1. Introduction
idney diseases manifest in many ways. A patient may be asymptomatic or may be suffering with a life threatening emergency. Apart from the clinical history, ancillary investigations, including urine examination and radiological investigations; renal biopsy is considered gold standard in reaching a diagnosis in many conditions especially in cases of acute renal failure (ARF). Renal biopsy is also the most definitive method of differentiating acute from chronic kidney disease and various renal/tubule-interstitial disorders. The underlying cause of most glomerular diseases remains an enigma. Infectious agents, autoimmunity, drugs, inherited disorders and environmental agents have been implicated as the cause of certain glomerular diseases. 1 The present study was undertaken over a period of three years in a single tertiary care center in the northern part of India so as to take a glimpse of the pattern of disease in an area which is highly resource challenged. A comparison was also drawn with areas in and around Indian subcontinent. A major part of the present study was to understand and analyze clinical symptoms and findings with laboratory investigations and final histopathological diagnosis (clinicopathological correlation). The biopsies were also tabulated according to auto-immune serological panel as well.
2. II.
3. Materials and Methods
The present prospective study comprised of 127 patients who underwent percutaneous renal biopsies over a period of three years (2005-2007) pertaining to renal parenchymal disease. The study was
The present prospective study comprised of 127 patients who underwent per-cutaneous renal biopsies over a period of three years. Before undertaking renal biopsies the clinical findings along with biochemical and urinary investigations were done.
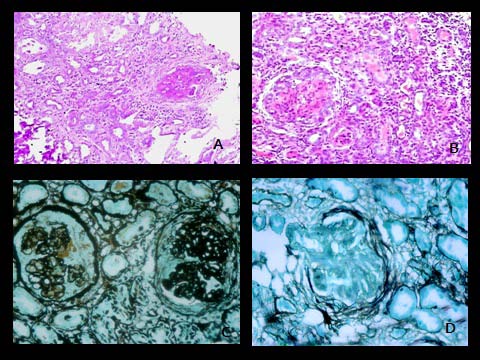
Specimens were subjected to light microscopic studies (with Hematoxylin and Eosin, periodic Schiff, Massons Trichrome and periodic methenamine silver). Autoimmune panel was employed in 79 cases. All the findings were noted and tabulated.
Results Most of the patients who underwent renal biopsy were of nephrotic range proteinuria (40.15%). End stage renal disease (ESRD) was the most common glomerulopathy. Lupus nephritis was the most common secondary glomerulopathy recorded. 12.5 % cases were also seropositive for anti-neutrophilic cytoplasmic antibody (ANCA). Of the clinical symptoms oliguria/anuria with anasarca were the commonest recorded followed by fever, loss of appetite and malaise Conclusion The present study which was truly a clinicopathological study not only adds on to the available Indian literature about spectrum of glomerulopathies in a region of poor human developmental indices but also stresses on the very innocuous sounding symptoms of urinary disturbance and anasarca presenting with fever and weight loss as important pointers towards renal diseases. The finding of ESRD as the most common glomerulopahy in the region done in conjunction with department of pathology and nephrology MLN medical college with SRN hospital, Allahabad, Uttar Pradesh (India). Most of the patients included in the biopsy were of adult age group with very few pediatric samples. The study was conducted after obtaining approval from the ethical committee of the institute. In all the cases informed consent was obtained.
Four per-cutaneous core (specimen) biopsies were retrieved after ultra-sonographic localization of the kidneys in each individual case. The patients complain and complications post procedures were noted.
Specimens were subjected to light microscopic studies (with Hematoxylin and Eosin, periodic Schiff, Massons Trichrome and periodic methenamine silver). Due to economic constraints immunofluoresence studies were done wherever possible. Biopsy samples were considered satisfactory for diagnosis if they contained five or more glomeruli. Biopsies were categorized as inadequate for diagnosis if glomeruli were less than 5. A total of 3 pathologists reviewed and reported the histopathological slides over this period to limit the interpersonal bias. The final diagnoses were then tabulated to ascertain the spectrum of glomerular diseases.
