1.
Evaluation of the Effectiveness of Lateral Intercrural Suture to Reduceinterdomal Distance in Order to Improve Nasal Tipdefinition on Primary Rhinoplasty
2. I. Introduction
hinoplasty is one of the most commonsurgeriesin our field and its demand requires wider studies aiming at offer to the patient more durable, consistent, predictable and harmonic results. The nose, focus of several studies, must also present an aesthetical balance, dynamic and functional; especially because nasal tip represents the main motive for postoperative dissatisfaction. (GARCIA, 1983). 1 In addition to aesthetics analysis, the surgeon must evaluate the respiratory function in order to provide an aesthetically balancedand functionally efficient nose. (PITANGUY, 1981) 2 The treatmentof the nasal tip is one ofthe most important components on rhinoplasty, modifying its form involves mainly the control, distribution and proportion of lower lateral cartilages (LLC). The utilization of sutures on specific areas of LLC, as well as on adjacent soft tissues are particularly useful o rhinoplasty (Daniel, 1993) 3 , therefore is necessary the confection of permanent or semi-permanentsutures to maintain the cartilage on the intended format until the fibrosis, resulting from time and cicatrization, is well processed. All suturesthat remain more than six months will probably be satisfactory, since the scar will have enough support of the LCC, after absorption of its thread. (Gruber, 1997) 4 . This concept of suture is based on otoplasty techniques for the correction of floppy years.
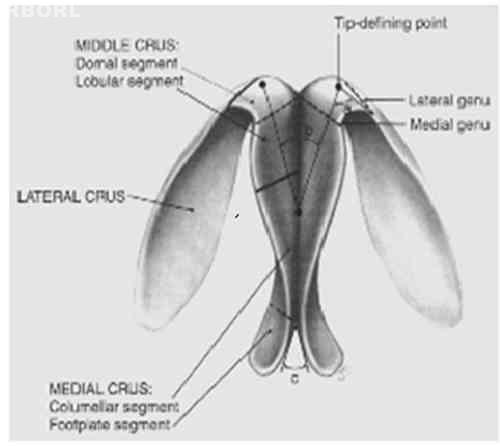
On the other hand these sutures maintain and improve structural support mechanism of the tip, considering that this area is physiologically dynamic since it moves while inhalation and exhalation, and facial expression. It works as a damper during nasal trauma and is an icon of nasal beauty and consequently facial beauty. (TORIUMI; CHECCONE, 2009) 5 O'Neil et al. (1993) 6 have described the domal definition angle and the domal divergence angle. This anatomic concept allows the surgeon to correlate the proportion and form of nasal tip with sutures that modify those angles, offering better definition of the nasal tip.
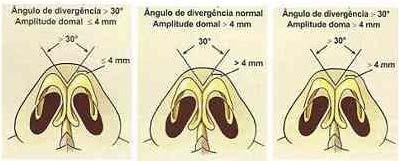
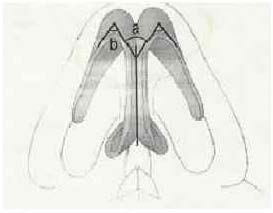
The domal angle is demarcated by lateral crus, and medial or intermedial crus, when there is one. The interdomal divergence angle considered normal is = 30° degreesand thedomalarch<=4 mm. (ROHRICH; ADAMS, 2001) 7 For harmoniousaesthetic lines onthe nasal dorsum, slightly divergent curves must occur, starting on the superciliary archand extending to the nasal tip definition points that correspond tothe domes. A poorly defined nasal tip, such as in bulbous or boxy noses, have an angle wider than 30 degrees. When observed through a basal view it gains a square shape, and its correction includes repositioning of nasal tip definition points, domes angling and modeling of lateral crura aiming at a more triangular form froma basal view.
3. II. Objeticves
a) Assess the efficacy of the lateral intercrural suture using polydioxanone (PDS®) 4.0absorbable thread by the interdomal measure on primary rhinoplasty. b) Systematizeand describe the lateral intercrural suture to improve nasal tip definition on primary rhinoplasty with mild to moderate deformities.
4. III. Literature Review
Detailed knowledgeof the nasal anatomy isthe most important element for the identification of anatomic structures on the transoperative and is directly related to the choice of the surgical technique that will be utilized. The nasal tip has a variable complex structure, with anatomic structures of several shapes, consistency and volumes, intimately connected. In other words, it is composed by structures of different characteristics that function as a whole, and any alteration in one of theme may affect other, resulting on different aestheticfunctional results.
The nasal lobe is an area that includes the nasal tip and is demarcated by a line connectingthe upper edge of the nostrils, the supratip (breakpoint) and the anterior half of the lateral nasal wall. It is divided in tip, supratip and infratip.
