1. Introduction
V nodal reentrant tachycardia (AVNRT), the most common form of paroxysmal supraventricular tachycardia, is characterized by nearly simultaneous activation of the atria and ventricles. The human compact AV node is small, just 3-5 mm, has a very long rightward posterior extension that travels down to the area between the tricuspid annulus and down to the floor the CS ostium.
In the typical slow/fast AVNRT the rightward inferior extension of the AV node is using for antegrade slow pathway conduction and the fibers crossing the tendon of Todaro for retrograde fast pathway conduction.
The classical electrophysiological definition of the dual nodal pathway represents an abrupt increase of nodal A-V conduction of at least 50 ms between the Atrial and His (AH) potential intervals, with an anterograde block in the fast pathway conduction and selective conduction over the slow pathway. This phenomenon is known as a AH jump. a) Ventricular -Atrial (VA) conduction time A typical AVNRT is considered when the VA interval is measured either from the onset of ventricular activation (on surface ECG to the earliest deflection of the atrial activation in the His bundle electrogram or high right atrium) is < 60 ms, or < 95 ms respectively. Retrograde AV junctional pathways have been characterized as fast (HA interval<100 ms), intermediate (100-200 ms), or slow (> 200 ms).
2. b) Retrograde atrial activation sequence during AVNRT
AVNRT has been traditionally classified as slow-fast or typical AVNRT, and fast-slow or atypical AVNRT, according to the conventional description of dual AV junctional pathways. The fast pathway of the reentry circuit runs superiorly and anteriorly in the triangle of Koch, whereas the slow pathway runs inferiorly and posteriorly close to the coronary sinus ostium. Indeed, in the majority of slow-fast cases of AVNRT, the site of the earliest atrial activation is close to the apex of Koch's triangle, near the AV node-His bundle junction. In the fast-slow form, the site of the earliest atrial activation is usually recorded posterior to the AV node near the orifice of the coronary sinus. c) "Left -Variant" of atypical AVNRT During reentry tachycardia, a small numbers of patients with AVNRT, have eccentric coronary sinus (CS) activation. The earliest retrograde activation site is on the left-sided from the coronary sinus, masquerading as tachycardia using a left accessory pathway. According the recent electrophysiological studies, from the Atrio-Ventricucar (AV) node there are two extensions, infero- The purpose of this study is to assess the incidence of atypical AVNRT with eccentric CS activation, and to determinate the efficacy of the slow pathway ablation in patients with AVNRT with left side extension.
3. II.
4. Methods
The study was conducted from April 2002 to October 2008 at the Clinic for Cardiology, in Skopje, Republic of Macedonia. During a 7 year period 178 consecutive patients underwent electrophysiological study for management of Atrioventricular Nodal reentry tachycardia. The indication for electrophysiology study (EPS) in these patents was symptomatic tachycardia, previous recorded tachycardia with surface electrocardiogram, a) Electrophysiology testing and ablation protocol Informed written consent was obtained in all patients before the procedure. Antiarrhythmic agents were discontinued for at least 4 half-lives. Three 6F quadripolar electrode catheters were introduced into the right femoral vein and positioned in the high right atrium (HRA), His bundle (HB) region, and in the right ventricular (RV) apex. One 6F decapolar electrode catheter was introduced in the left cubital or left subclavian vein for mapping of the coronary sinus (CS).The diagnostic catheters were used for either recording of local electrogram or pacing.
For radiofrequency ablation, a quadripolar electrode catheter with a 4 mm distal electrode and a deflectable tip was used. Radiofrequency (RF) current was generated from ATAKR II (Medtronic). The catheter position was anatomically monitored with fluoroscopy. Surface ECG lead I, II, and V1, and intracardiac electrograms from various sites were simultaneously displayed and recorded on Pruka 4000. (GE Medical) The pacing stimuli were delivered through a programmable stimulator (Bloom Electrophysiology). Complete anterograde and retrograde electrophysiological studies for atrioventricular node (AVN) were conducted in each patient using incremental and extrastimulus testing techniques. Conduction intervals and refractory periods of AVN were measured and defined. After that was performed programmed electrical stimulation was applied in order to induce the clinical tachycardia. Baseline electrophysiological evaluation and tachycardia induction were performed during incremental pacing and extra stimulation (basic cycle length: 400 -600 msec) from the right atrium and right ventricule.
Retrograde atrial activation sequence during atypical left variant AVNRT was determined by the intracardiac electrograms recorded from the high RA (HRA), His-bundle (HB) region and the Coronary Sinus (CS). The earliest retrograde atrial activation site was confirmed by mapping the right side of the interatrial septum and the CS. The absence of accessory pathway was confirmed by basic electrophysiological procedures.
