. (US) |