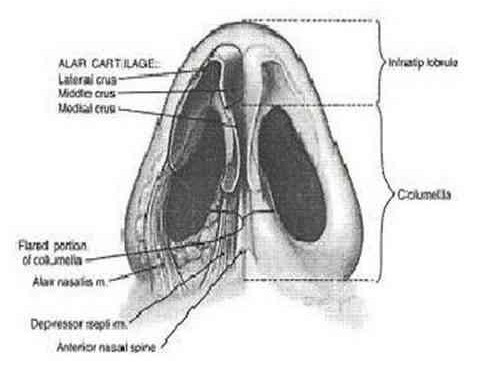
The lower lateral cartilage (LLC) is the main cartilage of the nasal tip and is anatomically divided in: medial, intermedial and lateral crus. From the lateral border of the lateral crus to the pyriform aperture we have the sesamoid or auxiliarycartilages that are bond bya fibrofatty connective tissue(Figures1 e 2) (TARDY, 1992) 8 Volume XIV Issue III Version I The LLC is a complex and variable structure. Traditionally, were only considered the medial and lateral cruraconnected by the domal segment. However Sheen (1997) 9 has introduced the concept of intermedial crus on which the domal segment would be superior. There are still some controversies about considering the intermedial crus as a single structure, but surgically there are few doubts regarding its importance on the nasal lobe configuration.
The medial crus of the LLC, consists on the base and columelar segments. O'Neal e Beil (2010) 10 let clear that that the itermedial crus is more than justa connection between the medial and lateral crura. It has a complex structure and therefore important for the nasal lobe.
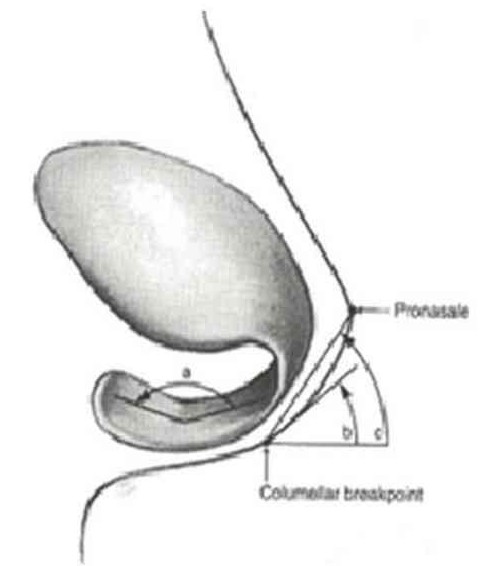
Most of the patients present an angulation in two planes: the cephalic rotation angle the basal divergence angle of the base of the medial crura of the LLC that can be observed on the base incidence (Figure3). These angles affect the shape and the protuberance of the large part of the columela. The amount of soft tissue, as well as the caudal portion of the septum, interfereson the projection of the nasal tip. Anatomically the columelar segment begins on the upper limit of the basal segment and ends on the columelar breakpoint, where the intermedial crus of the LLC starts. Variations on the width of the columelar supratip occur frequently. On the lateral incidence the more convex portion of the columela corresponds to the same columelar breakpoint, corresponding to the junction of this segment with the intermedial crus. The more acute these angulation, more elongatedthe columela will be. (Figure 4) The intermedial crus combine the lobular and domal segment, or simply the dome. Lobular segment has a more variable structure, however exertsless influence over the external appearance since normally it is covered by a great amount of soft tissue. Its width and angle determine the shape and protrusion of the infratip. Domal segment on other handstays more visible because it is covered only by a small portion of soft tissue and by thin skin. Daniel (1992) 11 describes two curvature on the domal region: a)convex, where the domes form a gentle trianglethat is important to the harmony of the nostril apex, where cartilage and skin have direct contact; b)boxy nose characterizing poor definition of the nasal tip c. concave forming a double dome, that is less frequent.
The lateral crus is the larger component of the nasal tip and shapes the upper and anterior portions of the alar wall. Medially it is continuous to the domal segment of the intermedial crus, and laterally to the accessory cartilages on the pyriform process region. Its caudal border offers support and definition to the anterior alar edge. Laterally it curves in a cephalic way becoming wider. Surgically the approximation between the lateral cruraincreases the projection of the nasal tip, and simultaneously gives it a better definition, distinguishing the supratip. Zelnick (1979) 12 has mentionedin his studies that, when the portion adjacent to the domeis concave, this promotes its definition, requiring a minimum modification of the lateral crus. However, it is known that the nasal tip definition is a subjective characteristic for which there is no exact formula to obtain a standard shape.
The scroll region is the junction of the cephalic border and the lateral crus of the LLC. Usually the caudal border of the upper lateral cartilage (ULC) has a slight lateral curve and LLC has a curve towards the bottom resulting on a lifting of the LLC over the upper lateral crus (ULC). The wider the curve of this area, greaterthe bulbosity of the nasal lobe will beresulting on a poor definition. Daniel (1992) 11 affirms that in order to improve the nasal tip definition we should convert the convex lateral crus into concave, and by this way highlighting the dome definition, where the tips, aesthetically adjusted, would give the characteristics of a convex domal segment and a concave lateral crus.
Sheen (1997) 9 has analyzed what would be the ideal nasal tip shape, and described it as two equilateral triangles with a common basemade bythe line that unite the domes. Therefore he named it intercrural distance, the distance between the two domes that coincide on the common base of the triangles.