Induced AVNRT's were classified into slowslow, fast-slow, and slow-fast forms according to the previously described criteria b) Slow pathway (SP) ablation
The SP ablation was performed in all patients at the conventional region at the right inferoseptal area between the tricuspid annulus and the CS ostium during sinus rhythm targeting the SP potential.
Inducibility of AVNRT was assessed after each ablation. Successful ablation was defined as elimination of the retrograde SP conduction for at least 30 minutes after the last energy application.
5. c) Statistical Analysis
Data was analyzed using commercially available statistical program. Continuous variables were reported as mean ± SD. Categorical variables were reported as percentages.
6. III.
7. Results
8. a) Patient Characteristics
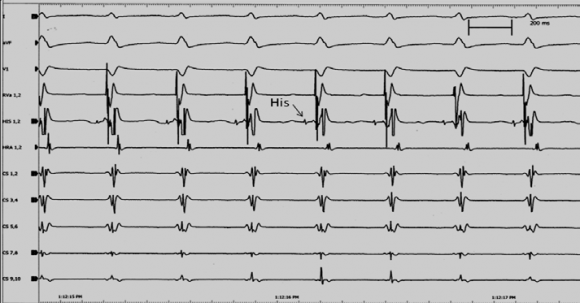
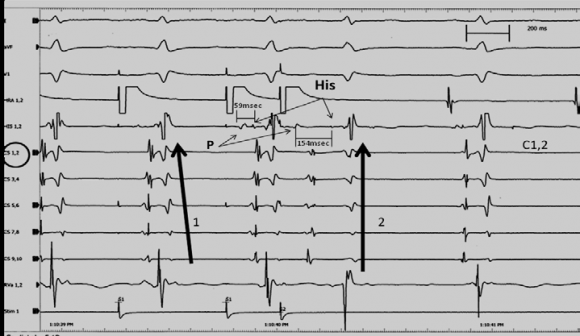
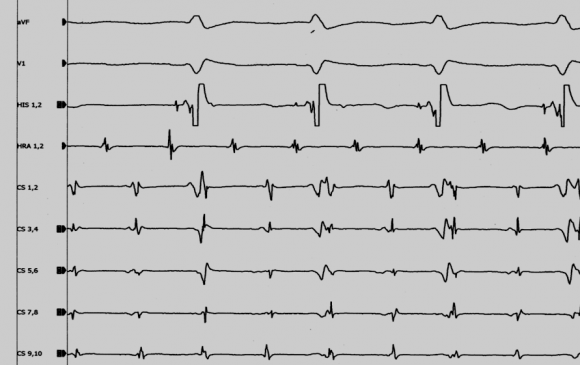
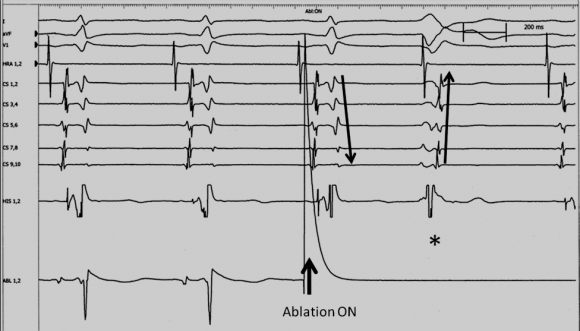
In the group with atypical AVNRT (16 pts), ten patients were with classified as slow/slow AVNRT, and 6 were classified with retrograde left eccentric conduction. (table1). In all patients there was no identifiable underlying heart disease. The basic electrophysiological characteristics are summarized in table 2. All patients showed dual AV node pathways, defined as a AH jump (prolongation of AH interval of more than 50 msec) between two consecutive programmed decremental stimulation cycles with either single or double extrastimuli from right atrium. Retrograde dual AV nodal pathway physiology was also demonstrated by a sudden jump-up in H-A (VA) interval and a simultaneous shift of the earliest retrograde atrial activation site from the superoseptal to the inferoseptal area during ventricular extra stimulation. In the group of AVNRT with LPNE (6 pts), the earliest retrograde atrial activation was recorded at the proximal coronary sinus (C1.2) (fig. 1.2). There was no difference in electrophysiological characteristics in each subform of AVNRT. There were significantly more another atrial arrhythmia (atrial flatter/fibrillation-figure 3) in the group of atypical AVNRT, especially in the subform of LPNE (
9. Patients with Eccentric CS Activation
Typical ablation sites between the tricuspid annulus and the anterior edge of the CS ostium produces accelerated junctional rhythm (rightward inferior extension injury) but fails to eliminate AVNRT. Because of that, delivering of the radiofrequent (RF) energy was in the higher parts in the triangle of Koch. We prefer to reach the target of the leftward inferior extension along the roof of the proximal CS. We avoid positioning the catheter straight upward to the roof or in lumen of CS during ablation because in that position is very easy to injured the fast pathway or ostium of CS. (figure 4). Among six patients with the eccentric CS activation, the SP ablation was performed at the right inferoseptal region during sinus rhythm. In all six patients, accelerated junctional rhythm was induced during energy applications. After the mean of 4,6 ( from 1 to 9 times of the energy application) at the right inferoseptum and midseptum, atypical AVNRT was non inducible. Four of the patients (4/6) atypical AV there was nodal echo beats (one or two). The mean Wenckebach CL of the retrograde SP significantly prolonged after the right inferoseptal ablation. (Before vs. after ablation: 405 ± 63 msec vs 466 ± 37 msec; P = 0.012). There was no complication related to the SP ablation.
