1. Introduction
arcinoid tumors are a group of neuroendocrine tumors (NET), that are so named because of their ability to secrete bioactive hormones. These tumors can be found along the whole length of gastrointestinal tract (GIT) from the foregut, midgut to the hindgut (1) .
Pre sacral/sacrococcygeal space is a potential space, that contains multiple embryological remnants and is a site for development of various types of tumors. Chordomas are the commonest among them (2) . Carcinoid tumors are rare at this site and are often silent with no associated carcinoid syndrome even if the tumor has metastatized (1,2) . These tumors may arise within tailgut cysts and teratomas suggesting the congenital nature of these tumors and the fact that they may have their origin from the residual neuroendocrine cells within hindgut remnants (2,3) .
Herein, we report a case of 30 year female who presented with vague abdominal and back pain for one year with intermittent constipation. Biopsy was performed which showed features of carcinoid tumor.
2. II.
3. Case history
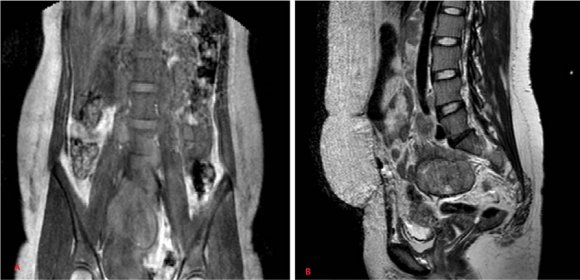
A 30 year-old female was admitted to the hospital, who presented with complaints of vague abdominal and back pain for one year along with constipation on and off. Magnetic resonance imaging (MRI) showed a well defined lobulated soft tissue mass 8.4x7.0x5.4 cm, involving the pelvis with both cystic and solid components. The mass was abutting the sacrum and reaching up to the aortic bifurcation. Rectum and urinary bladder were normal. No lymphadenopathy was observed (Fig 1).
4. Discussion
NET s are commonly found in the GIT and are referred to as gastroenteropancreatic (GEP) NETs (1,4) . These are most often seen in the small intestine, rectum and appendix in that order. These tumors are rarely found in the presacral region and when present are usually associated with tail gut cysts (TGC) (1,5,6) .
TGCs, also known as retrorectal cystic hamartomas are remnants of embryonic primitive hindgut and present as multiloculated cysts in presacrococcygeal space (1,2,3,7). Persistence of this embryological remnant results in the development of TGC (3) . These cysts can undergo malignant transformation to adenocarcinomas, carcinoid tumors, squamous cell carcinoma and sarcomas (3,7,8,9,10,11,12) . These tumors usually show female preponderance, which suggests possible hormonal influence in the pathogenesis (2,3) . Presacral carcinoid tumors usually are asymptomatic and produce symptoms only related to mass effect i.e. pelvic pain, rectal fullness and constipation. Other potential manifestations include infection, fistula formation, bleeding and malignant transformation. Typical symptoms associated with carcinoid tumors i.e. flushing, sweating, hypertension, watery diarrhea are not seen in these tumors. This behavior simulates the carcinoid tumors arising in colon and rectum that also tend to be silent (1,2,3) . The patient in this reported case was a 30 year female who presented only with vague abdominal pain and constipation. CT scan/MRI are useful to identify the primary tumor located at the presacral region and to plan preoperatively in order to delineate the pelvic structures which are in close proximity to the tumor (1,2,13) carcinoids are histologically similar to those arising in any other location regardless of the clinical features that the patient presented with (1,3) . Immunohistochemically, these tumors express cytokeratin (CK) and one or more of the neuroendocrine markers (chromogranin, synaptophysin, neuron specific enolase) (3) . In this case too, histopathology showed typical carcinoid morphology and IHC revealed positivity for CK7 and chromogranin.
Similar to all GIT carcinoids, presacral carcinoids can also metastatize to regional lymph nodes, liver, lungs and bones with risk increasing with the size, nodal status and histological growth pattern (1,14.15) .
The prognosis of these tumors depend on tumor histology, size of the tumor, metastasis and performance of complete tumor resection (2,3) .
IV.
5. Conclusion
Carcinoid tumors in presacral region are rare and do not differ clinically and histologically from those arising in colon and rectum. However, these are less aggressive and more localized. These tumors should be included in the differential diagnosis of presacral mass and close follow up should be maintained for early diagnosis and management of recurrence or metastasis.