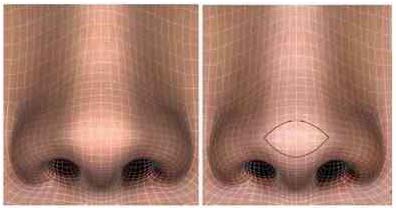
Assessment of asymmetry and concavities using tridimensional figures was performed by Toriumi (2006) 13 , to document precisely the spot of imperfections that are emphasized by shadows that impact over nasal aesthetic contour. From a front view there are criteria for a subtletransition from the lobe to the wing. Thus concludes that tip definition points are horizontally enhanced with tenuous shadows above and beneath it, with two opposite horizontal curvy lines outlining the tip enhancement. The exact configuration of this enhanceement varies among each patient, but on most of the female patients the widthis of 8 mm varying from 6 to 14mm. These values are a little higher on men. (Figure5) On oblique view there is a light shadow on the supratip break that continues along the supra alar notch. When we decide for a cephalic resection of the LLC, we cause the break of the supratip that descend on a frontal view resulting on a better definition of the nasal tip. The contour of the infratip break also becomes important to improve natural aesthetic aspects.
From a base view, the cartilagearch must have a triangular shape free from pinching. The soft tissue triangles must be bland.On a lateral view the nasal tip must be a little above the dorsum with a slight break of the supratip. These shadows are intensified on the soft tissue triangle. What brings us to the conclusion that to be welldefined a nasal tip should have a supratip and an infratip break, being the supratip defined by the junction of the lobe and thenasal dorsum and the infratip by the junction of the lobe with the columela. On the transition of these regions there must be a gaphighlighting the lobe from the tip and nasal dorsum.
Yet it is worth noting that the nasal dorsum aesthetic line, from the eyebrow to the tip, must be soft and its surface free from roughness. (Figure 6) There is a firm transversal connective tissue thatunites the medial and intermedial crura. Previously, it wouldform the interdomal ligament that foundscephalically with vertical and longitudinal fibersof the overlying dermis forming what Pitanguy (1981) 14 describes as dermo cartilaginous ligament of the nose. This ligament would make the superficial connection helping the dynamic balance between the dorsum and the tip of the nose. Therefore its section would result on a cephalic release of the nasal tip, especially in round noses.
Accordingto Tebbetts (2003) 15 , the Strong unification of the medial and intermedial crura by the fibrous tissue would provide a unique functional structure, composed by the lateral crura of the LLC, a sustenance tripod to the nasal tip.
The thickness of skin requires especial attention on a rhinoplasty surgical plan. Usually the skin tends to be thinner o the upper half of the nose and thicker and more adherent on the posterior half. Thicker skin disguises greater defects, but also soothes surgical corrections. Oiliness produced by the sebaceous glands on the nose tip difficult its definition, mainly on ethnics or non-Caucasiannoses. On elderly patients modification of cutaneous characteristics can also be responsible for some alteration typically related to ageing, such as nasal tip drop or lengthened nose.
5. IV. Material and Methods
The present study was approved by the ethics committee under the number CAE 0182.0208.000-11.
6. a) Sample Characterization and Research Site
The present experimental prospective study was performed between March of 2010 and 15 th of November of 2011. In addition to theoretical research, the present study was composed of four basic protocols: ? Selection of target population according to criteria of rhinoplasty indications associated or not with septoplasty. ? Clinical control of the interdomal distance on preoperative, transoperative and post-operative periods, with control and measurement at and interval of 90 to 180days respectively. ? Photographic control and measurement of interdomal distance ? Control, assessment and interpretation of the collected data and statistical results. At this step the electronic protocol SINPE® (Sistema Integrado de Protocolos Eletrônicos) to collect and hierarchize the research steps that corresponded to: anamnesis, physical exams, complementary exams, diagnosis and surgical treatment.
The average interdomal distances were compared during different operativestages from the whole group, genders and skin types of target population utilizing statistical Mann-Whitneytest. The adopted significance level was p<= 0.05.
7. b) Selection of Patients
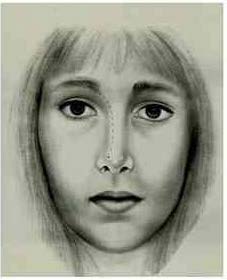
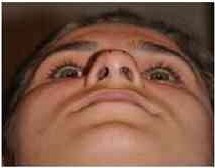
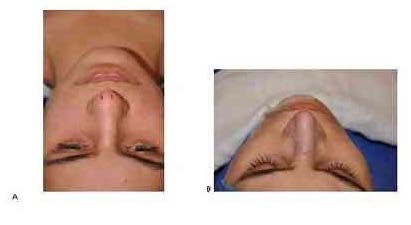
For the development of this study 54 patients with rhinoplasty indication to improve nasal tip definition through lateral intercrura, were selected. Among the main indications for the use of suture technique, the criteria of minor and moderate deformities, meaning, domal divergence angle wider that 30 degrees, normal domal arch smaller or equal to 4mm or moderately wider, larger or equal to 4mm, were the parameters to select the target population. (Figures 7 and 8) For the frontal position register the patient was standing while the surgeon (observer) framed the whole face, including the ears in the image. For the base view picture two images were captured: one with the nasal lobe alignment with the medial corner of the eyelid as parameter, and the other one with the tip of the nasal lobe aligned with the glabella. Left and right oblique vision must be vertically aligned, the nasal lobe tip meeting the pupil of the contralateral eye.
The distance for capturing the photographic images was standardized at 1m between the camera lens and the nasal tip, using a fixed lens with a 100mm zoom in order to avoid distortions. The focus was placed on the nasal tip. Results were assessed by a comparison between photographs from pre and postoperative periods.
Other aesthetic parameters such as: projection and rotation of the nasal tip, nasal base proportion, upper and middle thirds of the nose,were not assessed o this study. The skin of the nose tip was classified as thin, medium and thick according to the surgeon subjective assessment. Data were stored on SINPE© protocol.
