1. Introduction
ental disorders exert a high toll, accounting for 13% of the total global burden of disease. In Africa, neuropsychiatric disorders accounted for about 18% of years lived with Disability (YLD) in 2000. 1 The growing recognition that long term disability is experienced by a large proportion of persons with serious and persistent mental disorders has spurred the development of the field of psychiatric rehabilitation. 2 Beyond persisting symptoms, social maladjustment in family and vocational roles interfere with the quality of life of an exceeding high number of those with psychiatric disorders. 3 Psychiatric rehabilitation is a whole systems approach to recovery from mental illness that maximizes an individual's quality of life and social inclusion by encouraging their skills, promoting independence and autonomy in order to give them hope for the future and leads to successful community living through appropriate support. 4 The unmet needs of the mentally disabled have pointed the way towards longer-term and more comprehensive in-patient rehabilitation services to help disabled individual to develop the emotional, social and intellectual skills needed to live, learn and work in the community with the least amount of professional support. 5 Discharge from in-patient rehabilitation is a measure of good outcome because it marks an important stage in the individual's recovery. The person would have gained the skills needed for daily living, self medicating, engagement with community support to gain help and sense of identity. 6 Studies of schizophrenics and related psychotic disorders have found only limited evidence that socio-demographic, illness and treatment variables predict outcome. 7,8,9,10,11 In a study, serious self harm, suicide attempt, high dose antipsychotics and antipsychotic polypharmacy predicted non-discharge from rehabilitation in-services. 12 In psychiatric practice, some mentally ill patients spend their life in continuous hospitalization due to severe mental illness, substance dependence, homelessness and abandonment by the patient' relatives. 13,14 In developing countries like Nigeria, the issue of long-stay is intertwined with the history of orthodox psychiatric care. In the early 20 th century, asylums were established in selected cities in the country by the colonial masters. These were to serve as places of M confinement for psychiatric infirm. 15,16 when these asylums were converted to full-fledged psychiatric hospitals, most of the patients had remained in these facilities. Other sources of long stay patient is the vagrant psychotic patients and patients abandoned by their relatives. 17,18,19 In view of the peculiar mental health situation in Nigeria, there have been strong recommendations for the establishment of rehabilitation centres to cater for this category of long-stay patients. 20 The Neuropsychiatric hospital Aro, the foremost psychiatric hospital in Nigeria formally established Rehabilitation unit in 2002 and a transitional half-way home (Hope Villa) in 2009 for the effective rehabilitation and community re-integration of patients.
Since the service provision over a decade ago, no study had been undertaken on the outcome of the service. Knowledge of the factors that are associated with outcome can be used to guide treatment for individual patients. It can also be used at a service level to optimize the structure of services to meet the needs of the patient population.
This current study was therefore undertaken to evaluate the outcomes of care among patients admitted to the rehabilitation unit of Neuropsychiatric Hospital, Aro, Abeokuta, Nigeria.
2. II.
3. Methods
Site: The study centre is Neuropsychiatric Hospital, Aro, Abeokuta, Ogun State, Nigeria. The population of Ogun State is 3.7 million and Abeokuta, the capital city has a population of 0.45 million (2006 National Census).
The Neuropsychiatric Hospital, Aro, started at the Lantoro annex which was a colonial local government prison until 13 th April, 1944 when it was transformed into an asylum for the care of mentally ill soldiers repatriated from the Second World War. This asylum was converted to Neuropsychiatric Hospital (526 bed-space) Aro in 1954. Patients were admitted to the rehabilitation unit based on fulfillment of placement criteria. The rehabilitation unit utilizes a multi-disciplinary team approach to administer psycho-pharmacological, psychosocial, vocational and other structured interventions to patients in the unit. Patients had supervised vocational engagements both within and outside the hospital settings.
Design: This was a descriptive retrospective review of all patients admitted to the rehabilitation unit from inception, September, 2002 till August, 2013 (11 years period).
