1. Introduction
hyroid enlargement is a common occurrence in most regions of the world including India. Being tertiary care hospital we frequently encounter such cases because southernGujarat and surrounding mountainous areas are one of the endemic goitrebelt in India.
Thyroid lesions are one of the most common lesions subjected to the cytopathology as Fine needle aspiration cytology (FNAC) is the first line investigation apart from other investigations like ultrasonography (USG), thyroid function tests, thyroid scan, and antibody levels are done subsequently to select the patients who require surgery and those that can be managed conservatively. [1,2] For the primaryevaluation of patients FNAC has proven to be a rapid, cost-effective, safe and reliable method of investigationlikein lesions of breast, lymph nodes and others. [3,4] However, the success of FNAC is dependent on several important contributing influences including aspirator experience, skilful interpretation rational analysis and its application in management. Data from the Surveillance Epidemiology and End Results (SEER) registry show an increasing prevalence of differentiated thyroid cancer worldwide, [5,6] The increasing prevalence of thyroid cancer and improvements in the technology and resolution of ultrasound machines have led to an increasing number of cytological diagnostic procedures. [7] So being the primary investigation, interpretation and application of FNAC findings is very crucial for further management of thyroid lesions especially for ruling out need of surgery. Uniform communication amongst the cytopathologist, surgeons, endocrinologists, radiologists, and other health care providers will eliminate confusion regarding management. Few borderline thyroid lesions often create confusions regarding treatment. To eliminate such dilemma National Cancer Institute USA in 2007 conference meet was organised in Bethesda with one of the objectives beingto standardize the diagnostic terminology for the reporting of thyroid cytopathology results. The recommendations resulting from this conferenceled to the formation of The Bethesda System for ReportingThyroid Cytopathology (TBSRTC). This classificationscheme has achieved its purpose of standardization of thyroid-reporting cytopathology, as evidenced by several publications. [8] Materials and Method: During period of 1 year from 1 st January to 31 st December 2012 aspiration cytology has been carried out in 160 thyroid swellings referred to cytology department of a tertiary care hospital in Surat. Fine needle aspiration cytology was performed using mainly non-aspiration and aspiration techniques. All the cases were reported using TBSRTC. Cases were followed whenever possible.
Observations and Results: The cytological samples were assessed by qualified consultant pathologists and were categorized in category 1 to 6,six tier system according to TBSRTC criteria given by National Cancer Institute USA. Fine needle aspiration cytology analysis revealed 149 (93.12%) non-neoplastic and 11(6.88%)neoplastic lesions. Major bulks of 140 cases (87.5%) were of category II. Conclusion: Application of TBSRTC bridges the gap in communication amongst the cytopathologist, endocrinologists, surgeons, radiologists, and other health care providers not only in the confined region but also worldwide and leaves no confusion regarding management of thyroid lesions. Few of the borderline lesions often create the confusion which are eliminated by TBSRT. implementation of TBSRTC. Current study was mainly focussed to study the role of reporting system.
2. II.
3. Material and Method
Study includes 160 cases of thyroid swellings patients referred to the cytopathology section of pathology department in a tertiary care hospital in southern gujarat between January 2012 and December 2012. Patient's details regarding history, clinical examination, thyroid function tests, clinical diagnosis, FNAC and histological data whenever possible were noted. The data were analysed in simple statistical tables.