8. d) mensuration of the interdomal distance
The methodused to assess the efficacyof these suture technique was the palpation of the lower lateral cartilages, identifying the left and right domes of the nose and measuring the distance between them (IDD)with a beam compass ranging from 0 to 20mm. The exact point of measurement was the midpoint between cephalic and caudal borders of the lower lateral cartilages on the dome level. Those distances were measured on the pre-operative, transoperative and after 3 and 6 months intervals on the post-operative.
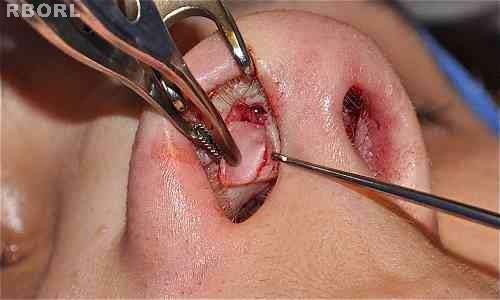
Complications and intercurrences were registered at all post-operative appointment. Data collection was made according to the SINPE© specificprotocol. Post-operative photos were taken under the same conditions described above during routine appointments on thethird and sixth month after the surgery. e) intercrural suture surgical techniques Lateral intercrural suture (LIS) technique is performed after lateral osteotomies. For a better visualization of the lateral crura, the Millard thimble was used with one of the hooks placed to coincide with the dome. Remind that the distance between the hook and the thimble is of 10mm.Anesthetic solution of xylocaine: adrenaline 1:100.000 is infiltrated using an insulin needle in order to achieve hemostasis and hydraulic dissection separating the vestibular ski from the cartilaginous portion of the lateral crus.
With a 15 blade a cutaneous incision is made, from medial to lateral, having the vibrissae caudally line as reference, and like this making a bi-pedicle flap on the medial and lateral vestibular skin using Converse angled scissor. (Figure 9) Using the same blade, these surgical steps are repeated on the contralateral area. Le Garde maneuver was performed La Garde maneuver that consists on the displacement of the soft tissues and connective tissues between lobular skin and lower lateral cartilages. (Figure 11)
Figure 11 : Transoperative. Maneuver of disruptionof the soft tissues and connective tissues between lobular skin and lower lateral cartilages At this moment the exact point, were the lateral intercrural suture will be performed, is marked on the lateral of the dome, using gentian violet. This distance varies according to the spot that, supposedly can offerbetter anatomic results, aiming at diminishing the domal divergence angle and consequently approxi-mates the domes. These distances can vary between 2 and 4mm.
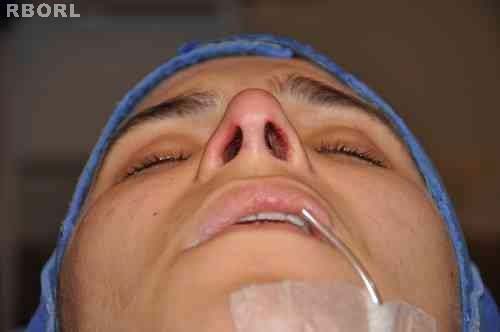
Than a sharp needle with 19mm f PDS 4.0 thread is inserted at cephalo-caudal direction in the left LLC (Figure 12). The knot grip is made progressively and gradually with previous simulation and visual parameter. It is important to mention that the knot must be centralized between the domes (interdomal space) with similar distances so that there are no asymmetries on the nasal lobe after the grip and knot tightening (Figure 16). A minimum of three knots is necessary, and a slight hypercorrection on the approximation of the domes is recommendable. The last step includes the performance of the three septo-columelar sutures also using PDS 4.0. Once the surgery is completed,using the beam compass the new interdomal distance is registered. When compared to the pre-operative distance, this distance should be smaller ( Figures 17, 18, 19).
9. V. Results
Average age was 26.4 years, minimum age of 14 and maximum of 62, and 44% of the sample (26 patients) were between 21 and30 years. Only two patients (3%) were between 51 and 70 years old.
Only one intercurrence (1.9%), was observed, an infection on the nasal tipand there were no major complications. After clinical treatment using antibiotics there were no functional or aesthetic sequels.
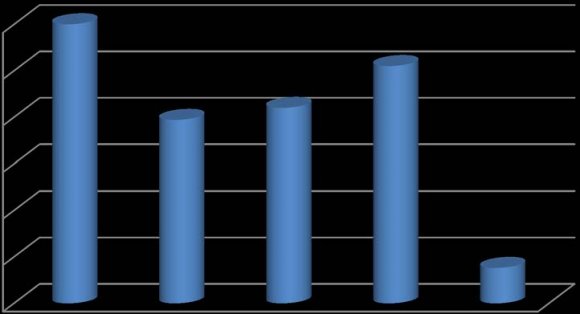
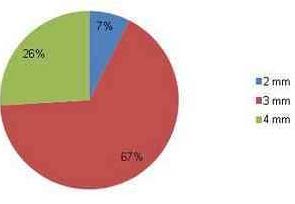
The area were intercrural suture was performed was of 3mm on 66.7% of the cases, at 4mm on 25.9% and in only 7.4% the suture was performed at 2mm lateral to the dome (Graphic1).
