1. Introduction
he success and predictability of osseointegrated dental implants have forever changed the philosophy and practice of dentistry and, perhaps more than any other specialty, Prosthodontics has changed dramatically. In the late 1950's, Per-Ingvar Branemark, a Swedish professor in anatomy studying blood circulation in bone and marrow, developed through a serendipitous finding in the history of medicine: he predictably achieved an intimate bone-toimplant apposition that offered sufficient strength to cope with load transfer. He called the phenomenon "osseointegration".. Since that time, millions of patients have been treated worldwide using this technique. The implants used sometimes had different geometries and surface characteristics. A key element in the reaction of hard and soft tissues to an implant involves the implant's surface characteristics, that is, the chemical and physical properties. Quest continued for a material with a surface property which enhances bone apposition at the implant surface in an osteoconductive manner. The quest was for a biocompatible if not bioactive surfaces, achieved through additive or subtractive process. Titanium, preferably commercially pure titanium, became the standard for endosseous implants. Actually titanium is a very reactive material that would not become integrated with tissues. However, its instantaneous surface oxidation creates a passivation layer of titanium oxides, which have ceramic-like properties, making it very compatible with tissues.
2. II.
3. Rationale for a Dynamic Implant Surface
Oral implant is an alloplastic material or device that is surgically placed in to the oral tissue beneath the mucosal or periosteal layer or within the bone for functional, therapeutic, or esthetic purposes 1 . More needs to be known about the optimal situation of the connection between an artificial material and the tissues-what type of material that gives the best tissue response and what type of surface is preferred by the bone cells or the cells in the soft tissue. If this is known, the response of the bone or soft tissue can be predicted when the implants are installed into the jaws. There is some information and understanding of the effect of design and toxicology of the implants, surgery techniques, effect of movement of the implant during the healing period and biodegradation. Understanding is lacking, however, of the relationship between the events that occur at the implant surface and the effect the implant material has in the tissue and the biocompatibility of the material 2 .
a) The bone-implant interface Bone tissue is a living organ, which can be described as a natural composite composed of an organic matrix strengthened by an inorganic calcium phosphate (CaP) phase. The extracellular organic matrix (ECM) of bone consists of 90% collagenous proteins and 10% non-collagenous proteins. Regarding the inorganic component, the most abundant mineral phase in human bone is carbonate rich hydroxyapatite (with a carbonate content between 4% and 8%) 3 .
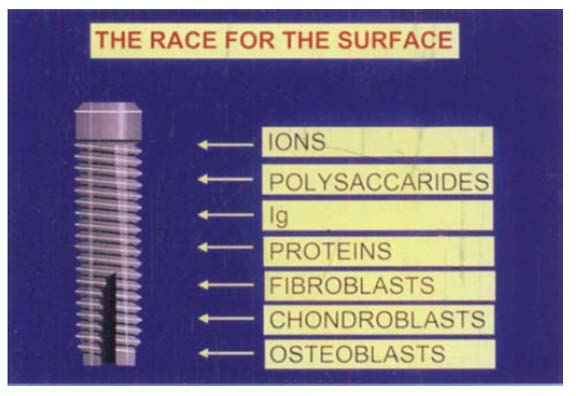
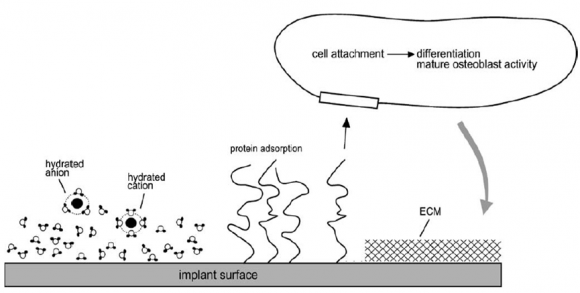
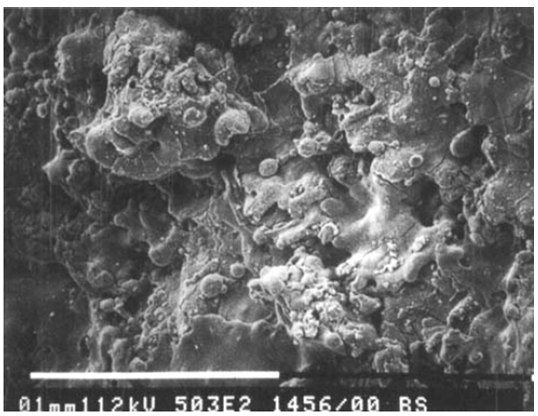
When an implant is installed in a jaw, a series of reactions take place on the implant surface. The implant is exposed to a series of different ions, to polysaccharides, carbohydrates and proteins as well as to such cells as chondroblasts, fibroblasts and osteob-lasts that react with the surface (Figure :1 and 1a) 2,3 . The initial reactions between the tissue constituents and the implant surface govern the further reactions and determine the biological activity of the surface and the further cell responses to the surface. This tissue response depends on the nature of the surface and its chemical properties, which influences the nature of the subsequent composition of the protein film that adsorbs onto the material [4][5][6][7] . this further strongly influences the cell responses on the surfaces.