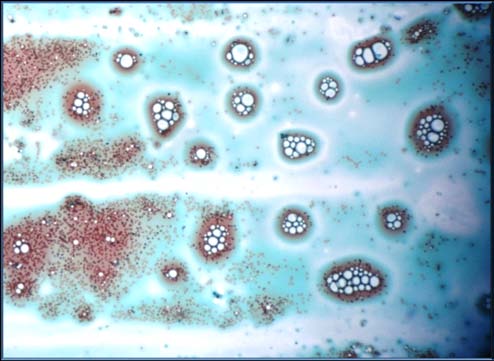
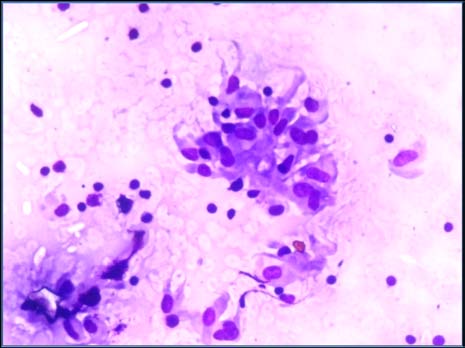
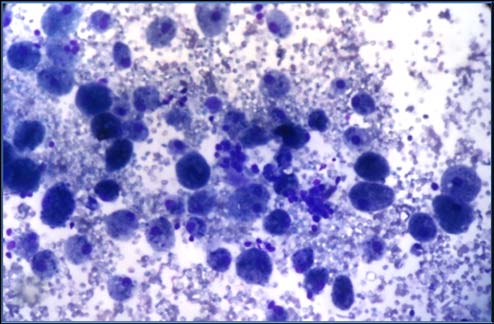
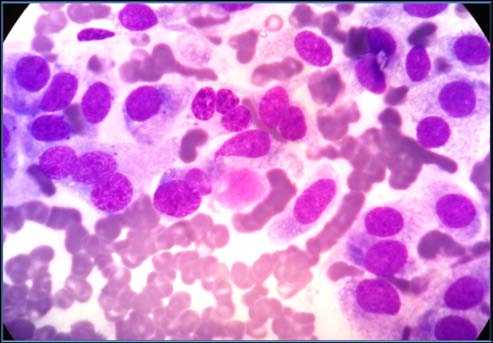
All the cases of thyroid swelling subjected to FNAC were performed by cytopathologist. Prior to procedure, palpation was carried out to note the mobility of the thyroid during swallowing and the presence of any enlarged cervical lymph node. The patients were made to lie supine with their necks stretched up. A 23-24 gauge needle was used, with non-aspiration technique in most cases and very few cases with aspiration technique by a 10 ml disposable syringe. Two or more passes at different sites were made in each case. No major complications like penetration injury to the trachea, laryngeal nerve, or hematoma were recorded. Slides were prepared from aspirated material. In the case of cystic nodules, the cysts' contents wereaspirated, centrifuged, and slides made from the sediment for cytological examination. The slides were stained with MayGrunwald Giemsa (MGG), Papanicolou [PAP] stain and Haematoxylin and Eosin (H&E) and examined under light microscope. The microscopic diagnosis was interpreted under guidelines laid down by TBSRTC including categories I to VI (table 1) after taking into account of all available clinical, radiology and other data. Whenever possible, further sub typing was given.The cytological diagnosis were correlated with clinical features, thyroid function tests, subjected to histopathological examination whenever possible.
4. III.
5. Results
Study includes 160cases with age rangebetween 5 to 70 years. Maximum cases were in 21 -50 years of age group. Bulk of the cases were females comprising of 136 cases (85%) and 24 cases (15%) weremales and female: male ratio was 5.67:1. Long standing history of thyroid swelling was the main presenting symptom. Swelling was mainly diffuse and nodular in few cases. Symptoms like pain in the neck region, dysphagia, hoarseness of voice and cough were rare.
FNAC of 160 patients yielded the following diagnosis as depicted in Table 1.
6. IV.
7. Discussion
As in management of thyroid lesions, FNAC is the gold standard and primary investigation of choice along with other investigations like (USG) ultrasonography examination, thyroid function tests, thyroid scan, and antibody levels are done subsequently to find out patients who require surgery and those that can be managed conservatively. [1,2] Being a tertiary care hospital we have many patients of thyroid disorders from the South Gujarat region including Bharuch, Vapi, Songadh, Vyara and other goitre belts. Majority of these lesions are usually benign and require no aggressive treatment. So interpretation in each case is very crucial for further management Also we want to establish uniform communication between the pathologist, radiologist, endocrinologist, surgeons and treating physicians. So that there would be no confusion regarding further management.
TBSRTC is a vital guideline which can bridge the communication gap and useful to maintain uniformity not on in the confined region but also worldwide. We followed the TBSRTC guidelines and every case was classified according to six tier reporting guideline from category I to VI.
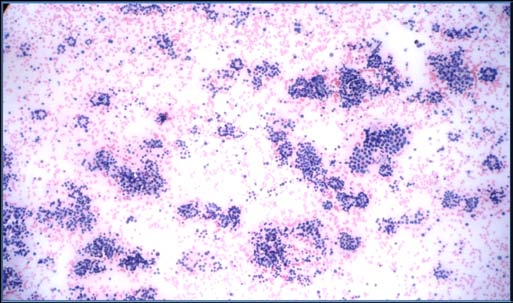
Study includes total 160 cases of thyroid lesions which comprised of 140 cases (87.5%) of total. Published data suggest FNA has an overall accuracy rate around 75% in the detection of thyroid malignancy. Category II: It included most of the study cases with 140 cases (87.5%) of total. Age ranges with maximum number of cases were in 20-50 year age group. It consists of 'non-neoplastic' or 'negative for malignancy' cases like colloid goitre with 97 cases (69.29%), Thyroiditis with 36 cases (25.71%) and Adenomatoid goitre 7 cases (5%). All of these benign cases were just followed up and surgery was prevented.