Graphic 1 : Suture placement lateral to the dome54 pacientes During pre-operative phase the average interdomal distance was of 12.3 mm varying between 10 to 16 mm, as presented on table 1. On transoperative period the average has decreased to 8.1mm, with variation from 6 to 10mm, and at the three month postoperative there was an increase on this distance reaching an average of 8.8mm (7-11m). After six months the average was 9.1mm (7-11mm). (Table 1) Table1 : Comparison of the Iterdomal Distances(Mm) Among the Several Operative on the Complete Group Note: n -number of patients; min-max -minimum and maximum values; sd-standard deviation;p -statistical significance level
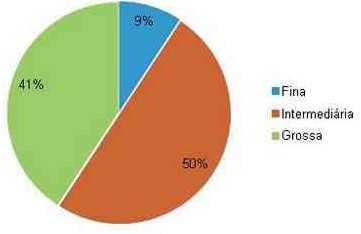
The comparison of the interdomal distance averages between gendersat different operative stages indicated an average of 12.33mm (10-16mm) for women and 12.5mm (12-13mm) for men. At the transoperative the average was of 8.0 mm (6-10mm) and 8.5mm (8-9 mm) respectively for women and men. And at the third month of post-operative period 8.8mm(7-11 mm) for women and 9.0 mm (8-10 mm) for men. The results were, at the sixth month of post-operative, of 9.1mm(7-11 mm) and 9.5 mm (9-10 mm), for women and men respectively. (Table 2) Regarding skin type, twenty seven (50%) had skin of medium thickness. There were twenty two patients with thick skin (41%) and 5 (9%) had thin skin (Graphic 2). The average interdomal distance on patients with thin skin, at the pre-operative, transop-erative and at the sixth month of post-operative were respectively 10.4 mm, 7.8 mm, and 8.8 mm. Therefore there was a slight increase of 1.0 mm when comparing transoperative period to the post-operative sixth month result. 3). Anexample of the comparative resultsof pre and post-operative periods, six months follow-up, of intercrural suture technique with cephalic resection of the LLC, at 3mm lateral to the dome in patients with thin skin, showa better definition of the nasal tip due to the reduction of the interdomal distance (Figures 21 and 24). Regarding interdomal distance at pre-operative phase of 54 patients, most of them (31%) presented a 13 mm distance; in 19% the distance was of 12 mm and in 18%of 11 mm (Graphic 3). Graphics 4 and 5 illustrate the interdomal distance at transoperative and sixth postoperative month respectively. It was noted that 61% of the foresaid measures reached 8mm at this transomperative. At the sixth month 29% stayed at 9 mm; 28% at 8 mm; and 18% at 10 mm. Therefore, most of the patients 85% presented interdomal distance measuring between 8 and 10 mm.
10. Discussion
Surgical treatment of the nasal tipis one of the most importantand challenging aspectsof rhinoplasty. The management of the nasal tip shape involves great part of the anatomy of the lower lateral cartilages, and requires knowledge of aesthetic standards. The aim of this procedure is to correct the nasal tip structure by narrowing it to a harmonic definition of its contours and without interfering on the nasal function.
For many years nose tip surgery utilized aggressive techniques with wide resections or interruption of the alar arches, that may result on sequels, especially those related to sustentation and therefore to secondary deformities. Cartilage sutures on the other hand are a viable alternative to alterations of the nasal tip preserving anatomic structure and improving structural support mechanism. The first suture performed on nose tip was described by Joseph at1930 (Joseph; Raghu, 2006)16. Along the two last decades, ideology among surgeons has changed very quickly, emphasizing sutures as technique for nasal tip remodeling. The control of the tension of the suture can reduce the convexity of the dome and result on concavity of the lateral crura of the LLC.(Corrado; Bloomm; Becker, 2009) 17 Most of those techniques aim at narrowing the tip, applying the suture precisely on a strategic spot approximating the domes ad reducing its divergence angle. Sutures to create a new antihelix on otoplasty described by Mustarde, resemble the technique of sutures in the nasal tip, on which bends and angled alterations can performed (Toriumi, 1995) 18 . These techniques are safer and reversible. Theuse of sutures to improve nasal tip definition is a world tendency at endonasal rhinoplasty (Tebbets, 2003) 19 . Final results of the suture may be influenced, mainly by the intrinsic force of the cartilage, its thickness; by the grip of the suture; limitations imposed by soft tissues, ligaments, amount of subcutaneous tissue and skin density.
The characteristics of the skin are determining factors for lateralintercrura suture efficacy. Patients with thin skin with lack of subcutaneous tissue present more expressive results. On patients with thick skin and excessive subcutaneous tissue the LIS can present low effectiveness if compared to other techniques such as transdomal suture using semi-open rhinoplasty (delivery), or alar lateral spanning (Lo; Rowe-Jones, 1984) 20 . Therefore the choice of the applied technique must bemade according to the skin type and the amount of subcutaneous tissue.