Figure 1 : After implantation, the biomaterial is exposed to a series of different tissue constituents that react with the surface. The type of reaction that occurs probably influences the further cell reactions and finally the tissuebiomaterial connection. Ig: immunoglobulins Figure 1(a) : Schematic representation of events consecutively taking place at the titanium surface after implantation into living bone tissue. Water binds to the surface, followed by incorporation of hydrated ions, adsorption and desorption of proteins, eventually leading to cell attachment. After differentiation, mature osteoblasts produce the extracellular matrix (ECM) b) Osseo-integration versus Osseo-coalescence
The term osseointegration largely refers to the physical integration or mechanical fixation of an implant in bone. The interlocking provides mechanical resistance to forces such as shear experienced in "pull-out" and "torque-out". With purely physical interaction, however, the interface would not be able to withstand even moderate tensile forces. The term osseocoalescence has been proposed to refer specifically to chemical integration of implants in bone tissue. The term applies to surface reactive materials, such as calcium phosphates and bioactive glasses, which undergo reactions that lead to chemical bonding between bone and biomaterial. With these materials, the tissues effectively coalesce with the implant 8 .
4. III.
5. Physical Properties
Several authors have discussed the dimension of the ideal roughness that would provide increased retention and an improved bone response. The roughness can be considered on different levels: macrostructural, microstructural and ultrastructural, and roughness on these different levels probably has different effects on the living tissues. It has been established in the literature based on several studies that, to gain complete growth of bone into a material's irregularities, these need to be at least 100 µm in size. Growth of bone into cavities or pores of this size will give a mechanical interlocking of the material with bone. This was demonstrated by Bobyn et al. in studying cobaltbased alloys with pore sizes of 50-400 µm 9 , Bone ingrowth was also observed by Clemow et al. when this group studied porous coated Ti&l,V femoral implants with pore sizes ranging from 175 to 235 µm 10 .
6. a) Surface Microstructure
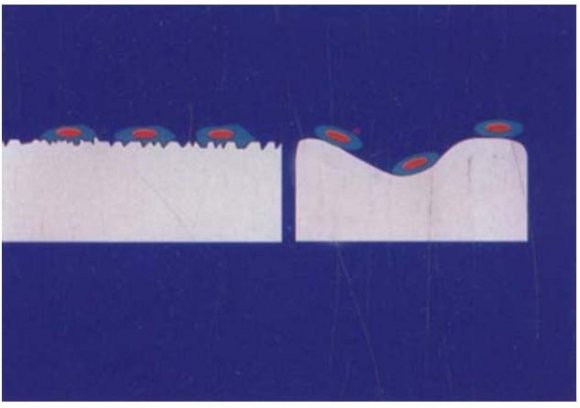
This can vary considerably depending on the surface treatment of the implant. Variation of the surface microstructure has been reported to influence the stress distribution, retention of the implants in bone and cell responses to the implant surface. The implants with rough surfaces have improved bone response, with bone trabeculae growing in a perpendicular direction to the implant surface. An improved retention in bone has also previously been reported after implantation of rough-surfaced implants 2 .
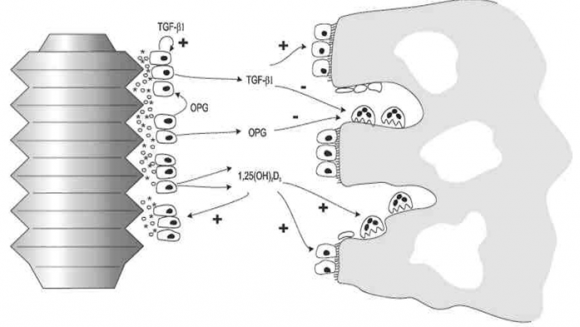
Surface roughness on a smaller scale was, however, found to be important for integration of the bone with the implant surface 11 . Although surface roughness on a micrometer scale gives some retention due to bone in growth, in vitro cell studies indicate that this property of the surface influences the function of the cells, the matrix deposition and the mineralization 12 . Cells seem to be sensitive to microtopography and appear to be able to use the morphology of the material for orientation and migration 13 . The maturation of the cells also affects the response to the surface roughness, which is in agreement with earlier observations that indicated that chondrocytes are affected differently by local factors such as vitamin D and transforming growth factor p depending on the stages of maturation of the cells 14,15 . Microtopography may therefore be one factor that influences the differentiation of mesenchymal cells into fibroblasts, chondrocytes or osteoblasts. Based on these studies, it can be hypothesized that osteogenesis may be favored by vascular in growth, whereas a limited vascular in growth may induce chondrogenesis. Figures: 2 and The ideal surface roughness for bone implants on a micrometer scale probably depends on the distribution of cortical or cancellous bone and on the level of loading to the implants. 2 The rugofile bone cells recognizes the surface prepared by the course particle, as a smooth surface, whereas the 25-pm particles creates a rough surface that is identified by the osteoblasts Osteoblasts respond to microarchitectural features of their substrate. On smooth surfaces (tissue culture plastic, tissue culture glass, and titanium), the cells attach and proliferate but they exhibit relatively low expression of differentiation markers in monolayer cultures, even when confluent. When grown on microrough Ti surfaces with an average roughness of 4-7 ?m, proliferation is reduced but differentiation is enhanced and in some cases,as it is synergistic with the effects of surface microtopography. In addition, cells on microrough Ti substrates form hydroxyapatite in a manner that is more typical of bone than do cells cultured on smooth surfaces. Osteoblasts also respond to growth factors and cytokines in a surface-dependent manner. On rougher surfaces, the effects of regulatory factors like 1?, 25(OH) 2 D 3 or 17?-estradiol are enhanced. When osteoblasts are grown on surfaces with chemistries or micro architectures that reduce cell attachment and proliferation, and enhance differentiation, the cells tend to increase production of factors like TGF ?1 that promote osteogenesis while decreasing osteoclastic activity. Thus, on microrough Ti surface, osteoblasts create a microenvironment conducive to new bone formation 16 . Figure: Although micro-roughness seems to be an important characteristic for tissue response to biomaterials, there are also observations that indicate a biological response to irregularities on the nanometer level. Larsson et al. studied the biological effect of changing the oxide thickness of titanium implants from an electropolished level, to thick oxide layers formed by anodization. By this treatment the surface changes from an amorphous metal surface with a noncrystalline oxide to a polycrystalline metal surface with a crystalline oxide layer 17 .