4. a) Sample Size and Sampling Technique
With in the eleven (11) years period, there were sixty-two (62) admissions. However, case records of six (6) patients could not be traced, consequently a total of fifty-six (56) case records were analyzed. Data Collection: Data was collected using a semistructured proforma containing the following sections: Socio-demographic variables, clinical diagnoses, physical co-morbidity, Rehabilitation activities and outcomes.
The psychiatric diagnoses were made according to ICD 10 diagnostic criteria Activities of Daily Living (ADL) was rated good for patients who could take care of their personal hygiene without prompting; take care of their immediate environment; could prepare or vend for their meals without assistance and could take medications willingly without supervision.
Data Analysis: Data entering, cleaning and analysis was done using the statistical package for social sciences (SPSS) Version 17. Frequency tables and cross tabulations of relevant socio-demographic, clinical, rehabilitation and outcome variables were drawn up.
For survival analysis, the desired endpoint is achieving discharge from the rehabilitation unit, which means that this category achieved mental stability, completed rehabilitation and were re-integrated back into the community.
Survival data analysis was done using Kaplan-Meier method for censored data. This involved coding the outcome variables into 1 -discharge, which is the desired event and 0 -other outcomes which are the censored observations. The factors influencing discharge were evaluated using Cox' Proportional Hazard Regression. The factors in the model were socio-demographic variables, clinical diagnoses and rehabilitation variables.
Chi-square test was used to assess association between categorical variables and Independent student -t-test to compare the difference in the means of quantitative variables. P -values of significance was set at P ? 0.05.
5. b) Ethics
Confidentiality of data was assured and approval for the study was obtained from the Ethical Committee of Neuropsychiatric Hospital, Aro.
6. III.
7. Results
Of the 56 patients, 36 (64.3%) were males. The mean (SD) age of the patients was 54.6 (14.4) years. The socio-demographic characteristics of the patients shown in table I revealed that they were mostly Yoruba (73.2%), Single (67.9%), previously unemployed (73.2%), and that 36(64.3%) of the patients had primary school education and below. Social and family support was poor in 41(73.2%) of the patient while activities of daily living was also reportedly poor in 25 (44.6%) of the patients. Vocational engagements was reported in 35 (62.5%) of the patients.
8. Volume XIV Issue III Version I
9. A
Comparing patients who achieved discharge with the non-discharged group, the discharged group was found to be statistically more educated (x 2 = 21.888, P = 0.001), employed (x 2 = 36.842; P = 0.001) Younger (x 2 = 15.079; P = 0.001), married (x 2 = 9.212; P = 0.027); had good family support (x 2 = 41.837; P = 0.001), had good activities of daily living (x 2 = 22.347; P = 0.001), and engaged in vocational activities (x 2 = 9.184; P = 0.002) while the difference in gender, tribe, vagrant status (homeless) did not attain statistical significance.
The distribution of psychiatric diagnoses and co-morbid medical conditions among patients as shown in table II revealed that schizophrenia was the commonest (85.7%) diagnosis followed by bipolar affective disorder (8.9%). Among the physical co-morbid conditions, hypertension(23.2%) and epilepsy (12.5%) were the commonest. There was no significant difference in clinical diagnoses and medication used between the discharged and non-discharged group of patients. (Table III)
The distribution of vocational engagement among patients as shown in table IV revealed that barbing (8.9%), shoemaking (8.9%) and fashion designing (8.9%) were most represented and 15 (26.8%) patients were involved in paid sheltered work in the hospital.
Outcome measures as shown in table V revealed that 15 (26.8%) patients completed rehabilitation programme and were consequently discharged into the community. Improvement was reported in 43 (76.8%) patients and mortality was recorded in 12.5% of the cases while follow up care was good in 83.9% of the cases. The median duration of stay in the rehabilitation unit was 41.3 months with the discharged group staying lesser (10.1months) while 43.9% of the patients were abandoned in the unit.