LIS is indicated mostly for noses with thin or medium skin and aim at correcting deformities with an increased divergence of the domal angle, such as bifid tip, boxy tip, or round tip, with poor definition (Patrocinio et al., 2009) 21 . Nasal tips with more complex deformities, such as hyper-projected, asymmetric, congenital or with thick skin, disproportion between cartilage thickness and the amount of subcutaneous tissue, require grafts or division of the dome to adequate definition and narrowing of the nasal tip (Simons, 1987) 22 . Authors agree that the improvement of nasal tip definition should consider the utilization of conservative techniques fordiscrete alterations on patients with thin skin, and use more aggressive techniques for severe deformities. (JANG, 2008) 23 The success of the LIS depends on the previous knowledge of its indications. The surgeon must consider the several options of suture techniques to refine nasal tip since each nose has a variable anatomy and itsharmonization may require distinct procedures. These procedures are not indicated for patients with ethnic noses, such as the Asian, that present certain limitations. In these cases the use ofstrut, medial intercrura and nasal tip graft (GUNTER; FRIEDMAN, 1997). 24 There isn't a better technique for nasal tip definition and refinement, but different efficient methods that must be customized according to the experience of the surgeon that executes them. (NEDV, 2009) 25 It was observed that on the LIS sutures placed on distances more laterally to the dome, up to 4mm, have distinct aesthetic results. The more definition required, more on the lateral the suture mustbe performed. Even not being the object of this study this suture may affect rotation and projection of the nasal tip According to Toriumi (1995) 18 and Tardy (1987) 26 the cartilage suture techniques have been widely applied due to the low index of complications in comparison to cartilaginous arch interruption technique.
11. Volume XIV Issue III Version I
The building with reposition of the domes is efficient with LIS. According to data on the literature, chances of extrusion of the thread PDS® 4.0 are very low (Corrado; Bloomm; Becker, 2009) 17 Most complications reported are inadequate selection of patientor technical errors as asymmetric appliance of the suture. Therefore pre-operative analysis is essential.
In the present study was observed only one case (1.9%) of infection due to the suture, at acceptable levels according to the literature (Pitanguy, 1965) 27 . Furthermore it is well known that PDS® ethicon (polydioxanone) is completely absorbed after approximately 180 days. The absorptionis considered slow but has the possibility of spontaneous resolution or with conservative clinic treatment using antibiotics as verified on this study.
In addition to infection, literature also reports scar retraction, abnormal tip rotation, extrusion of the suture, projection alteration, excessive narrowing of the tip, concavity of the lateral crus, supratip characterization, pinching and valve insufficiency.
Cephalic resection of the LLC is one of the most utilized techniques to reduce the width of lateral crus, and was applied in all cases in order to obtain standardization. Access was transcartilaginous as described by Converse, preserving the cartilaginous arch respecting a minimum of 5mm on the medial portion, next to the dome and 7mm on the lateral following the standard described by Pedroza (2002) 28 on the New Domes technique. Excessive removal may result on inconvenientsuch as loss of support of the lateral crus leading to a pinching of the tip.We consider important the maintenance these measures to preserve the support of the lateral crus, on which a sharp 1.9 cm needle was used. Thegrip of the knot must be gradual and always atthe most natural position of the domes.
Symmetri ccephalic resectionof the LLC associated to LIS must have a strikingand attractiveaspect favoringthe preservationof the triangle creating a more gracious transition on the scroll area and nasal contour, especially from a frontal view. The result would be the harmony of the aesthetic line of the nasal dorsum that must have slightly divergent curves from the supraciliary region to the nasal tip definition spots. (FRIEDMAN; AKCAM; COOK, 2006) 29 . All the patients had compatible symmetry regarding that aspect.
The maneuver described by Le Garde, that consist on the displacement of the soft tissues that connect the lower lateral cartilages to the skin, are of great importance, because they provoke secondary lobular cicatricial reaction, leadingto animprovement of the harmonization of the nasal tip. It also allows the approximation and consequent reduction of the interdomal distance. The knot stays concealed at the medial line, equally distant from the dome, named interdomal space. If this does not occur asymmetry may become evident.
It is observed the necessity of more conservative surgical approaches to correct deformities on the nasal tip. We consider the endonasal access on most cases, especially at the south of Brazil where there is a prevalence of Caucasian noses, therefore requiring less reduction surgeries. Endonasal access through inter-cartilaginous incisions and septo-columelar transfixation is considered less destructive in comparison to semi-open and opened access. However, due to miscegenation a significant part of the population have noses with "mestizo noses", and in these cases there is a reductionof its structure associated tothe increase on the skin thickness and subsequent poor definition of the nasal tip, and the LIS is an option for surgical treatment.
Among the disadvantages of open rhinoplasty is the larger post-operative edema and due to the dissection of the skin there can be scar retraction distortingthe reconstructed osteocartilaginous structure. (Gruber; Weintraub; Pomerantz, 2008) 30 . Indiscriminate fat removal must also be avoided since it is known that it increase the risks of necrosis and skelotonization of the LLC. Although it is not common, transcolumelar unaesthetic scar must be considered, however advantages such as better anatomic visualization and its intercartilaginous relation are prioritized by some surgeons. We preferendonasal rhinoplasty but we have Possibilities of extrusion of the suture thread are reduced when the knot is equidistance from the domes and covered by subcutaneous tissue layer under the skin. Unabsorbable suture with nylon® forms a minimum inflammatory reaction that devolves to a cicatricial fibrosis.After some time there is a small loss of tensional force. Similar reaction also happens with polypropylene (Prolene®) utilized by Pedroza (2002) 28 on its New Domes Technique. Polydioxanone is completely absorbed after approximately 180 days, giving enough time for cicatrization. The inconvenient is that,after approximately 4 weeks, it begins to loose gradually itstensional force that, according to the manufacturer, can be reduced to 50% in this period (ETHICON, INC. Johnson & Johnson Company). Another alternative would be the Polydioxanone (PDS®3.0) considered more efficient regarding tensional force, with a 60% loss in 42 days. In the present study was verified that a slight hypercorrection with interdomal approximation of 1 mm more than the necessary must be performed, considering the structure and thickness of the LLC; the amount of subcutaneous tissue, skin thickness and that the more lateral the dome more tension will be necessary. Poliglicaprone (Monocryl®) would be another option, but, according to the manufacturer, its total absorption is faster, from 91 to 119 days. Thus there is no ideal thread and surgeons must be critical, particularly about absorption and loss of tensional force. Therefore more precise measurements comparing these measures at pre-operative and medium and long term post-operative are required.