Analysis of these surfaces at a high resolution level demonstrated that the new surface was heterogeneous with mainly smooth areas of thick oxide but separated with porous regions on a nanometer level. This observation of an increased roughness after anodization of titanium was in line with earlier transmission electron microscopic studies demonstrating increased pore sizes with increased oxide thickness 18 .
Implants with this thick, heterogeneous oxide seemed to have a slightly improved response in bone, particularly in the first weeks after implantation. c) Smooth versus Rough Surfaces Surface quality of an oral implant can be subdivided in to mechanical, topographic, and physicchemical properties 19 . Surface topography is characteristic of the preparation process. Variations in the roughness and porosity can be categorized in function of the surfacing process. The current state of information regarding implant surface topography has provided clinicians with confusing options. Machined implants are not smooth, and not all rough implant surfaces are equivalent. Surfaces often are identified by the method of manufacture and not the resultant surface.
Rough surfaces can be divided into three levels depending on the scale of the features: macro-, microand nano-sized topologies. The macro level is defined for topographical features as being in the range of millimeters to tens of microns 20 . This scale is directly related to implant geometry, with threaded screw and macro porous surface treatments giving surface roughness of more than 10?m. Numerous reports have shown that both the early fixation and long-term mechanical stability of the prosthesis can be improved by a high roughness profile compared to smooth surfaces 21 .
The high roughness resulted in mechanical interlocking between the implant surface and bone on growth. However, a major risk with high surface roughness may be an increase in peri-implantitis as well as an increase in ionic leakage. A moderate roughness of 1-2?m may limit these two parameters 22 . The microtopographic profile of dental implants is defined for surface roughness as being in the range of 1-10?m.
IV.
7. Chemical Properties a) The surface chemistry of the implants
The chemical properties of the biomaterial surface play an important role for the tissue responses elicited by the material. This is at least one main reason why the tissues responds differently to different materials. 2 A material with a surface that is accepted by the tissue seems to exhibit improved integration with bone, either due to passive growth, leading to a tight connection between implants and bone, or by stimulation that probably leads to a bone-implant bonding. This is probably the case with the two main materials used in dental implants, hydroxyapatite and J titanium. 2 The calcified parts of the bone consists of hydroxyapatite (or rather carbonated apatite), and introducing this substance as an implant material often gives favorable responses in the bone. 23 The biological effects of modifying the biomaterial surface have also been elaborated [24][25] . In an attempt to study the effect of the oxide layer of titanium on calcium-phosphate precipitation, titanium-dioxide (TiO2) and powder of oxidized and nonoxidized titanium were introduced into an in vitro nucleation test system 24 . In this system they found that titanium powder enhances calcium phosphate nucleation only after prolonged preincubation in an aqueous buffer, or after autoclaving. These treatments enhance the growth of the oxide layer. This observation indicated that the oxide content, or structure, is required for titanium to act as a nucleation substrate. Even more effective nucleation was observed when pure TiO2 was used as a nucleation substrate. The nucleation capacity and formation of calcium phosphate precipitates is related to the biocompatibility of titanium, and enhanced nucleation capacity may indicate improved biocompatibility. 2 The biological activity of the TiO 2 probably also influences the protein adsorption to titanium. In an in vitro study, serum proteins seemed to adsorb to titanium dioxide by the same mechanisms as to hydroxyapatite through calcium binding 24 . The surface characteristics of TiO2 probably change from an anionic to a cationic state by the adsorption of calcium to the surface. This will subsequently increase its ability to adsorb acidic macromolecules, such as albumin, a property demonstrated for hydroxyapatite [26][27] .
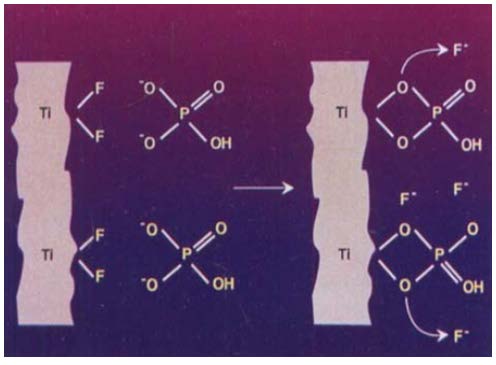
Fluoride ions have documented activity in bone. This element is known to form fluoridated hydroxyapatite or fluorapatite with improved crystallinity and better resistance to dissolution than hydroxyapatite 28 . Fluoride also enhances the incorporation of newly formed collagen into the bone matrix and increases the rate of seeding of apatite crystals as well as increasing trabecular bone density and stimulating osteoprogenitor cells number in vitro 29,30.