The indications for performing the biopsies were nephrotic syndrome, nephritic syndrome, acute and chronic renal failure of known/unknown etiology, persistent or recurrent asymptomatic hematuria or proteinuria. The biopsies were tabulated according to age, sex, clinical complaints and findings and lab investigation findings (notably urine examination and biochemical examination). The final histopathological diagnoses were then extrapolated on the clinical presentation and laboratory findings for clinicopathological deductions.
Autoimmune panel was employed in 79 cases which included-complement levels (C3/C4), anti nuclear antibody (ANA), double stranded DNA (dsDNA), perinuclear anti neutrophilic cytoplasmic antibody (P-ANCA), cytoplasmic anti neutrophilic cytoplasmic antibody (C-ANCA), anti glomerular basement memberane (Anti-GBM) and cryoglobulins detection.
4. III.
5. Results
6. a) Glomeruolopathy Spectrum
A total of 127 renal biopsies were performed at our centre during the study of which 7 were considered inadequate. There were 86 (67.71%) males and 41 (32.28%) females with male to female ratio being 2:1. The male predominance was virtually present in every lesion except for those seen in lupus nephritis, renal cortical necrosis and in a single recorded case of focal global glomerulosclerosis. The average age of the patients who underwent the procedure was 34 years. (Table -1 The overall complication rate in this study was 2.0%. Local pain at the biopsy site was noted in 1.5% with gross/ microscopic hematuria was noted in 0.5% patients.
Most of the cases who underwent biopsy were of nephrotic range proteinuria (51 patients; 40.15 %) followed by nephritic syndrome (30 patients; 23.62 %) and sub-nephrotic range proteinuria (21 patients; 16.53%). A few cases also underwent renal biopsy having presenting complains of renal failure of uncertain etiology (15 patients; 11.81%) and asymptomatic hematuria (10 patients; 7.87%). (Table -2 Secondary glomerulopathy was found in 19 cases (15.0%); most common pathology was lupus nephritis (4.96%) followed by diabetic nephropathy (4.34%) and amyloid nephropathy (2.48%).
Serological studies concluded that 15 cases (12.5 %) were serologically P-ANCA, C-ANCA or both positive and were categorized as ANCA positive biopsies. P-ANCA positivity accounted for the maximum number of ANCA cases (80.00%) whereas C-ANCA positivity was seen in 13.33% of all ANCA cases. Rest of the cases (20.00%) on serology were showed positivity for both C-ANCA and P-ANCA.
Of all the serologically ANCA positive cases; the maximum number of cases were of end stage renal disease (ESRD) (26.66 %). Focal and segmental mesangial proliferative and crescentic glomerulonephritis without fibrinoid necrosis were the next most common category (20.00 %) followed by necrotizing crescentic glomerulonephritis (13.33 %). Necrotizing glomerulonephritis, focal proliferative and membranous with foci of fibrinoid necrosis were the least commonly seen (6.66 %).(Table -3) Study also recorded the various biochemical and urinary findings in all the cases at the time of the biopsy which are discussed in details according to individual glomerulopathies under Table -
7. Discussion
In the present study, nephrotic range proteinuria, was detected in majority of patients who underwent renal biopsy at our centre. This is comparable to the study by Balakrishnan et al 2 and Narasimhan et al 3 who also reported nephrotic syndrome (proteinuria >3.5 g/24 hr) as the major clinical presentation in Indian adults undergoing renal biopsy.
The predominant primary glomerular pathology in our study was ESRD followed by MGN and MPGN. The present study was conducted in a tertiary care hospital in North Indian state of eastern Uttar Pradesh and hence represents data analysis from this region. This is in contrast to other Indian studies which have recorded MEGN as the commonest injury pattern followed by MGN. 4,5 In a few studies from north India MCD is the commonest recorded injury pattern. 6 Asian studies done in Saudi Arabia and China have reported MPGN as the most common glomerulaopathy followed by FSGS. 7,8,9 The spectrum of glomerular disease is a little different in European and American context where Ig A nephropathy is the most common patern of glomerular injury. 5 Also it was noted in the present study that ESRD was not only the most common injury pattern noted overall but also in the cases of systemic vasculitis.