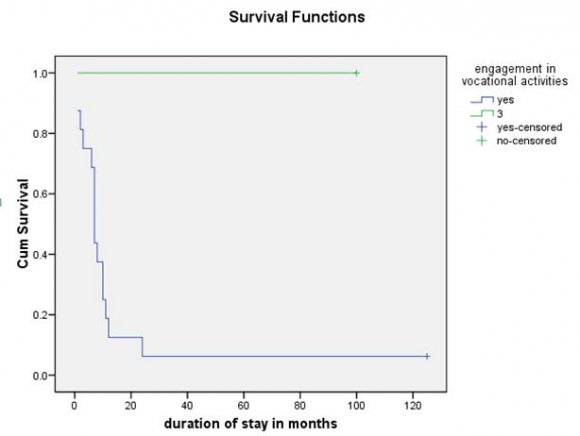
A survival function curve (complementary cumulative function) on vocational engagement and time to discharge from rehabilitation unit is illustrated in Figure 1. The cumulative probability of discharge was higher for patients with vocational engagements at all times.
The factors identified by Cox' proportional hazard regression analysis that significantly influenced time to discharge (increase or decrease) included: low education (HR 0.030, 95% CI, 0.002 -0.287), unemployment (HR 0.409, 95% CI, 0.231-0.736), good social and family support (HR 3.352, 95% C.I, 0.897-12.553), Poor Activities of daily living (HR 0.02, 95% C.I, 0.001-0.290) and being lesser than 40 years old (HR 2.631, 95% C.I, 0.675-10.261), (Table V1).
IV.
10. Discussion
In our study, most of the patient were males, a finding that mirrors those of Joanna et al, but the patients in this sample were much older. 12 Sociodemographic variable predicting discharge were high education, previous employment, younger age, being married, having good social and family support, good activities of daily living and engagement in vocational activities. These findings were in variance to some studies 7,8,9 that found only limited evidence that sociodemographic variables predict outcome. The nondischarged group had inferior socio-demographic profile which could be a reflection of the severity of illness that interfered with normal role performance.
The commonest diagnosis was Schizophrenia. This was similar to the findings amongst patients admitted to the rehabilitation service at the Royal College, Edinburgh hospital. 12 At anytime, about 1% of people with severe and enduring mental illness such as schizophrenia require in-patient psychiatric rehabilitation. Schizophrenia associated with major cognitive deficits independent of age of diagnosis may interfere with both education and employment. 19 The findings of the highest psychiatric co-morbidity with cardiovascular and neurological diseases gave credence to the previous studies that showed that these conditions were common in Nigeria . 21,22 Medical comorbidity in psychiatric patients have been shown to increase the number of hospital admissions and the length of hospital stay with consequent increase in the overall cost of treatment. 23 A high percentage of the patients were engaged in vocational activities. Engagement in vocational activities was predictive of discharge from Rehabilitation unit. Vocational engagement promote gains in related areas such as self-esteem and quality of life as work and employment are a step away from dependency and a step to integration in to society.
Despite the fact that many persons with serious mental disorders want to work, estimated rates of competitive employment among those with these conditions range from 10% to 20% hence most of the patients were placed on appropriate artisan skill training/re-training. 24 The hospital provided support to the patients by placing some of them on paid sheltered employment.
The discharged group of patients stayed lesser in the rehabilitation unit. The factors found to significantly prolong duration of stay in the rehabilitation unit were unemployment, low education, poor social support, poor activities of daily living and older age. These poor socio-demographic factors could be a reflection of the severity of mental illness that impact negatively on the functional domains of the sufferers. 19 V.
11. Limitations
All retrospective studies have certain limitations. Some patients' case records were missing. At the time of admission, there was no baseline rating of illness However, this effect was minimized as the two groups had similar clinical diagnoses. For some of the patients, their ages may not be exact. Although age is a potential variable determining the clinical profile and outcome of treatment, we did not match for this variable in the design stage. We however, evaluated the effect of age and other potential confounding variables in the multivariate Cox proportional hazard regression analysis.
