1.
These activities are due to NK cells (antibodydependent cellular cytotoxicity (ADCC)) or complement (complement-dependent cytotoxicity (CDC)). These activities might not be the original therapeutic intent of monoclonal antibody treatment; however, it is desirable to enhance these activities if possible.
ADCC activity is dependent on specific antibody and NK cell activities. For example, Cetuximab promotes ADCC activity on cancer cells. The enhancement of NK cell activity can be difficult. We previously reported the use of daily interleukin-2 (IL-2) injections to enhance NK cell activity; however, it is very complicated clinically.
Recently, some herbal drugs were found to stimulate immunological activities. Polysaccharide K (PSK) is obtained from the mushroom Trametes versicolor and reportedly enhances ADCC activity 1 , but the mechanism is still unclear. Some reported that it increased the number of NK cells, and others reported that it enhanced NK cell activity. Oral intake of PSK has been clinically used for colorectal cancer therapy when combined with 5-FU [2][3][4] . Here, we evaluated PSK's anticancer effect on gastrointestinal cancer cell lines in vitro and in vivo and discuss the therapeutic possibility of PSK combined with Cetuximab.
2. II.
Materials And Methods a) Cell Lines DLD1, COLO320, COLM-5 and HT-29, human colon cancer cell lines, and GLM-1, MKN-28 and MKN-45, human gastric cancer cell lines, were used in this study. Among them, those cell lines positive for EGFR expression were emphasized. DLD1, COLO320, MKN-28 and HT-29 were purchased from RIKEN Cell Bank (Tsukuba, Japan), GLM-1 and COLM-5 was kindly provided by H. Nakanishi (Aichi Cancer Center Research Institute, Japan; Ito et al., 2010). These cells were maintained in DMEM (Nissui Pharmaceutical Company, Tokyo, Japan) supplemented with 10% FBS (Gibco, Grand Island, NY), 100 units/mL penicillin, and 100 µg/mL streptomycin in plastic dishes (BD Falcon; Introduction he use of monoclonal antibodies in the clinic has changed approaches to cancer chemotherapy. Specific, targeted antibodies can block signals from growth factor receptors by competing for receptor binding. Many kinds of monoclonal antibody chemotherapies have been established.
Cetuximab (Erbitax) is one of the available antiepidermal growth factor receptor (EGFR) monoclonal antibodies that is used for treatment of tumors. Cetuximab is used commonly for treatment of colorectal cancer patients. There are two types of monoclonal antibodies for colorectal cancer therapy, anti-VEGF monoclonal antibody (Bevacizumab) and anti-EGFR antibody. Whereas Bevacizumab is usually used as a first or second line treatment combined with Oxaliplatin or Irinotekan, anti-EGFR antibodies are used as third line therapy. However, these anticancer treatments remain inadequate.
The primary anticancer mechanism of therapeutic antibody treatment is inhibition of growth factor signals. In addition, several monoclonal antibodies have immunological activities.
T BD Biosciences, Franklin Lakes, NJ) and incubated at 37?C in 5% CO 2 b) Agents . After evaluation of cell surface EGFR expression by flow cytometric analysis, the cell lines with highest expression of EGFR were evaluated in the following proliferation assays and in vivo assays.
PSK was obtained from Kureha Corporation (Tokyo, Japan). Cetuximab (two mg/mL) was purchased from Merck (Darmstadt, Germany). These two drugs are clinically used at a dosage of three g/ person and 400 mg/m 2 c) Flow Cytometry , respectively.
Flow cytometric analysis was performed to evaluate the expression of EGFR on the cell surface of each cell line. Tumor cells were harvested with trypsin/EDTA and washed twice with buffer (five mM EDTA, five mg/mL bovine serum albumin in PBS) and reacted on ice with mouse anti-human EGFR monoclonal antibody (NeoMarkers) as the primary monoclonal antibody for 30 min. After washing twice with buffer, cells were incubated on ice for an additional 30 min with PE-conjugated polyclonal goat anti-mouse IgG, F(ab') 2 d) Cell Growth Assay as the secondary antibody (Jackson ImmunoResearch, West Grove, PA). The labeled cells were then washed, and the intensity of fluorescence was evaluated with a FACSCalibur (BD Biosciences, San Diego, CA).
Cancer cells were harvested with trypsin/EDTA, plated at 5 x 10 4 e) Animals cells/24-well plastic plate (BD Falcon) in DMEM supplemented with 10% FBS on day 0, then treated with a range of doses of PSK (5, 10, 50, 100 and 500 µg/mL) or Cetuximab (1, 5, 10, 50 and 100µg/mL) on days one and three. Both the total number of cancer cells and viable cells were measured in triplicate on day four with an Automated Cell Counter (Bio-Rad). Viable cells in controls, 500 µg/mL PSK, and 100 µg/ of Cetuximab were also counted with the Trypan blue exclusion procedure.