Category III: It includes lesions which were not clearly benign or malignant. Conclusive opinion was not possible. We did not have any case diagnosed in this category.
Category IV: It includes 5 cases(3.12%) of follicular neoplasm (FN) and suspicious of follicular neoplasm (SFN). The age group which was studied ranged from 5 years to 70 years and maximum no. of cases were in the age group 20-50 years means bulk of thyroid diseases were frequently encountered in young and middle aged group also the majority of cases were the females in reproductive age groups. In present study a female preponderance was noted. Similar female preponderance was noted by Unnikrishnan et al. [10] Neoplastic lesions were 11 cases (6.88%). The benign cyst consistent with thyroglossal cyst were 4 cases (2.06%) and others were 4 cases (2.06%). The bulk of the goitre cases were in the age group of 20-50 years and thyroiditis cases were in 11-40 years and mainly in the reproductive age group of the females.
Category I: This category includes cases in which sufficient material was not available like insufficient follicular cells (Satisfactory for evaluation: six groups of well visualised follicular cells with at least ten cells per group), cyst fluid only, obscuring blood, only macrophages, preparation artefact. In such cases repeat FNA was carried out under ultrasound guidance.
Category II: Majority of lesions were benign mainly of colloid goitre 97 cases (69.29%) out of 140. In comparison to various studiesbenign category includes 60-70% [8] reason for that is we have goitre belt here. Similar findings were observed Unnikrishnan et al. [10] The chances of thyroiditis after reproductive age appeared minimal from this study.
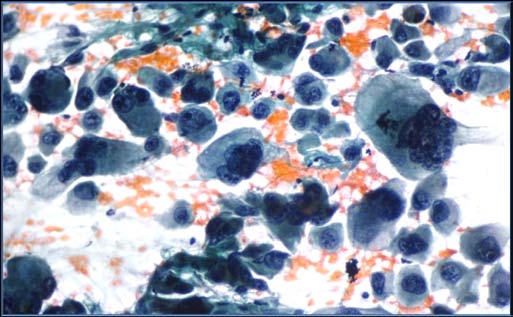
Category III: It is reserved for specimens that contain cells (follicular, lymphoid, or other) with architectural and/or nuclear atypia that is not sufficient to be classified as suspicious for a follicular neoplasm, suspicious for malignancy, or malignant. Management in such lesions is repeat FNAC after an appropriate interval. To be noted that this category is of last resort & should not be used indiscriminately. [8] Category IV: The goal of this category is to identify all potential follicular carcinomas and refer them for a diagnostic lobectomy. Although these cytomorphologic features do not permit distinction from a follicular adenoma (FA), they are reportable as Follicular Neoplasm (FN) or suspicious of Follicular Neoplasm (SFN), leading to a definitive diagnostic procedure, usually lobectomy. [11,12,13] The term SFN is preferred by some laboratories over FN for this category because a significant proportion of cases (up to 35%) prove not to be neoplasms but rather hyperplastic proliferations of follicular cells, most commonly those of multinodulargoiter. [14][15][16][17] About 15% to 30% of cases called FN/SFN prove to be malignant. [11,14,16] The majority of FN/SFN cases turn out to be FAs or adenomatoid nodules of multinodulargoiter, both of which are more common and outnumbers the Follicular carcinoma. Category V: FNAC can diagnose many of the thyroid cancers with fair accuracy, especially papillary thyroid carcinoma (PTC) which can be diagnosed with certainty by FNA. But the nuclear and architectural changes of some PTCs are subtle and focal. This is particularly true of the follicular variant of PTC, which can be difficult to distinguish from a benign follicular nodule. [18] Other PTCs may be incompletely sampled and yield only a small number of abnormal cells. [19] If only 1 or 2 characteristic features of PTC are present or if they are only focal and not widespread throughout the follicular cell population, or if the sample is sparsely cellular, a malignant diagnosis cannot be made with certainty. Such cases occur with some regularity, and they are best classified as suspicious for malignancy," qualified as "suspicious for papillary carcinoma." Such cases suspicious for papillary carcinoma are resected by lobectomy or thyroidectomy. Most (60%-75%) prove to be papillary carcinomas, and the rest are usually FAs. [11,14,16] The same general principle applies to other thyroid malignancies like medullary carcinoma and lymphoma, but these are less frequent than PTC. Such cases were considered after correlating the other findings like serum calcitonin and calcium levels and other relevant data in medullary carcinoma.