Thus in contrast to the documented finding of most common histological findings of cresenteric type glomerulonephritis in cases of systemic vasculitis 10 and MEGN in non systemic vasculitis cases by various researchers, diffuse global glomerulosclerosis/ ESRD was the most common histological finding in our group. This in turn points towards a poor socio-economic indicators in patients from in and around north gangectic plains of Allahabad region and reflects delayed presentation and patient ignorance about and complications of renal diseases as a great challenge to nephrologists practising in this region. This is in turn the larger scenario noted in many developing countries of Asia and Africa which are highly resource challenged. The probable reasons for having a different spectrum of renal diseases in different regions of same country and internationally is attributed to the multiple factors such as environmental (infectious as well as noninfectious), human developmental indices, facilities and access to health facilities, degree of health education, presentation of patient in physician OPD to final diagnosis). 11 The second part of study which studied in details the clinical features with renal diseases overall and with specific glomerulopathies also detail presence of urinary disturbances ( anuria/oliguria) and anasarca if presenting with fever and weight loss as the lower most common denominators in screening out all patients who would eventually be diagnosed to be suffering from glomerulopathies.
This becomes important in educating patients as well as physicians as pyuria and hematuria are often thought as red -herrings by both as the features associated with glomerulopathies. But as noted in the study conducted this is often not the case in these patients as despite high urea and creatinine levels and discordance in various other urinary parameters, patients with glomerular diseases present late when only possible therapy is renal replacement either dialysis or renal transpalnation.
Similary very exuberatnt hematuria was noted in renal cortical necrosis and diffuse proliferative glomerulonephritis. Pyuria was seen in cases of secondary glomerulonephritis especially associated with diabetic nephropathy and ESRD. Often in these cases the patients were in higher grade of renal failure with features consistent with those of uremia. In the present study the range of increased urea levels was from 80-210.8 mg/dl with higher values recorded in ESRD. Very high creatinine values were seen in two ends of spectrum of renal failure with an average creatinine value of 7.10 in cases of acute renal failure associated with cresentic glomerulonephritis and chronic renal failure associated with ESRD. These findings are also corroborated with work done previously by various researches. 12,13,14 prompt both the practising physicians and the pathologist in this region to be ever vigilant against a possibility of glomerulopathy in patients attending outpatients so that early action can be initiated to preserve kidney function and to avoid renal replacement therapies which add on to the morbidity and economic burden to the patients. In this regard work by government and non government organization to educate masses in this region can also go a long way to prevent kidney failure and reduce the prevalence of ESRD. Comparing the biochemical and urinary findings with other studies, it was found that nephrotic range proteinuria of 4+ was seen in minimal change disease only with 3+ proteinuria noted in FSGS, ESRD and MeM glomerulonephritis. The proteinuria in rest of the glomerulonephritis was sub-nephritic to minimal.
[Table -3] The present study which was truly a clinicopathological study not only adds on to the available Indian literature about spectrum of glomerulopathies in a region of poor human developmental indices but also stresses on the very innocuous sounding symptoms of urinary disturabce and anasarca presenting with fever and weight loss as important pointers towards renal diseases. The finding of ESRD as the most common glomerulopahy in the region under investigation should 13. Reichert LJM, Koene RAP, Wetzel JFM. Prognostic factors in idiopathic membranous nephropathy. Am J Kidney Dis 1998, 31: 1-11. 14. Schena FP. A retrospective analysis of the natural history of primary Ig A nephropathy worldwide. Am j Med 1990, 89: 209-215.