8. Diferent Types of Implant Surface Treatments
The desired implant surface can be achieved by addition of material over the surface, removal of material from the surface or modification of the surface material. Some of the examples are: I. Addition of material -Titanium plasma spray (TPS, TiO2); coating with hydroxyapatite (HA).
II. Removal of material -Particle jets and/or acid etching III. Modification of material -The implant surface can be modified without either adding or removing material. (Electron beam, thermal treatment, laser treatment, and ion implantation) a) Addition of Material (Additive Methods)
Chemical substances are successfully added over the surface. Some of the materials used for this purpose include: VI.
9. Additive Methods of Surface Treatment a) Hydroxyapatite coating
Hydroxyapatite is a calcium phosphate ceramic that is an osteophilic, osteoconductive, bioactive coating, which is totally biocompatible and becomes an integral part of living bone tissue. Hydroxyapatites and tricalcium phosphates have an excellent grade of acceptance, and these materials may be more rapidly incorporated in bone than commercially pure titanium. Hydroxyapatite coating over titanium has enjoyed a rapid growth because of its inherent biomaterial properties that some consider an advantage over uncoated surgical titanium. Hydroxyapatite (HA) coating has become popular for load bearing dental implants because it elicits a faster bony adaptation, absence of fibrous tissue seams, firmer implant bone attachment, reduced healing time, increased tolerance of surgical inaccuracies, and inhibition of ion release 31 .
The first clinical use of hydroxyapatite (HA) as a coating on dental implants began in February 1984, with the results showing many benefits over the no coated implants31. Later, many researchers conducted studies and obtained promising results.
Contemporary plasma-sprayed hydroxyapatite (HA) coatings with high crystalline content are much more resistant to in vivo degradation than HA coatings of a decade ago but reportedly exhibit reduced wettability, which could potentially negatively affect tissue adhesion and long-term clinical outcome.
Bone morphogenetic proteins (BMP s) play a crucial role in cell ingrowth and differentiation in a variety of cell types, including osteoblasts 32 . Because of their beneficial effects, BMP s have been used to accelerate healing after implant placement. Apatite is considered a suitable carrier of BMP-2 33 and the incorporation of BMP-2 into the apatite layer of a titanium implant may enhance its osteoinductive properties. i.
10. Methods of HA Coating
Conventional plasma spraying, flame spraying, and chemical techniques have all been investigated as techniques for producing a thinner HA coating on a metal substrate. The bond formed between HA coatings and the metallic substrate by the spraying method, formed primarily through mechanical interlocking, is not strong enough. Additionally, the spraying method is unsatisfactory for applying a thinner, uniform HA coating on implants because of their complicated shapes. On the other hand, electrochemical methods, electrop-0horetic techniques in particular, seem attractive for forming HA coatings on titanium implants with complicated shapes. However, the bond between the coating and the metal substrate is significantly weak. Magnetron sputter coating and Ion Beam sputtering techniques for coating HA on implant surfaces have been tried with varying rates of success. Hydroxyapatite can be coated by plasma spraying. In this technique, powdered crystalline hydroxyapatite is introduced and melted by the hot, high velocity region of a plasma gun and propelled onto the metal implant as a partially melted ceramic. b) Plasma Sprayed Titanium Hahn and Palich (1970) first developed titanium surfaces by plasma spray techniques and reported an enhanced bone ingrowth in those implants. The plasma sprayed titanium surfaces exhibit a porous surface with macro irregularities 34 .
11. i. Macro-irregularities
Macro-irregularities in an implant include macroscopic threads, fenestrations, pores, grooves, steps, threads, or other surface irregularities that are visible. The idea is to create mechanical interlocking between implant and bone at the macro level.
ii. Method of Plasma spraying Powdered Titanium is melted at a temperature of 15,000 degrees and is sprayed on to the surfaces of the implant at a very high velocity of 600 m/sec through argon plasma associated with a nozzle. The diameters of the sprayed particles are around .04 to .05mm thickness. When observed microscopically the coatings show round or irregular pores that are interconnected with each other. The surface of the implants where they condense and fuse together, forming a film about 30 ?m thick. The thickness must reach 40-50 ?m to be uniform. The resulting TPS coating has an average roughness of around 7 ?m, which increases the surface area of the implant. c) Anodic Spark Deposition Anodic spark deposition techniques have been effectively applied to achieve a microporous morphology on metals. Recently, a new electrochemical process has been developed to improve further the mineralization potential, mechanical stability, and corrosion resistance of the ceramic coating obtained with anodic spark deposition. Electrochemically treated titanium showed promising results and was able to introduce substantial improvements in achieving fast and stable osseointegration of implants in osteopenic sheep bone 35 .
12. d) Biologic Coatings
Puleo and Nanci (1999) emphasized the importance of biochemical methods of surface modification as an alternative or adjunct to morphologic approaches. Biochemical methods are aimed at control of the tissueimplant interface by the immobilization and/or delivery of proteins, enzymes, or peptides for the purpose of inducing specific cell and tissue responses. They rely on current understanding of the biology and biochemistry of cellular function and differentiation and on suitable surface modification techniques 36 . e) Bio-molecules i.
Laminins 37 Laminins are major proteins in the basal lamina, a protein network foundation for most cells and organs. They are an important and biologically active part of the basal lamina, influencing cell differentiation, migration, adhesion as well as phenotype and survival.
ii.
