1. Introduction
alaria is a mosquito-borne parasitic disease. In India it is mainly caused by P.vivax and P.falciparum. Complicated malaria characterized by serious organ failures or abnormalities in the patient's blood or metabolism,usually occurs in P.falciparum malaria. Manifestations of severe malaria include cerebral malaria, severe anemia, hemoglobinuria, AR-DS, thrombocytopenia, cardiova-scular collapse and shock, acute kidney injury, metabolic acidosis and hypoglycemia.
In contrast to falciparum malaria, vivax malaria is rarely associated with serious complication. Scattered cases of P.vivax causing severe malaria have been reported in the last 30 years.
Manifestations of malaria vary from asymptomatic infection to severe malaria. The essential pathologic feature of severe malaria is sequestration of erythrocytes, which contain mature forms of the parasite in the deep vascular beds of vital organs and rosette formation, thus producing organ dysfunction.
P.vivax may no longer be a paradigm for uncomplicated malaria. Presence of thrombocytopenia in acute febrile travelers returning from tropical areas has become highly sensitive marker for malaria diagnosis (D' Acremont et al.2002).The sensitivity of thrombocytopenia together with the acute febrile illness was 100% for malaria diagnosis, with specificity of 70%, a positive predictive value of 86% & a negative predictive value of 100% (Patel et al 2004).
Since the beginning of the 1970s, there have been reports proposing that malaria associated thrombocytopenia is quite similar in P.vivax and P.falciparum infections (Beale et al 1972). Most of the data were published in late 1990s because of an availability of affordable automated machines capable of performing complete blood count (CBC). 6). The TROPHOZOIT form followed by RING form is predominantly seen in the PBF study. The least common form of the parasite is GAMATOCYTE. While most of the time one or more types of the form of parasite are found together in the peripheral blood smear study.
2. II.
3. Material & Methods
IV.
4. Discussion
? Organ dysfunction is characteristic of P.falciparum malaria & unusual in P.vivax infection. Severe complicated malaria is a well-recognized feature of P.falciparum malaria. Although a few cases with P.vivax have been reported in literature. Any patient infected with P. vivax who exhibits severe malaria is presumed to be suffering from mixed infection [5]. However, that may not be always true. As evident from the present report, P.vivax infection can also present with complications. ? Clinical data indicates that P.vivax can cause both sequestrations related and non-sequestration related complications of severe malaria [4]. The exact pathogenetic mechanism however remains elusive. Sachdev and Mohan [6] studied the clinicolaboratory profile of patients with P.vivax cerebral malaria. Focal neurological signs were observed in one patient. Recently a case of cerebral vivax malaria that presented with status epilepticus has been described [7]. ? P.vivax malaria without any complication has been reported many times, even remains silent [8]. It may be presented occasionally with mild anemia or febrile illness. However, none of them had any evidence of thrombocytopenia, AKI and recovered without any sequel [8,9]. ? However almost all type of complications have been found in this study, but more common one is thrombocytopenia. ? There are reports of thrombocytopenia occurring as a manifest of P.vivax malaria in adults. The mechanism of thrombocytopenia (figure 9) in malaria is not clearly known?.
1. Decreased thrombopoiesis, although this hypothesis was later ruled out [9,10] 2. Thrombocytopenia is a result of peripheral destruction in which immune complexes generated by malarial antigens lead to sequestration of the injured platelets by macrophages in the spleen, although this mechanism has not been systematically evaluated in P.vivax malaria [1,11] . 3. An inverse relationship between elevated parasite levels and decreased platelet counts observation consistently has been reported for P.vivax infection [12].
? Fajardo and Tallent [9] in 1974 demonstrated P.vivax within platelets by electron microscopy and suggested a direct lytic effect of the parasite on the platelets. Both non-immunological destruction [13] as well as immune mechanisms involving specific platelet-associated IgG antibodies that bind directly to the malarial antigen in the platelets has been recently reported to play a role in the lysis and the development of thrombocytopenia [14]. ? Oxidative stress damage of thrombocytes has also been responsible based on the finding of low levels of platelet superoxide-dismutase and glutathione peroxidase activity and high platelet lipid peroxidation level in malaria patients, when compared to those of health subjects [15]. ? Malaria may cause anemia and hyperbillirubinemia because of the loss of red blood cells. Intravascular hemolysis & DIC in P.vivax malaria can cause ARF, which occurs more in P.falciparum malaria but we found 8% cases in p.vivax infection [10] . Renal ischemia is the dominant pathogenic mechanism that results in acute tubular necrosis. The prognosis of ARF in P.vivax malaria is favorable.
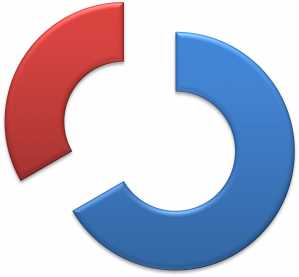
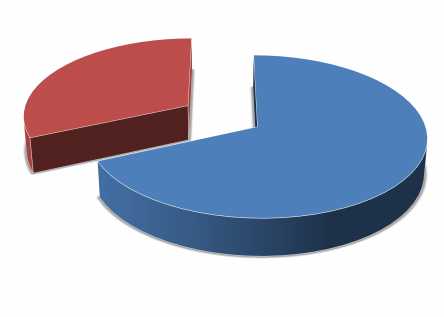
? P.vivax may no longer be a paradigm for uncomplicated malaria. It has been observed that the burden of complicated P.vivax malaria is progressively increasing. ? Complications are common in the form of Thrombocytopenia(71.33%), Anemia (10%), hyperbillirubinemia(8.67%), Acute renal failure(8%) and cerebral malaria(1.33%) in their respective order. As far as the thrombocytopenia is concerned, it is having favorable prognosis & most of them were recovered with only antimalarial treatment so routine use of platelet transfusion is not recommended in a case of thrombocytopenia. ? P.vivax now a days emerging as one of the cause of isolated thrombocytopenia. It is a challenge to differentiate P.vivax from falciparum malaria and Dengue fever.
No.of pts.