8. Legends to Figures

| Year 2015 | |||||||||
| ( D D D D ) | SN | GLOMERULONEPHRITIS | TOTAL | % OF ALL | % OF | MALE FEMALE NO.OF | AVG. | ||
| (GLN.) | LESIONS | GLN. | GLO/ | AGE | |||||
| BIOPSY | |||||||||
| 1 | End Stage Renal Disease | ||||||||
| (ESRD) | 21 | 13.04 | 16.53 | 15 | 06 | 12.81 | 37.91 | ||
| 2 | Membranous | 16 | 09.93 | 12.59 | 12 | 04 | 08.50 | 34.75 | |
| 3 | Mesangial Proliferative | 11 | 06.83 | 08.66 | 07 | 04 | 12.08 | 31.77 | |
| 4 | Diffuse Proliferative | 10 | 06.21 | 07.87 | 08 | 02 | 13.22 | 36.66 | |
| 5 | Focal Segmental/ Proliferative | 10 | 06.21 | 07.87 | 07 | 03 | 15.40 | 49.33 | |
| 6 | Membrano Proliferative | ||||||||
| (MPGN) | 08 | 04.96 | 06.29 | 04 | 04 | 13.87 | 27.64 | ||
| 7 | Systemic Lupus | ||||||||
| Erythematosus (SLE) | 08 | 04.96 | 06.29 | 01 | 07 | 14.42 | 33.56 | ||
| 8 | Diabetic Nephropathy | 07 | 04.34 | 05.51 | 04 | 03 | 16.57 | 48.20 | |
| 9 | Focal Segmental | ||||||||
| Glomerulosclerosis (FSGS) | 07 | 04.34 | 05.51 | 06 | 01 | 09.57 | 17.57 | ||
| 10 Inadequate | 07 | 04.34 | 05.51 | 06 | 01 | 00.00 | 34.66 | ||
| 11 Crescentic | 05 | 03.10 | 03.93 | 05 | 00 | 05.80 | 27.00 | ||
| 12 Minimal Change Disease | 05 | 03.10 | 03.93 | 03 | 02 | 08.40 | 14.40 | ||
| 13 Amyloid Nephropathy | 04 | 02.48 | 03.14 | 04 | 00 | 18.75 | 33.75 | ||
| 14 Normal | 03 | 01.86 | 02.36 | 03 | 00 | 03.66 | 37.00 | ||
| 15 Renal Cortical Necrosis | 02 | 01.24 | 01.57 | 00 | 02 | 11.50 | 37.00 | ||
| 16 Benign Nephrosclerosis | 01 | 00.62 | 00.78 | 01 | 00 | 10.00 | 60.00 | ||
| 17 Focal Necrotizing | 01 | 00.62 | 00.78 | 01 | 00 | 04.00 | 60.00 | ||
| 18 Focal Global | |||||||||
| Glomerulosclerosis | 01 | 00.62 | 00.78 | 00 | 01 | 40.00 | 07.00 | ||
| TOTAL | 127 | 78.39 | 87 | 40 | 12.14 | 34.90 | |||
| SN | Indication | Total | Incidence | ||||
| 1 | Nephrotic Syndrome | 51 | 40.15% | ||||
| 2 | Nephritic Syndrome | 30 | 23.62% | ||||
| 3 | Sub-Nephrotic Proteinuria | 21 | 16.53% | ||||
| 4 | Renal Failure of uncertain | 15 | 11.81% | ||||
| etiology | |||||||
| 4 | Asymptomatic hematuria | 10 | 07.87% | ||||
| Of | all | the | glomerulopathies, | primary | |||
| glomerulonephropathy was observed in 108 patients | |||||||
| (85.0%) with end stage renal disease (ESRD) was the | |||||||
| commonest recorded lesion followed by membranous | |||||||
| glomerulonephritis (MGN) and Mesangioproliferative | |||||||
| (MeGN) glomerulonephritis (MPGN) respectively. | |||||||
| (Table-1) | |||||||
| Year 2015 | |||||
| Volume XV Issue 1 Version I | |||||
| D D D D ) C | |||||
| ( | |||||
| SN | AGE | SEX | P-ANCA | C-ANCA | HISTOLOGICAL DIAGNOSIS |
| 1 | 19 | M | + | _ | Crescentic Necrotizing Glomerulonephritis |
| 2 | 25 | M | + | _ | Crescentic Glomerulonephritis |
| 3 | 22 | F | + | _ | End Stage Renal Disease (ESRD) |