Fibronectin 37 Fibronectin is a high-molecular weight (~440 kDa) extracellular matrix glycoprotein that binds to membrane-spanning receptor proteins called integrins.
In addition to integrins, fibronectin also binds extracellular matrix components such as collagen, fibrin and heparan sulfate proteoglycans.
It is involved in cell adhesion, growth, migration and differentiation. Cellular fibronectin is assembled into the extracellular matrix, an insoluble network that separates and supports the organs and tissues of an organism.
iii.
13. Vitronectin
Vitronectin is an abundant glycoprotein found in serum the extracellular matrix and promotes cell adhesion and spreading.
Vitronectin serves to regulate proteolysis initiated by plasminogen activation. Additionally Vitronectin is a component of platelets and is thus involved in hemostasis. Vitronectin contains an RGD sequence which is a binding site for membrane bound integrins, e.g. the Vitronectin receptor, which serve to anchor cells to the extra cellular matrix. iv.
14. RhBMP-2
BMP's are Bone morphogenetic proteins. They are members of -growth and differentiation protein family. They are homodimeric, glycosylated proteins that are highly conserved across species. They are found to be osteoinductive in animals and humans.
They are supposed to promote bone induction by increasing Chemotaxis and increasing the proliferation and differentiation of bone forming cells from undifferentiated mesenchymal cells.
They induce the formation of both trabecular and woven bone. The formed bone remodels based on the demand at the particular site. The delivery of BMPs is aimed at local administration, which is in favor for coating the implant surfaces. v.
15. Bio molecules and Implants
The proportions of these biologic molecules and the presence of other lesser-known components seem to vary with the anatomic location and specific function of the individual basement membrane. Ultra structural data provided by Swope and James (1981) indicate that hemidesmosomes formed on Vitallium Volume XIV Issue IV Version I Year ( ) J implants in monkeys after 2 days and became well established after 3 days 38 .
However, more recently published data dispute these findings, indicating that hemidesmosomal contacts were found only on apatite and polystyrene substrates.
vi.
16. Amino acid sequence RGD
In a goat femur wound chamber model, Bernhardt et al. ( 2005) compared bone-to-implant contact on uncoated titanium implant surfaces with RGD peptide-coated surfaces. After 5 and 12 weeks of healing, no significant effect of RGD coating on the mean bone-to-implant contact percentages was observed 39 . These results contradict the findings of
17. Schliephake et al. (2005b
) compared, in the mandible of dogs, machined titanium implant surfaces (Ti) with RGD-coated implant surfaces. RGD coatings were achieved either with low RGD concentrations (100 m mol/ml) (RGD low') or with high RGD concentrations (1000 m mol/ml) (RGD high). After 1 month of healing, bone-to-implant contact was significantly higher for RGD high compared with Ti. After 3 months of healing, boneto-implant contact was significantly higher for RGD high and for RGD low compared with Ti 40 .
vii.
18. Collagen and collagen mimetic peptides
The in vivo osteoconductive potential of type I collagen, type III collagen and collagen mimetic peptide sequences as coating for titanium implants was investigated in the publications of Rammelt et al. (2004,2006,2007) [39][40][41][42] .
In the proximal tibial metaphysis of rats, Reyes et al. (2007) compared the mechanical anchorage as well as bone-to-implant contact of machined c.p.titanium implant surfaces (Ti)with either bovine type I collagen (Col-I) or glycine-phenyl alanine-hydroxy proline-glycine-glutamate-arginine (GFOGER; a collagen mimetic peptide sequence)-coated implant surfaces. After 4 weeks of healing, the mean pull-out forces were around 35N for GFOGER, 20N for ColI and 35N for Ti. GFOGER was statistically higher compared with ColI or Ti, but the values for Col I were not statistically higher compared with Ti. The authors concluded that both coatings (GFOGER and ColI) enhanced bone repair and implant integration. viii.
19. Collagen composite coating with CaP
In the mandible of dogs, Schliephake et al. ( 2003) compared bone-to-implant contact between titanium alloy implants with a polished surface (Ti), collagen-coated (Col), mineralized (hydroxyapatite) collagen-coated (Col/HA), sequentially hydroxyapatitecollagen-coated (Col/sew HA) and hydroxyapatitecoated titanium surfaces (HA). Animals were sacrificed after 1 and 3 months of healing. No significant differences in the mean bone-to-implant contact between the various implant surfaces were observed in cortical as well as in cancellous bone after 1 and 3 months of implantation 43 . ix.
20. Growth factor coatings
Growth factors are signaling proteins that promote replication, differentiation, protein synthesis and /or migration of appropriate cell types. In case of endosseous titanium implants, an enhanced proliferation and differentiation of undifferentiated mesenchymal cells osteoprogenitor cells and preosteoblasts into osteoblasts may enhance bone healing (Chappard et al.1999) 44 .
Therefore, the rational to coat titanium implants with locally acting growth factors is the assumption that the release of these growth factors might improve the remodeling process at the bone-implant interface, leading to enhanced bone response (De Jonge et al. 2008) 45. x.
21. Bone Morphogenic Proteins
A particular class of growth factors, BMPs, has shown considerable potential to stimulate bone formation both in extra skeletal sites (Yamazaki et al. 1996; Yoshida et al. 1998) While BMP-2 is used more commonly, BMP-4 is also considered as a candidate growth factor that might improve the remodeling process at the bone-implant interface (Stadlinger et xii.