12. VI.
13. Conclusion
In a sample of rehabilitation in-service patients, we conclude that good socio-demographic profiles and engagement in vocational activities were significantly associated with achieving discharge during the eleven year period we studied. In Nigeria and other developing countries, there is need for the recognition of the role of rehabilitation in addressing the adverse consequences of mental disability to the individual, community and the nation. Future research on the dynamics and econometrics of this rehabilitation psychiatry service is highly indicated.
14. VII.
15. Oshuntokun
| 24. Cook JA, Leff HS, Blyler CR. Results of a multisite | ||||||
| Prevalence of epilepsy in Nigeria Africans; a | randomized trial of supported employment | |||||
| community study. Epilepsia, 1987; 28: 272-279. 23. Lyketsos CG. Medical co-morbidity in Psychiatric inpatients: relation to clinical outcomes and hospital | interventions for individuals with severe mental illness. Arch Gen Psychiatry 2005; 62: 505-512. | |||||
| length of stay. Psychosomatics 2002; 43: 24-30. | ||||||
| Variable | Rehabilitation Status of Patients | Total | Test Statistics | P -Value | ||
| DISCHARGED | NON-DISCHARGED | N = 56 (%) | (Chi-Square) | |||
| N = 15 (%) | N = 41 (%) | |||||
| Gender Male Female Age 20 -39 | 11 ( 73.3) 4 (26.7) 12 (80.0) | 25 ( 61.0) 16(39.0) 4 (9.8) | 36( 64.3) 20 (35.7) 16 (28.6) | 0.810 | 0.368 | Year 2014 |
| 40 -59 | 3 (20.0) | 18 (43.9) | 21 (37.5) | 15.079 | 0.001 | |
| Over 60 | - | 19 (46.3) | 19 (33.9) | |||
| Mean (SD) Tribe Yoruba Ibo Others Marital Status Single Married Divorced Widowed Education No Formal Primary | 10 (66.7) 4 (26.7) 1 (6.7) 8 (53.3) 5 (33.3) 2 (13.3) -3 (20.0) 1 (6.7) | 31 (75.6) 8 (19.5) 2 (4.9) 30 (73.1) 2 (4.9) 6 (14.6) 2 (4.9) 21 (51.2) 11 (26.8) | 54.6(14.4) 41 (73.2) 12 (21.4) 3 (5.4) 38 (67.9) 7 (12.5) 8 (14.3) 2 (3.6) 24 (42.9) 12 (21.4) | 1.760 9.212 | 0.624 0.027 | Volume XIV Issue III Version I |
| Secondary Tertiary | 1 (0.7) 10 (66.7) | 7 (14.6) 3 (7.3) | 7 (12.5) 13 (23.2) | 21.882 | 0.001 | D D D D ) |
| Previous | ( | |||||
| Employment | ||||||
| Yes | 9 (60.0) | 6 (14.6) | 15 (26.8) | 36.842 | 0.001 | |
| No | 6 (40.0) | 35 (85.4) | 41 (73.2) | |||
| Patients' Status | ||||||
| Vagrant | ||||||
| Non-Vagrant | 3 (20.0) | 8(19.5) | 11 (19.7) | 2.060 | 0.357 | |
| 12 (80.0) | 33 (80.5) | 45 (80.4) | ||||
| Social and | ||||||
| Family Support | ||||||
| Poor | ||||||
| Good | 5 (33.3) | 36 (87.8) | 41 (73.2) | 41.837 | 0.01 | |
| 10 (66.7) | 5 (12.2) | 15 (26.8) | ||||
| Activities of | ||||||
| Daily living | ||||||