8. Category VI:
The malignant category is used whenever the cytomorphologic features are indicative of malignancy. After confirming the malignancy the sub classification was done after summarizing all the results. Approximately 3% to 7% of thyroid FNAs have conclusive features of malignancy, and most are papillary carcinomas. [11,14] Malignant lesions are usually treated bythyroidectomy, with some exceptions (e.g., metastatic tumors, non-Hodgkin lymphomas, and undifferentiated carcinomas). According to studies the positive predictive value of a malignant FNA interpretation is 97% to 99%.
We here practiced mainly the non-aspiration technique in almost all cases for studying cytology and found that it is better than aspiration technique. Aspiration technique is associated with low cellularity and more blood as compared to non-aspiration method. We recommend the non-aspiration method for FNAC of thyroid lesions. Similar suggestions by different studies like Maurya et.al [20] also recommend the non-aspiration technique better for thyroid lesion evaluation by FNAC. The study found thatit is difficult to differentiate follicular/Hurthle cell adenoma from carcinoma on cytological assessment because cytology cannot evaluate the criteria of vascular or capsular invasion or of intrathyroid spread. But the papillary carcinoma, Anaplastic carcinoma and medullary carcinoma can be diagnosed by characteristic cytological features.
V.
9. Conclusion
TBSRTC is a vital guide for accurate management of thyroid lesions. Classifying the lesions in six categories and following the guidelines given by The Bethesda USA meetings solves all problems regarding the management of thyroid lesions and leaves no confusion. It plays a big role in establishing the uniform communications between the managing medical personnel. Marked cellularity of the smear is the problem inherent in thyroid FNAC. Increased cellularity of the smear and loss of cohesion may be present in hyperplastic/adenomatous goiter and follicular neoplasm which causes difficulty in differentiating them. This can be solved by using The Bethesda System of Reporting thyroid lesions. We experienced that The Bethesda Reporting Systemisbest for management of thyroid lesions as it gives uniform reporting system. I-Non diagnostic or unsatisfactory, II-Benign, III-Atypia of undetermined significance or Follicular lesions of undetermined significance, IV-Follicular neoplasm or suspicious of follicular neoplasm, V-Suspicious of malignancy, VI-Malignant lesion.

| 2014 | ||||||||||
| Year | ||||||||||
| 16 | ||||||||||
| Volume XIV Issue I Version I | ||||||||||
| ( ) C | ||||||||||
| Medical Research | ||||||||||
| Global Journal of | Age in | Male Female | I | II | III | IV | V | VI | Total | |
| years | ||||||||||
| 1-10 | 1 | 1 | 0 | 2 | 0 | 0 | 0 | 0 | 2 | |
| 11-20 | 2 | 5 | 0 | 6 | 0 | 0 | 0 | 1 | 7 | |
| 21-30 | 4 | 43 | 2 | 44 | 0 | 1 | 0 | 0 | 47 | |
| 31-40 | 11 | 41 | 4 | 45 | 0 | 0 | 1 | 2 | 52 | |
| 41-50 | 4 | 27 | 1 | 25 | 0 | 3 | 0 | 2 | 31 | |
| 51-60 | 1 | 8 | 0 | 8 | 0 | 1 | 0 | 0 | 9 | |
| 61-70 | 1 | 11 | 2 | 10 | 0 | 0 | 0 | 0 | 12 | |
| Total | 24 | 136 | 9 | 140 | 0 | 5 | 1 | 5 | 160 | |
| (15%) | (85%) | (5.63%) | (87.5%) | (0%) | (3.12%) | (0.63%) | (3.12%) | |||
| Diagnostic | Cytological diagnosis | Risk of | Clinical management |
| category | malignancy | ||
| I | Non-diagnostic or | 1-4 % | Repeat FNA with |
| Unsatisfactory | ultrasound guidance | ||
| II | Benign | 0-3 % | Clinical follow-up |
| III | AUS/FLUS* | 5-15 % | Repeat FNA |
| IV | FNS/SFN ¶ | 15-30 % | Surgical lobectomy |
| V | Suspicious of malignancy | 60-75 % | Near total thyroidectomy |
| or Surgical lobectomy | |||
| V | Malignant | 97-99 % | Near total thyroidectomy |