| 4 | 35 | F | + | _ | Necrotizing Focal And Segmental |
| Glomerulonephritis | |||||
| 5 | 43 | M | + | _ | Crescentic Necrotizing Glomerulonephritis |
| 6 | 40 | F | + | _ | Necrotizing Focal proliferative Glomerulonephritis |
| 8 | 10 | M | + | + | Focal Necrotizing Glomerulonephritis |
| 9 | 22 | F | _ | + | Necrotizing Focal proliferative glomerulonephritis |
| 10 | 70 | M | + | + | Diffuse Proliferative And Sclerosing |
| Glomerulonephritis (ESRD) | |||||
| 11 | 45 | F | + | _ | End Stage Renal Disease (ESRD) |
| 12 | 42 | M | Diffuse global and Segmental | ||
| Mesangioproliferative glomerulonephritis | |||||
| 13 | 45 | F | + | + | Diffuse Global Glomerular Sclerosis with |
| Advanced Diabetic Glomerulopathy (ESRD) | |||||
| 14 | 21 | M | + | - | Crescentic Glomerulonephritis |
| 15 | 29 | M | - | + | Membranous with foci of fibrinoid change |
| b) Clinico-pathological correlation | symptomswere recorded and later on tabulated | ||||
| A major part of present study dealt with correlation of clinical presentation according to the histopathological diagnosis. All the signs and | according to histopathological diagnosis in 114 cases with detailed patient history and physical examination. (Table-4 and 5) | ||||
| © 2015 Global Journals Inc. (US) | |||||
| Clinical Characteristics and Histopathological Findings in Renal Parenchymal Disease Patients:our | ||||||||||||||||||||||||||
| Single Centre Experience from Northern Plains of India | ||||||||||||||||||||||||||
| MEGN | (n=11) | 06 | (54.5) | 04 | (36.6) | 04 | (36.6) | 02 | (18.1) | - | 05 | (45.5) | - | - | - | 126/ | 86 | |||||||||
| FON | (n=1) | 01 | (100) | 01 | (100) | 01 | (100) | 01 | (100) | - | - | - | - | - | 210/ | 168 | ||||||||||
| FOS | (n=10) | 06 | (60) | 07 | (70) | 04 | (40) | 07 | (70) | 03 | (30) | 09 | (90) | 01 | (10) | 02 | (20) | 01 | (10) | 146/ | 96 | |||||
| FSGS | (n=10) | 04 | (40) | 05 | (50) | 02 | (20) | 06 | (60) | 03 | (30) | 05 | (50) | 01 | (10) | - | - | 142/ | 96 | |||||||
| CGN | (n=5) | 04 | (80) | 05 | (100) | 05 | (100) | 05 | (100) | - | - | 03 | (60) | 03 | (60) | 01 | (20) | 160/ | 100 | |||||||
| LN | (n=8) | 08 | (100) | 06 | (75) | 06 | (75) | 04 | (50) | 03 | (37.5) | 08 | (100) | 03 | (37.5) | - | 01 | (12.5) | 160/ | 100 | ||||||
| DN | (n=7) | 04 | (57.1) | 07 | (100) | - | 07 | (100) | 05 | (71.4) | 06 | (85.7) | 04 | (57.1) | 01 | (14.2) | 04 | (57.1) | 200/ | 120 | ||||||
| MCD | (n=5) | 01 | (20) | 05 | (100) | - | 05 | (100) | - | 02 | (40) | 01 | (20) | - | - | 106/ | 90 | |||||||||
| ESRD | (n=21) | 15 | (71.4) | 21 | (100) | - | 21 | (100) | 21 | (100) | 21 | (100) | 10 | (47.6) | 08 | (38) | 07 | (33.3) | 210/ | 150 | ||||||
| MEM | (n=16) | 02 | (12.5) | 16 | (100) | - | 16 | (100) | - | 11 | (68.7) | - | - | - | 124/ | 96 | ||||||||||