22. Bone-like coatings
A method to self-assemble and mineralize collagen gel and to precoat a bone-like layer of J mineralized collagen immobilized on titanium implant surfaces has been demonstrated. The mineralized layer was found to promote cellular activity, indicating potential for more efficient bone remodeling at the implanttissue interface. This may promote and/or accelerate osseointegration 58 .
23. VII.
Removal of Material (Subtractive Methods)
Implant Surfaces can be roughened by various material removing techniques. Of which the most common methods are:
1. Sandblasting. 2. Acid etching.
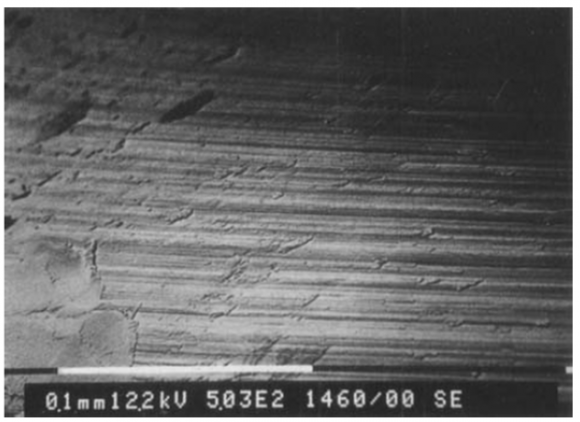
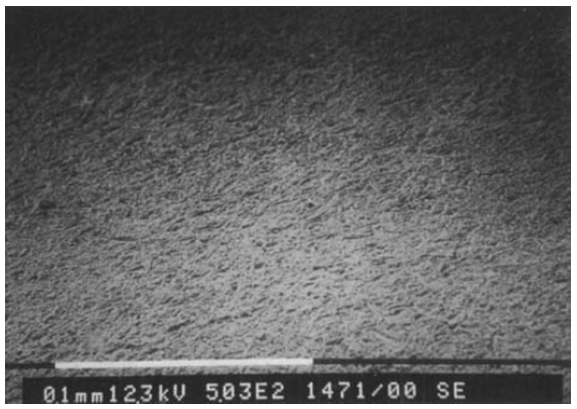
24. Machining. a) Machining
The machining of Cp titanium imparts a surface roughness that is distinct from smooth or polished surfaces. The machining method is an important determinant of the resulting surface. Different surfaces are imparted by machining or subsequent modification. Electro polishing of machined components can further reduce variations measured at the surface, but such surfaces are not well osseointegrated. Creating topographic variation from the mean surface plane can be achieved by abrasion (TiO2 blasting or soluble/resorbable blasting materials [S/RBM]), blasting, blasting and etching (alumina oxide and H2SO4/HCl), anodizing, cold working (dimpling), and different chemical etching methods (H2SO4/HCl)59-61. Bone to implant contact is one of the important factors for osseointegration. Bone to implant contact is higher for osteotite surfaces when compared to machined surfaces 62 .
25. b) Grit Blasting
Another approach for roughening the titanium surface consists in blasting the implants with hard ceramic particles. The ceramic particles are projected through a nozzle at high velocity by means of compressed air. Depending on the size of the ceramic particles, different surface roughnesses can be produced on titanium implants. The blasting material should be chemically stable, biocompatible and should not hamper the osseointegration of the titanium implants. Various ceramic particles have been used, such as alumina, titanium oxide and calcium phosphate particles. Alumina (Al2O3) is frequently used as a blasting material and produces surface roughness varying with the granulometry of the blasting media. However, the blasting material is often embedded into the implant surface and residue remains even after ultrasonic cleaning, acid passivation and sterilization. Alumina is insoluble in acid and is thus hard to remove from the titanium surface. In some cases, these particles have been released into the surrounding tissues and have interfered with the osseointegration of the implants. Moreover, this chemical heterogeneity of the implant surface may decrease the excellent corrosion resistance of titanium in a physiological environment 63 .
26. c) Acid-etching
Etching with strong acids such as HCl, H2SO4, HNO3 and HF is another method for roughening titanium dental implants.
Acid etching produces micro pits on titanium surfaces with sizes ranging from 0.5 to 2nm in diameter. 64 Acid-Immersion of titanium implants for several minutes in a mixture of concentrated HCl and H2SO4 heated above100 ?C (dual acid-etching) is employed to produce a micro rough surface. This type of surface promotes rapid osseointegration while maintaining long-term success over 3 years 65. Enhanced bony anchorage was noted to dual acidetched implants as compared to machined implants 66 .