Comparative studies with several threads mustbe performed and are fundamental to systematize techniques of sutures on the nasal tipon primaryor revision rhinoplasty. Other parameters such as stabilization degree, and cartilaginous support, symmetry and objectives relative to tip projection must also be analyzed
We prefer to measure the exact spot, lateral to the domes, than place the needle for further grip of the suture. Tebbetts19described at 1994 the lateral intercrura suture placing the needle on the middle third of the lateral crura. Likewise the present study, the author is critical in relation to the knot placement that must be at a centralized and symmetric position. The grip must be controlled to prevent excessiveness tension narrowing overmuch the nasal tip, increasing the concavity of the lateral crura. These sutures progressively force the lateral crura to move medially, thus the domes will be dislocated to a more caudal position with a little alar retraction.
Dependingon the intrinsic forces, this suture may also result on a concavity of the alar edges and therefore requiring alar grafts. Was noticed in this study that when it is necessary to reduce the interdomal distance,, the suture must be performed on the anterior portion of the dome (Gunter,1997). 32 Another peculiarity that we have observed was that for poor defined tips the LIS should be placed on the lateral of the dome, at 4mm for example. Alar or domal arches wider than 4mm or unsupported cartilagescan also benefit from thistechnique, because in these cases there is a lengthen of the medialcrura that leads to alength of the columela. It was concluded that before griping the knot the surgeon must look at the nose from a tridimensionalview, so that when necessary he can change the local on the future.
We have performed this technique using simple suture, however McCollough and English (1985) 33 have reported at 1985 a technique aiming at tip projectionand consequent definition using a single horizontal suture connecting the 4 crura to the morcellized domes. Other technique that deserves to pointed out was published by Tardy and Chemy (1987) 34 and consists on a previously mentioned modification technique that resect interdomal fibrous soft tissue. Gruber et al. (2008) 30 have reported on their study that the horizontal suture approximation must not be inferior to 10 mm approaching the domes preserving the natural bifid aspect. Our study has achieved an interdomal distance of 8.1 mm at the transoperatory evolving to 9. Evaluating the quantity of sutures to be performed single suture is considered efficient, but the necessity of a second or third complementary suture to achieve the desired effect must not be discarded (Guyuron; Behmand e Ramin, 2003) 35 . A parameter would be a tenuousresidual convexity of the lateral crura.
Leach e Athré (2006)36described 77 patients submitted to the technique with 4 sutures: medial intercrural suture, bilateral transdomal suture and another interdomal suture along the cephalic board of the LLC using PDS 5.0®. They have verified that these sutures interfere over 7 variables on the nasal tip: projection, supratip, rotation, form, definition, symmetry and bifid columela. However only open technique was used and follow-up was short, 3 to 8 months.
They also suggest that lateral intercrural sutures must be performed at a distance of at least 5 to 6 mm away from the alar edge in order to avoid pinching, unaesthetic scar, preserving the aesthetic triangle described by Sheen (1997) 9 as well as the natural aspect of thesoft triangle.
According with increased domal divergence angle or wider domal arch, of patients with thin or medium skin.
Our study has similar indications, but on cases where these deformities are more severe, other techniques can be associated, such as intercrural columelar strut and alar board grafts. However patients that required complementary techniques were excluded from the present study.
Cephalic resection was performed in all cases living a minimum 5mm distance from the medial portionof the LLC and 7 mm on its lateral portion. Patients with interdomal distance with a slight bulbosity were excluded from the study because there would be no indication for narrowing or augmentation and definition of the nasal tip.
Subtle asymmetries on the lower lateral cartilages are common and the LIScan be indicated for cases on which higher LLC can be only at one side, unilateral widening of the domal arch and/or when the cephalic portion of the LLC have different width.
LIS technique does not intent to substitute other techniques of nasal tip refinement that are already consecrated, such as the New Domes Technique described by Pedroza (2002) 28 where a lateralization of the domes is proposed in order to obtain an enlargement of the medial crus length, were transdomal and interdomal suture are performed using Vycril® 5.0. In these cases the tip usually requires more structuring, especially on negroids and mestizo noses.
LIS does not substitutes advanced techniques for nasal tip requiring extended shield graft (Rohrich et al., 2002) 37 , alar support graft (Gunter; Friedman, 1997) 32 and alar contour graft (Rohrich et al., 2002) 37 necessary to correct the excessively convex lateral crura or vertically oriented (Rohrich et al., 2002). 37 An advantage that must be taken into account is that this technique can be reversed if the interdomal distance gets exaggeratedor if there is a reaction to the thread.