Five-to six-week-old male athymic nude mice of the KSN strain were purchased from Japan SLC (Hamamatsu, Japan) and maintained under specific pathogen-free conditions. The health of the mice was monitored by daily observation. Chlorinated water and food autoclaved for five min were provided ad libitum, and the animals were kept in a controlled light : dark cycle (
3. Results
cells in 0.2 mL Hank's balanced salt solution (HBSS) were injected subcutaneously (sc) into the left abdominal flanks of male nude mice. When the subcutaneous tumors developed to approximately eight mm maximal diameter, treatment with intraperitoneal injection (ip) of Cetuximab (one mg/ mouse, twice a week) or PSK alone (2.5 mg/mouse, every two days) or a combination (same doses as above) or vehicle (ip, 400 ?L/mouse, twice a week) was performed for four to five weeks (6 mice/group). The maximal tumor diameter (L) and the right angle diameter to that axis (W) were measured twice a week. Tumor volume was estimated by the following formula: L x W x W x 1/2. Mice were sacrificed after five weeks of treatment according to the ethical guideline of UKCCR as described above. Subcutaneous tumors were then removed and weighed.
4. a) Flow Cytometric Analyses
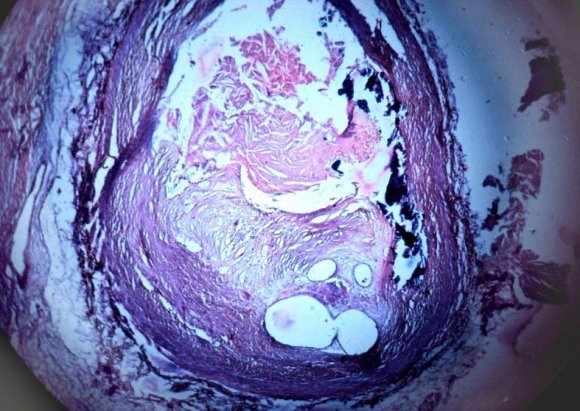
The expression of EGFR on the cell surface was evaluated by flow cytometry. Expression was the highest on MKN-28 and HT-29 in gastric and colorectal cancer cell lines, respectively (Fig. 1). Thus, we used these two cell lines in the following assays.
5. b) Proliferation Assay
We evaluated MKN-28 and HT-29 cell growth using several concentrations of Cetuximab (one to 100 µg/mL), or PSK (five to 500 ?g/mL) (Fig. 2). Neither Cetuximab nor PSK alone showed in vitro antitumor cell growth activity with MKN-28 or HT-29 even at the maximum concentrations. The numbers of viable cells in the control group and in the highest concentration of PSK (500 ?g/mL) were almost the same. On the other hand, Cetuximab suppressed tumor cell growth in a dose-dependent manner. However, the suppression was incomplete. c) Tumor Xenografts Xenografted tumor sizes are shown in Fig. 3. Tumors were xenografted subcutaneously in the mouse inguinal region and were resected and evaluated after treatment. In both HT-29-and MKN-28-induced tumors, PSK alone failed to suppress tumor growth compared with the control group. Cetuximab alone did very little, and the difference was not significant statistically. However, when PSK was added to Cetuximab, the anticancer effect of combination therapy was enhanced remarkably (p=0.01, compared with Cetuximab group), as tumor volume was reduced 41% in HT-29 and 42% in MKN-28 compared with those control group. Similar results were seen in tumor weights. The resected tumor weights of control, PSK alone and Cetuximab alone groups were not different significantly. However, the weights of tumors in the HT-29 and MKN-28 groups treated with a combination of drugs were 42% (p=0.01) and 51% less than the control groups, respectively.
6. IV.
7. Discussion
Chemotherapy for colorectal cancer patients has changed dramatically over the past decade. Oxaliplatin and Irinotecan are used in two standard therapies as FOLFOX and FOLFIRI, respectively. Furthermore, two kinds of monoclonal antibodies, anti-VEGF antibody and anti-EGFR antibody, can make variation for these standard therapies [5][6][7] . Currently, the survival of patients with unresectable or recurrent colorectal cancer can be prolonged more than two years 8 .
Many kinds of monoclonal antibodies have been established as therapeutic drugs. Some of them are used for neutralization of certain ligands, and others are used to block cell surface signals. There are many receptors on cancer cell surfaces that promote cell proliferation via activation and the initiation of downstream signal cascades. Many monoclonal antibodies against these receptors function by attaching to the cancer cell surface and blocking these signals.