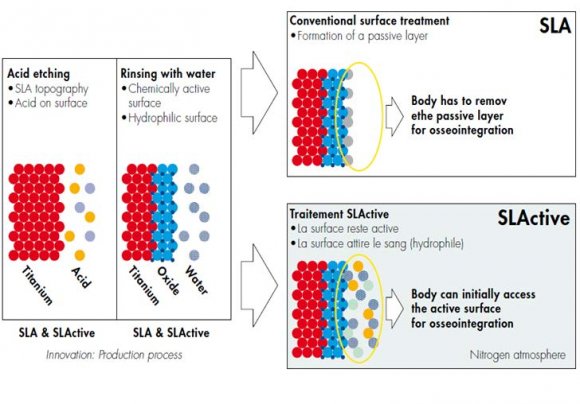
Acid-etched implants showed significantly higher mineral apposition rates compared to acidetched, phosphate coated implants 67 . d) Sand Blasted and Acid etched (SLA) surface Among the various techniques to produce a micro rough titanium surface, the combination of sand blasting and acid etching can be used. These surfaces showed enhanced bone apposition in histomorphometric studies, and higher torque values in biomechanical testing. Based on these experimental studies, clinical studies were initiated to load SLA implants after a reduced healing period of only 6 weeks. The clinical examination up to 3 years demonstrated favorable results, with success rates around 99% 68. e) Chemically Modified SLA Surface: SLActive SLActive is based on the scientifically proven SLAR topography (M. de Wild 2004.). In addition, it has a fundamentally improved surface chemistry. The chemically active, hydrophilic SLActive surface promotes the initial healing reaction, allowing for direct cell interaction at the initial stage of the osseointegration process. Bone formation is immediately initiated resulting in earlier secondary stability and reducing the critical dip. D.Buser et al studied the modified SLA surface produced by rinsing under N2 protection and storing in an isotonic NaCl solution. They demonstrated that the modSLA surface promoted enhanced bone apposition during early stages of bone regeneration 69 .
Michael M. Bornstein et al showed that Dental implants with a mod SLA surface (SLActive) demonstrated statistically significant differences for probing depths and clinical attachment level values compared to the historic control group, with the mod SLA surface implants having overall lower probing depths and clinical attachment level scores 70 . Figure -9. Modification of Material a) Ion Implantation CO ion implantation is a new surface treatment designed to improve implant bone integration by modifying the chemical structure of the implant surface at the atomic level without adding or removing material. This is a high vacuum physical technique (<10-4Pa) in which the surface of a material is bombarded with previously selected and accelerated ions that become integrated or implanted within the outer atomic layers of the surface, thereby modifying the physicochemical properties. A study showed improved percentage BIC values for implants with ion-implanted surfaces in comparison to Diamond like Carbon coating and machined controls. Furthermore, bone integration appeared to be accelerated in the ion implantation group 71 .
27. b) Optimum Roughness
The topography of rough surfaces is characterized by different surface roughness parameters (Ra, Rq, Rt, Rsk, Rku, ?q, or ?q, in 3D or 3D mode). Hansson described that an average surface roughness Ra (filtering 50x50 µm) of about 1.5 µm gave the strongest fixation for a bone-metal interface. If the implants are smoother or rougher than this, the anchorage between bone and implant decreases.
A typical measure of implant surface roughness is the Ra value: the arithmetic mean value of the surface departures from the mean plane. Unfortunately, surfaces may have very different morphologies and still share a common Ra value. It is clear that height descriptors alone do not adequately describe surface roughness. More recently, the average peak spacing (Sa) has been associated with implant behavior. There is enough evidence for the positive relationship between surface roughness and increased bone to implant contact (BIC) 72. c) Optimal Surface Properties Surface properties of implants directly influence bone responses. Thus, irrespective of the surface modification technology used, detailed surface characterization of an implant is important. Based on the bone response in the present study, which was expressed as a function of quantitative changes in the surface oxide properties, the following appear to be the optimum surface properties of oxidized implants:
? The optimal oxide thickness of a porous surface structure appeared to be in the range of 1,000 to 5,000 nm. ? An optimum porosity of open pores is in the range of 19% to 30%, (i.e.) approximately 24%; with a pore size of 2.0 ?m. ? Surface roughness values of 0.7 to 1.0 ?m for Sa, 0.9 to 1.4 ?m for Sq, and 27% to 46% for Sdr seemed to be optimum. ? TiO2 in a crystalline phase seemed to be optimal 73 .
28. d) Controversies
With Respect To Implant Topographies Machined titanium surfaces have been reported to favor fibroblastic growth, migration, and spread, and therefore were considered favorable for formation of peri-implant soft tissue. On the other hand, because of the increased proliferative activity of fibroblasts on machined surfaces, fibrous capsules or connective tissue overgrowth can form, compromising local blood supply and leading to failure of the implant to integrate with the soft tissue. To overcome this problem, rough Rough titanium surfaces have been reported to improve attachment and decrease growth and spread of fibroblasts. However, a diminished growth of fibroblasts on rough titanium surfaces can result in the formation of a thin connective tissue that will not be capable of supporting surrounding tissue structures. In addition, rough implant surfaces have been reported to be especially prone to peri-implant infection and seem also to attract inflammatory cells.
Another suggested titanium surface comprises grooved topography, which has been demonstrated to favor the orientation and alignment of fibroblasts and claimed in several studies to be appropriate for the establishment of an organized connective tissue structure around the implant. However, the exact topographic configurations of grooved titanium surfaces that are appropriate for the in vivo establishment of longterm stable and overall optimal peri-implant soft tissue conditions are still largely unknown.
There is a lack of knowledge about the ideal implant surface characteristics that lead to the establishment of optimal connective tissue and attachment around titanium implants. The acid-etching and blasting methods generally do not change the main compositional surface elements of the titanium, which consist mainly of titanium and oxygen, but rather the surface morphology/topography and consequently surface roughness, two action mechanisms of osseointegration of oxidized implants have been proposed: 1) mechanical interlocking through bone growth in pores and 2) biochemical bonding [74][75] .
29. e) Surface roughness at the nano scale level
The chemistry and roughness of implant surfaces play a major role in the biological events that follow implantation. Nevertheless, surfaces are often developed using an empirical approach with in vitro and in vivo tests. Most of the surfaces currently available have random topography with a wide range of thicknesses, from nanometers to millimeters 76 .