10. Post ablation follow up
No recurrence of AVNRT was observed during a mean ambulatory follow-up period of 16 ± 12 months in all 6 patients.
V.
11. Discussion a) Major Findings
In our study, atypical AVNRT was observed in 9% of patients (16/178). The eccentric CS activation pattern was found in (6/16 pts). It's 37.5% of the patients with atypical AVNRT. But only 3.4 % in hole group of AVNRT (6/178 pts) were with left variant. The conventional right inferoseptal SP ablation did not abolish eccentric retrograde conduction from CS, but the clinical tachycardia was not inducible in any of the 6 patients with left variant of AVNRT. Standard right atrium ablation is effective and successful for AVNRT with retrograde left eccentric conduction in the coronary sinus. b) Incidence of eccentric coronary sinus activation pattern in AVNRT Hwang et al. [3] reported that the earliest retrograde atrial activation was recorded within the CS in 0% (0/310 patients) among typical form and in 43% (20/46 patients) among atypical form, while Nam et al. [1] reported its incidence of 6% (3/52 patients) among typical form and 80% (8/10 patients) among atypical form. Chen et al. [5] reported its incidence of 8% (16/211 patients) among typical form and 14% (2/14 patients) among atypical form.
12. c) Slow pathway ablation for atypical AVNRT with eccentric coronary sinus activation
Whether the retrograde left-sided atrionodal connection constitutes the critical component of the reentrant circuit or only an innocent bystander in atypical AVNRT with the eccentric CS activation pattern is controversial. [1][2][3] Furthermore, whether the eccentric CS activation pattern during atypical AVNRT is the hallmark of AVNRTs that require left-sided ablation remains to be elucidated. Jackman et al. [4] reported that the leftward PNE constituted the retrograde limb of the reentrant circuit and the SP ablation at the earliest retrograde activation site within the proximal CS was, therefore, required to eliminate atypical AVNRT with the eccentric CS activation pattern. Conversely, others postulated that the retrograde left-sided atrionodal connection was an innocent bystander; therefore, conventional right-sided SP ablation was sufficient to eliminate inducibility of atypical AVNRTs with the eccentric CS activation pattern. [3,5] . Otomo [6] , among eight patients with the eccentric CS activation, the standard right-sided ablation lengthened the VA Wenckebach CL and rendered atypical AVNRT nonsustained in seven of eight patients (88%), possibly suggesting partial injury to the retrograde eccentric SP induced by the right-sided ablation. The retrograde eccentric SP conduction was eliminated only after the SP ablation at the earliest atrial activation site within the CS.
13. VI.
14. Conclusion
Atrioventricular node reentry tachycardia can be associated with eccentric retrograde left-sided activation, masquerading as tachycardia using a left accessory pathway. In our study, incidence of atypical left variant of AVNRT was 3.4%.We performed standard RF ablation, but a little bit higher in the triangle of Koch, closer to the fast pathway. In that position, ablation in the right atrium is effective and successful for AVNRT
| Result of electrophysiological studies | Patients | % of 178 |
| AVNRT slow/fast | 159 | 89.3% |
| AVNRT slow/slow | 10 | 5.6% |
| AVNRT with retrograde left eccentric conduction | 6 | 3.4% |
| AVNRT with bystander AVRT | 2 | 1.1 % |
| AVNRT with AV node diseased | 1 | 0.26% |
| Total ablated patients | 173 | 97.1% |
| Without ablation | 5 | 2.9 % |
| AVNRT -atrioventricular nodal reentrant tachycardia, | ||
| AVRT -atrioventricular reentry tachycardia |
| 013 |
| 2 |
| Year |