| Poor | - | 25 (61.0) | 25 (44.6) | 22.347 | 0.001 | |
| Good | 15 (100.0) | 16 (39.0) | 31 (55.4) | |||
| Vocational | ||||||
| Engagement | ||||||
| Yes | 15 (100.) | 20 (48.8) | 35 (62.5) | 9. 184 | 0.002 | |
| No | - | 21 (51.2) | 21 (37.5) | |||
| Variable | Frequency | Percentage (%) |
| Psychiatric Diagnosis | ||
| Schizophrenia | 48 | 85.7 |
| Bipolar affective disorders | 5 | 8.9 |
| Alcohol/Substance use disorder | 3 | 5.4 |
| Co-morbid Medical Conditions | ||
| Hypertension | ||
| Epilepsy | ||
| Arthritis | 13 | 23.2 |
| Infections | 7 | 12.5 |
| Cataract/Sight Problem | 5 | 8.9 |
| Diabetes mellitus | 4 | 7.1 |
| 3 | 5.4 | |
| 2 | 3.6 |
| Variable | ||||
| DISCHARGED | NON-DISCHARGED | Total | P -Value | |
| N = 15 (%) | N = 41 (%) | N = 56 (%) | ||
| Psychiatric Diagnosis | ||||
| Schizophrenia | 13 (86.7) | 35 (85.4) | 48 (85.7) | 0.491 |
| Bipolar affective disorder | 1 (6.7) | 4 (9.8) | 5 (9.8) | 0.226 |
| Co-morbid medical condition | ||||
| Hypertension | ||||
| Epilepsy | 3 (20.0) | 10 (24.4) | 10 (24.4) | 0.523 |
| 2 (13.3) | 5 (12.2) | 5 (12.2) | 0.667 | |
| Medication Use | ||||
| Conventional antipsychotics | 12(80.0) | 32 (78.0) | 32 (78.0) | 0.867 |
| Depot antipsychotics | 4 (26.7) | 11 (26.9) | 11 (26.9) | 0.988 |
| Atypical antipsychotics | 1 (6.7) | 3 (7.3) | 3 (7.3) | 0.703 |
| Mood Stabilizer | 1 (6.7) | 4 (9.8) | 4 (9.8) | 0.226 |
| Antidepressants | 1 (6.7) | 2 (4.9) | 2 (4.9) | 0.448 |
| Anti-cholinergic | 6(40.0) | 18 (43.9) | 18 (43.9) | 0.243 |
| Report of Non-adherence | 1 (6.7) | 5 (12.2) | 5 (12.2) | 0.068 |
| Year 2014 | ||
| ( ) | ||
| Variable | Frequency | Percentage (%) |
| Barbing | 5 | 8.9 |
| Shoe making | 5 | 8.9 |
| Fashion designing | 5 | 8.9 |
| Hair dressing | 4 | 7.1 |
| Food and Catering | 3 | 5.4 |
| Retailing/Business | 3 | 5.4 |
| Vulcanizing | 2 | 3.6 |
| Computer programme | 2 | 3.6 |
| Paid sheltered work | 15 | 26.8 |
| Variable | Frequency | Percentage |
| Rehabilitation Status | ||
| Completed & Discharged | 15 | 26.8 |
| Not completed | 41 | 73.2 |
| Abandoned in the Unit | 24 | 42.9 |
| Improvement Status | ||
| Improved | 43 | 76.8 |
| Worsened | 10 | 17.9 |
| Died | 7 | 12.5 |
| Follow Up Care | ||
| Good | 47 | 83.7 |
| Poor | 4 | 7.2 |
| Absconded/Lost to follow up | 5 | 8.9 |
| Median Duration of Stay: 41.3 Months | ||
| Survival Functions | ||
| Variables | Hazard Ratio (HR) | 95% Confidence Interval (CI) |
| Low education | 0.030 | 0.002 -0.287 |
| Unemployment | 0.046 | 0.0231 -0.736 |
| Good Social Support | 3.352 | 0.897 -12.553 |
| Poor Activities of daily living | 0.02 | 0.001 -0.290 |
| Age < 40 years | 2.631 | 0.675 -10.261 |