The exact biological role of these features is unknown because of the absence of standardized surfaces with repetitive topography at the nano-sized level (e.g. pits with fixed diameters and depth, lanes with controlled profiles). Such controlled or standardized surfaces might help to understand the interactions between specific proteins and cells. These standardized surfaces might also promote early bone apposition on the implants.
Only a few studies have reported modifications to the roughness as well as the chemistry at the nanometer scale in a reproducible manner. Most of these attempts have used processing methods from the electronic industry such lithography and surface laserpitting.
These nanometer structures may also give the cells positive guidance by means of the selective attachment of osteoblasts to the implant surface. This selective attachment process might result in the improvement of initial healing around dental implants22. f) Re-Osseo integration Persson et al (2001) evaluated reosseointegration of SLA (Sandblasted and acid etched) and turned implants in dogs. They found that reosseointegration was substantial for implants with SLA surfaces but only minimal for exposed smooth (turned) surfaces. Reosseointegration (BIC) at SLA surfaces averaged 84% compared to 22% at turned implant surfaces 77 .
30. IX.
31. Recent Innovations and Future Directions a) Nanotechnology
Nanotechnology is the engineering of functional systems at the molecular scale. Materials reduced to the nanoscale can show different properties compared to what they exhibit on a macro scale, enabling unique applications. For instance, opaque substances become transparent (copper); stable materials turn combustible (aluminum); insoluble materials become soluble (gold). A material such as gold, which is chemically inert at normal scales, can serve as a potent chemical catalyst at nanoscale. Much of the fascination with nanotechnology stems from these quantum and surface phenomena that matter exhibits at the nanoscale.
Nanotechnology involves materials that have a nano-sized topography or are composed of nano-sized materials. These materials have a size range between 1 and 100 nm (109m) Nanotechnology often involves onedimensional concepts (nano-dots and nano wires) or the self-assembly of more complex structures (nanotubes). Materials are also classified according to their form and structure as nanostructures, nanocrystals, nano coatings. b) Methods of Creating Nano-topography Nanotechnology requires novel ways of manipulating matter in the atomic scale. Several approaches are currently prevalent in the experimental application to endosseous implants.
1. One approach involves the physical method of compaction of nano-particles of TiO2 vs. micronlevel particles to yield surfaces with nano scale grain boundaries78. An advantage of this method is that it conserves the chemistry of the surface among different topographies. 2. Second is the process of molecular selfassembly. Self-assembled monolayers (SAMs) are formed by the spontaneous chemisorptions and vertical close-packed positioning of exposed functional end group could be an osteo inductive or cell adhesive molecule. An example of this is the use of cell adhesive peptide domains (RGD domains) appended to SAMs composed of poly ethylene glycol (PEG) and applied to the titanium implant surfaces. 3. A third method is the chemical treatment of different surfaces to expose reactive groups on the material surface and create nano-scale topography. This is popular among current dental implant investigators. NaOH treatment catalyzes the production of titanium nanostructures outward from the titanium surface79. 4. The deposition of nanoparticles on to the titanium surface represents a fourth approach to imparting nanofeatures to a titanium dental implant80 Solgel transformation techniques achieve deposition of nano meter-scale calcium phosphate accretions to the implant surface81-82. Alumina, Titania, zirconia and other materials can also be applied83. Owing to their resultant atomic-scale interactions, the accretions display strong physical interactions. a. In a modified approach, Nishimura and colleagues [2007] demonstrated a directed approach to assembly of CaPO4 nano features on dual acid-etched cp Titanium implant surfaces. The deposition of discrete 20-40nm nanoparticles on an acid-etched titanium surface led to increased mechanical interlocking with bone and the early healing of bone at the endosseous implant surface in a rat model. One of the main concerns related to coating the implant surface is the risk of coating detachment and toxicity of related debris 84 . 5. A fifth approach to creating nano scale topography on Titanium is the use of optical methods (typically lithography) reliant on wave length specific dimensions to achieve the appropriate nano scale modification. These approaches are labor intensive methods that require considerable development prior to clinical translation. The present use of lasers to promote micron-level groove on an implant surface can produce micron-level, not nano scale, modification of the implant surface . Another method of depositing nano scale material on to the implant surface involves ion beam deposition (e.g. hydroxyapatite) 85 .
X.
32. Conclusion
Implant surface characteristics are widely recognized as being of fundamental importance in achieving long-term implant success. As such, extensive research has been performed in order to determine the surface texture necessary to attain an optimal bone-implant biomechanical interlock. Four interrelated properties of an implant surface affect osteogenic activity: chemical composition, surface energy, surface roughness, and surface morphology.Osseointegration and its underlying mechanisms of cell attachment, migration, proliferation, and differentiation are sensitive to one or more of these properties. Methods of enhancing the implant surface include alteration of the microstructure and modification of its physiochemical parameters, including surface free energy and wettability.
The surface qualities are of utmost importance in establishing of a reaction between the implant and the tissues. This concerns the surface structure as well as its chemical and biological properties. Much attention has been focused on the importance of the macrostructure of the implants for establishing retention in the bone. More attention will probably be focused in the future on the biological effects of the surface structure on the microstructural and ultrastructural levels as well as on the surface chemistry of the implants. Progress in these fields based on knowledge of the biological effects may provide implants with improved tissue response and clinical performance in the future.