| DPGN | (n=10) | 07 | (70) | 07 | (70) | 08 | (80) | 05 | (50) | 04 | (40) | 08 | (80) | 03 | (30) | 04 | (40) | - | 148/ | 100 | ||||||
| MPGN | (n=8) | 04 | (50) | 02 | (25) | 05 | (62.5) | 07 | (87.5) | 04 | (50) | 06 | (75) | 04 | (50) | - | - | 128/ | 96 | |||||||
| RCN | (n=2) | 01 | (50) | 02 | (100) | - | 02 | (100) | 02 | (100) | 02 | (100) | 02 | (100) | 01 | (50) | 01 | (50) | 110/ | 80 | ||||||
| Fever | Oliguria/ | Anuria | Cola coloured | urine | Anasarca | Persist.nausea, | vomiting >3 | months | Anaemia, | weakness and | malaise | Pain abdomen/ | lump | Altered | sensorium, | confusion and | seizures | Signs of LVF | B.P (Average) | Small joint | pain, alopecia, | rash | ||||
| Glomerulopathies At The Time Of Biopsy | |||||||||||||
| Urine | RCN MPG | DPG | MEM ESR | MC | DN | LN CGN FSGS FO | FON ME | ||||||
| Examination | N | N | D | D | S | GN | |||||||
| CHEMICAL | |||||||||||||
| EXAMINATION | |||||||||||||
| Protein | 2+ | 2+ | 1+ | 3+ | 3+ | 4+ | 1+ | 2+ | 1+ | 3+ | 1+ | 1+ | 2+ |
| Sugar | - | - | - | 1+ | 1+ | - | 3+ | 1+ | 1+ | - | - | - | - |
| MICROSCOPIC | |||||||||||||
| EXAMINATION | |||||||||||||
| Pus cells/hpf | 0-3 | 0-4 | 5-10 | 0-5 | 20-30 | 0-5 | 20- | 5-8 | 5-10 | 1-5 | 1-5 | 1-2 | 1-2 |
| 30 | |||||||||||||
| RBC's /hpf | 40- | 5-10 | 20-50 | 0-3 | 5-10 | 0-2 | 0-3 | 8-10 | 20- | 2-4 | 8-10 | 20- | 5-8 |
| 60 | 30 | 30 | |||||||||||
| Granular | 1-2 | 1-2 | 5-9 | - | - | - | - | 2-5 | 2-3 | - | 1-2 | 1-2 | 2-4 |
| casts/lpf | |||||||||||||
| Hyaline | 5-9 | 1-2 | 1-2 | 2-3 | 5-8 | 1-2 | 1-2 | 2-3 | 3-5 | 2-4 | 1-4 | 2-5 | 2-3 |
| casts/lpf | |||||||||||||
| RBC casts/lpf | 5-9 | 1-2 | 10-20 | - | - | - | - | 2-3 | 8-10 | - | 3-6 | 5-8 | - |
| Broad waxy | - | - | - | - | 5-9 | - | - | - | - | - | - | - | <1 |
| casts/lpf | |||||||||||||
| BIOCHEMICAL | |||||||||||||
| INVESTIGATIONS | |||||||||||||
| Serum Urea | 168.9 | 59.9 | 122.6 | 34.8 | 210.8 | 23.0 | 77.7 78.9 198.9 | 39.9 | 67.8 112.0 80.0 | ||||
| (mg/dl) | |||||||||||||
| Serum | 5.1 | 1.2 | 3.1 | 0.8 | 6.9 | 0.5 | 2.3 | 1.9 | 7.10 | 1.2 | 1.9 | 4.7 | 1.8 |
| Creatinine | |||||||||||||
| (mg/dl) | |||||||||||||
| RCN= Renal cortical necrosis; MPGN= Membranoproliferative glomerulonephritis; DPGN= Diffuse proliferative | |||||||||||||
| glomerulonephritis, MEM= Membranous; ESRD= End stage renal disease; MCD= Minimal change disease; DN= | |||||||||||||
| Diabetic nephropathy; LN= lupus nephritis; CGN= Crescentic glomerulonephritis; FSGS= Focal segmental | |||||||||||||
| glomerulosclerosis; FOS= Focal segmental/proliferative glomerulonephritis; FON= Focal necrotizing | |||||||||||||
| glomerulonephritis; MEGN= mesangioproliferative glomerulonephritis | |||||||||||||
| IV. | |||||||||||||