On the other hand, some of these monoclonal antibodies possess an Fc region that can stimulate NK cells and enhance ADCC activity. Thus, Bevacizumab, which neutralizes VEGF cannot promote ADCC, and anti-EGFR antibody can.
Cetuximab and Panismumab are well-known anti-EGFR antibodies used for the treatment of colorectal cancer patients. The anticancer effect is caused by the inhibition of EGFR signaling. Cetuximab and Panismumab are structurally different. Whereas Cetuximab is a chimeric IgG 1 antibody, Panismumab is a complete human monoclonal IgG 2 antibody. Whereas Cetuximab might cause allergic or anaphylactoid reactions, the structure contributes to immunologic anticancer effects, such as CDC and ADCC 9,10 . However, there has not been a significant difference in outcome between Cetuximab and Panismumab when they were used under standard clinical conditions 11 . We previously reported that Cetuximab activity can be enhanced in gastric cancer when NK cell activity is stimulated by daily injections of IL-2 12 . However, daily use of IL-2 is clinically difficult.
An herbal drug, PSK, is obtained from a species of mushroom. This drug is administered by daily oral intake and has been used safely in Japan for cancer therapy. However, its antitumor activity has not been clarified. Recent studies have revealed that PSK can induce apoptosis in a pancreatic cancer cell line 13 . Polysaccharide K has also been known to stimulate a patient's immune system. Polysaccharide K has been used in Japan for treatment of gastrointestinal cancer.
The drug is usually used with another chemotherapeutic drug such as 5-FU. Some investigators have reported that PSK stimulates NK cells and enhances ADCC activity. Our study showed that PSK or Cetuximab alone had no remarkable suppressive activity on HT-29 in vitro. Furthermore, PSK alone had no anticancer effect on either cell line following subcutaneous xenografting in mice. Cetuximab decreased tumor volume compared with controls, however the difference was very small. On the other hand, combination therapy of PSK and Cetuximab showed significant tumor growth suppression. One possible reason of this result is caused by ADCC.
Anti-EGFR monoclonal antibody is not recommended for use in colorectal cancer patients who have a mutation in KRAS 14 . This is because blocking EGF signaling by EGFR is not useful when EGF signaling is constantly activated by this mutation. Thus, these patients currently have no choice for third line therapy after earlier failures. However, ADCC is not influenced by KRAS mutations. Thus, this combination therapy might provide an option for patients carrying a KRAS mutation and who otherwise could not undergo anti-EGFR therapy as third line treatment.
V.
8. Conclusions
As with monoclonal antibodies, PSK's synergic activity enhanced Cetuximab's anticancer effect on a gastrointestinal cancer cell line's growth in vivo. This might be an option for Cetuximab therapy for colorectal cancer patients. The expression of EGFR on the cell surface in various cell lines.
9. Volume Issue III Version I
These cell lines had differing levels of expression of EGFR. Among colorectal cancer cell lines, HT-29 had the highest expression, and among gastric cancer cell lines, MKN-28 was highest. The proliferation of HT-29 in several concentrations of PSK or Cetuximab.
HT-29 cells were cultured with several concentrations of PSK (5, 10, 50, 100 or 500 µg/mL) or Cetuximab (1, 5, 10, 50 or 100µg/mL). PSK had no suppressive activity on the proliferation of HT-29. Even at the highest concentration, viable cell numbers (VC/ total cell) of PSK 500 µg/mL (97%, grey bar) were almost the same as that of controls (95%, grey bar). On the other hand, Cetuximab suppressed both proliferation of HT-29 and the proportion of viable cells in 100µg/mL (52%, grey bar) compared with that of control (94%, grey bar). However, the number of total cells was not different significantly. Tumor volumes were measured after a four-or five-week treatment (vehicle; PSK alone: 2.5 mg/ mouse every two days; Cetuximab alone: one mg/mouse twice/week; PSK and Cetuximab combined). Tumors in the control, PSK alone, and Cetuximab alone groups were not significantly different after xenografting either HT-29 or MKN-28 cells (A, B). However, growth was significantly suppressed when PSK was used with Cetuximab (p=0.01). Similar results were seen in tumor weight (C and D). Cx: Cetuximab,


| f) Animal Experiments |
| To examine the anti-tumor activity of Cetuximab |
| and PSK in vivo, growing tumor cells were harvested |
| with trypsin-EDTA, washed with PBS, and 5 x 10 6 |
| III. |