The study has verified that the profile of the patients submitted to primaryrhinoplasty aiming at a better definition of the tip, indicated a prevalence of young woman. Twenty e four patients (44%) had ages between 21 and 30 years. Fifty patients (94%) were females.
There was a prevalence of rhinoplasty with LIS on patientswith mediumskin thickness (50%), indicating an ethnic miscegenationin our field. Nine percent of the patients had thin skin.
Comparing to the literature patients with thin and medium skin are more indicated for technique of LLC repositioning using sutures (Gruber; Weintraub; Pomerantz, 2008) 30 . We do not believe that this procedure mustnot be recommended for patients with thick skin, however a more critical analysis must be made because intercrural columelar struts, graft on the alar edge, nasal caudal septum extensor, and in some cases a graft are required. According to our statistics 41% of the patients were classified as presenting thick skin type.
There was only one caseof infectionon the nasal tip, a 15 years old patient on the third post-operative month. Conservative treatment with antibiotics was effective with improvement of inflammatory signs and no aesthetic or functional repercussion over the final result.
It was noticed that on 67% of the LIS cases the suture was performed at 3mm lateral to the dome, 26% at 4 mm from the domes and 7% at 2 mm. Thus it is possible to affirm that the sutures are efficientwhen placed between 2 and 4 mm from the dome.
It mustbe observed that when more projection of the nasal tip was necessary, meaning anenlargement of the medial crus of the LLC, the suture must be more fixed more laterally. In this circumstance we must be critical about the knot grip in order to not reduce excessively the interdomal distance, avoiding valvular insufficiency and preserving respiratory function.
About the gradual grip of the LIS, we must also evaluate at the transoperative the possibility of a slight increase if the supratip. There is a relation between this defect and the skin thickness, since the knot is hidden on this interdomal space and can discretely elevate the skin (NEDEV, 200925; GRUBER, 200830). That would lead to an undesired effect, a subtle "polly beak", the augment of the medium nasal third.
Graphic 3 describes the pre-operative interdomal distance in mm. Distances between 10 and 13 mm corresponded to 83% of the cases, being 31% of 13 mm, 19% of 12 mm and 15% of 10mm. Major interdomal distance was of 16mm on two patients (4%) and the smaller was of 10 mm on 7 patients(15%). Our aesthetic and functional analyses indicated that the interdomal distance at the transoperative can vary between 6 and 10 mm depending on skin type and the necessity to reduce interdomal distance in comparison to the aesthetic line of the dorsum.
The majority of the interdomal distance wasbetween 8 mm (61% of the cases). Twenty percent presented a 9 mm distance. The wider interdomal distance was 10 mm (4% of the patients) and the smaller one was of 6mm on 8% of the patients (Graphic 3). Therefore the comparison of measures between preoperative (12.3 mm) and the average of transoperative average interdomal distance (8.1 mm) indicates a significant diminishing of 4.2 mm proving the efficacy of this technique. Analyzing these distances at the third month of the post-operative period, they stay between 7 and 11 mm, an average of 8.8mm, so there is an increase of 0.8 mm in comparison to transoperative period.
At the sixth post-operative month, when a more objective result is observed, the measure of interdomal distance has stabilized onthe same 7 to 11 mm with a small increase of the average to 9.1mm. We believe on the maintenance of the interdomal distance at the sixth month because the average was similar to the previous one. The most important comparison on the evaluation of real efficacy of LIS on reducing interdomal distance would be the transition from the transoperative to the sixth month of post-operative period. Was concludeedthat the average of 8.1 mm (transoperative) reaches9.1 mm (post-operative 6thmonth). Therefore an average increase of 1.0 mm between these distances is acceptable. By means of statistical analysis using Mann & Whitney test comparative values between distances had high significance level p<=0,05. There At this point we suggest a slight hypercorrection on the LIS, around 1.0mm, expecting that as mentioned before, the interdomal distance will increase progressively.
Comparison of differentskin types, regarding its thickness, the interdomal distance on thin skin patients was of 7.8 mm (transoperative) reaching 8.8mm at the 6 th month (post-operative). Thus, a similar result to thegeneral averageincrease of 1.0 mm. Medium thickness skin patients presented a 8.1 mm distance (transoperative) followed by a 9.4 mm distance at the 6thmonth (post-operative), indicating an augment of 1.3 mm, 0.3 mm more than the average. For thick skin patients when comparing the transoperatory distance (8 mm) to post-operative measures (8.8 mm) this augment is of 0.2mm, smaller than the average. (Table3)
12. VII. Conclusion
The result analysis indicates that the reduction of interdomal distance by lateral intercrural suture (LIS) technique using polydioxane thread(PDS®), diminishes the domal divergence angle, approximatesthe domes resulting on a better definition of the nasal tip on primary rhinoplasty, maintaining an efficient support with good reliability, low morbidity andlow complication index. Therefore this can be a complementary technique to the aesthetic harmonization of the nasal dorsum line It was also concluded that there was no significant difference among the obtained results regarding gender and skin types. However it would be prudent to hypercorrect that distance in approximately 1.0mm considering the aesthetic and functional relation on noses with slight or moderate deformities










| Year 2014 |
| Year 2014 |
| Volume XIV Issue III Version I |
| D D D D ) I |
| ( |
| Year 2014 |
| Volume XIV Issue III Version I |
| ( ) |